Health
Mel Gibson Drops Two Medical Bombshells on the Joe Rogan Podcast

From The Vigilant Fox
Being familiar with alternative cancer therapies, Rogan concluded Gibson was talking about antiparasitic drugs Ivermectin and Fenbendazole, which Gibson confirmed with a nod.
In the final hour of episode #2254 of The Joe Rogan Experience, actor Mel Gibson shared two shocking medical experiences that defy mainstream knowledge.
It all started the moment Anthony Fauci’s name lept out of Gibson’s mouth.
“I don’t know why Fauci’s still walking around… or at least free,” Gibson remarked before revealing that he had “road rage” after listening to RFK Jr.’s book about Anthony Fauci.
Piling on, Joe Rogan quickly dismantled any doubts about the book’s accuracy, arguing that if it were full of lies, RFK Jr. would have been sued into the ground and publicly humiliated.
“First of all, people that don’t believe it. How come RFK Jr. didn’t get sued? How come there’s no lawsuits? If there were lies, there would be lawsuits. You’d be publicly humiliated,” Rogan pointed out.
“That book is an accurate depiction of what Anthony Fauci did during the AIDS crisis, which probably was an AZT crisis. It wasn’t an AIDS crisis.”
The first bombshell dropped when Gibson shared that he “couldn’t walk for three months” after taking Fauci’s pet drug for COVID.
“[Remdesivir] kills you. I found out that afterward. And that’s why I wonder about Fauci,” Gibson said.
“Remdesivir is so lethal it got nicknamed ‘Run Death Is Near’ after it started killing thousands of COVID patients in the hospital,” Stella Paul wrote in a previous report.
“The experts claimed that remdesivir would stop COVID; instead, it stopped kidney function, then blasted the liver and other organs.”
Unfortunately, Gibson’s gardener wasn’t as fortunate. After reportedly receiving the kidney-toxic treatment, he tragically passed away.
“I knew the guy for 20 years, and we both went to the same hospital, and he died, and I didn’t,” Gibson lamented. “I think we both got remdesivir, which is not good.”
While you’re here, please take a few seconds to subscribe for more
reports like this one.
The most jaw-dropping moment happened when Gibson made a statement that could threaten the entire cancer industry.
Gibson revealed that he has three friends who had “stage four cancer,” and now “all three of them don’t have cancer right now at all.”
“And they had some serious stuff going on,” Gibson added.
Rogan asked, “What did they take?”—to which Gibson hesitantly replied, “They took what you’ve heard they’ve taken.”
Being familiar with alternative cancer therapies, Rogan concluded Gibson was talking about antiparasitic drugs Ivermectin and Fenbendazole, which Gibson confirmed with a nod.
Corroborating what Gibson reported to Rogan, cancer surgeon Dr. Kathleen Ruddy revealed to The Epoch Times last year that she has seen several late-stage cancer patients make dramatic recoveries after taking Ivermectin.
One patient had a grim future, and then something remarkable happened. This man had stage four prostate cancer and tried all the conventional protocols before doctors told him that there was nothing they could do.
Then, he started taking ivermectin…
Within six months, the metastatic lesions began to disappear, and in less than a year, “he was out dancing for four hours” three nights per week, according to Dr. Ruddy.
A similar scenario unfolded for another man named Eddie. He was also in bad shape.
Eddie was diagnosed with two unresectable esophageal tumors that surgeons wouldn’t go near. He was a smoker, couldn’t swallow, and had lost 40 pounds in a year and a half.
“Within a couple of weeks, he sounded stronger. He could swallow. He had gained six pounds. His voice was better,” reported Dr. Ruddy.
Several weeks later, Dr. Ruddy said to Eddie, “You need to get a scan.”
Guess what happened?
“We got the scan. No tumors. Gone. Gone. The problem was that he had sold his fishing boat. That was the biggest problem. He was getting better. His tumor was gone. Now he’s got to buy another fishing boat … I was like, ‘Well, now, that’s interesting.’”
Recently, anecdotal reports have also praised Fenbendazole as a potentially miraculous anti-cancer drug.
It reportedly works by destabilizing microtubules, the structures that help cancer cells divide and grow.
By disrupting this process, Fenbendazole is believed to effectively halt cancer cell division and slow or stop tumor growth.
A case series published in 2020 documented three cancer patients who experienced complete remission after taking Fenbendazole.
“FBZ (Fenbendazole) appears to be a potentially safe and effective antineoplastic agent that can be repurposed for human use in treating genitourinary malignancies.’”
Adding to the growing evidence in support of Fendendazole’s use case against cancer, an Oklahoma man credited his miraculous cancer recovery to the pet med after overcoming terminal small cell lung cancer, defying a less than 1% survival rate and leaving doctors baffled.
EDMOND, Okla. — When you tell someone a medicine for dogs cured your cancer, you better be ready for some skeptics, but Joe Tippens says it saved his life, and the lives of others.
Now, even cancer researchers are open to the possibility it might be true.
“My stomach, my neck, my liver, my pancreas, my bladder, my bones — it was everywhere,” Tippens said.
Tippens said he was told to go home, call hospice and say his goodbyes two years ago.
The doctors were unanimous, he was going to die of small cell lung cancer.
“Once that kind of cancer goes that far afield, the odds of survival are less than 1 percent, and median life expectancy is three months,” Tippens said.
Tippens said he went from 220 pounds to 110.
“I was a skeleton with skin hanging off of it,” he said. “It was difficult.”
But that was January of 2017. Today, Tippens is very much alive and what he credits for his survival has doctors scratching their heads, and the rest of us raising eyebrows.
“About half the people think I’m just crazy,” he said. “And about half the people want to know more and dig deeper.”
Tippens said he received a tip from a veterinarian, of all people. And in his desperation, he turned from people medicine to dog medicine.
Specifically, something you give your dog when it has worms.
“The truth is stranger than fiction, you know?” Tippens said, laughing.
Just three months later, Tippens says, his cancer was gone.
Thanks for reading! If you enjoyed this post, please do me a quick favor and follow this page (@VigilantFox) for more reports like this one.
Food
Trump says Coca-Cola will switch to real cane sugar in U.S.

Quick Hit:
President Trump announced Wednesday that Coca-Cola will start using real cane sugar in its U.S. beverages, calling the decision “a very good move.” In a Truth Social post, Trump said he had spoken directly with the company and thanked its leadership for the change.
Key Details:
- Trump wrote, “I have been speaking to Coca-Cola about using REAL Cane Sugar in Coke in the United States, and they have agreed to do so.”
- He praised the company’s leadership, saying, “This will be a very good move by them — You’ll see. It’s just better!”
- U.S. Coca-Cola currently uses high fructose corn syrup, unlike versions in Mexico and the UK that use cane sugar.
Diving Deeper:
President Donald Trump on Wednesday said that Coca-Cola is set to bring real cane sugar back into its U.S. soft drinks — a switch many longtime Coke fans have long desired. Posting on Truth Social, Trump wrote: “I have been speaking to Coca-Cola about using REAL Cane Sugar in Coke in the United States, and they have agreed to do so.”
The president continued, “I’d like to thank all of those in authority at Coca-Cola. This will be a very good move by them — You’ll see. It’s just better!”
Coca-Cola has used high fructose corn syrup in the United States since the 1980s, largely due to domestic corn subsidies and the higher cost of imported sugar. However, the cane sugar version — still available in Mexico and much of Europe — remains popular among American consumers, with many saying it offers a cleaner, smoother flavor.
Trump’s comments immediately drew attention both for the policy implication and the personal touch. Though the president is known for his affinity for Diet Coke, which contains no sugar at all, his interest in restoring cane sugar to the classic formula taps into a broader nostalgia many Americans have for pre-1980s Coke.
No formal announcement has yet been made by Coca-Cola itself, and it remains unclear if the reported agreement pertains to all Coke products or specific regional lines. But Trump’s declaration is already generating buzz among fans of the brand and supporters.
(AP Photo/Lynne Sladky)
Addictions
After eight years, Canada still lacks long-term data on safer supply
By Alexandra Keeler
Canada has spent more than $100 million on safer supply programs, but has failed to research their long-term effects
Canada lacks long-term data on safer supply programs, despite funding these programs for years.
Safer supply programs dispense pharmaceutical opioids as a replacement for toxic street drugs.
There is a growing body of research on safer supply’s short-term health effects. But there are no Canadian studies that evaluate program participants’ health impacts beyond 18 months.
The absence of research into long-term data on safer supply means policymakers do not understand how safer supply affects participants’ health, substance use or social outcomes over time.
“Long-term data is important because it helps us understand not just short-term health outcomes like reduced overdoses, but also broader impacts on quality of life, stability and health care use,” said Farihah Ali, scientific lead at the Institute for Mental Health Policy Research at CAMH. The Centre for Addiction and Mental Health is one of Canada’s leading centres for addiction research and clinical care.
Pilot projects
Canada’s first safer supply programs were introduced in Ontario in 2016. Those programs were initially small in scope, intended for a small group of high-risk individuals.
In 2020, the federal government began funding safer supply pilot programs across the country. Provinces are responsible for the delivery and regulation of these programs.
B.C. introduced provincewide programs in 2021. Other provinces, such as Alberta, have restricted safer supply access to a very small number of clinics, and have generally shifted away from harm reduction models in favour of recovery-oriented approaches.
According to the Canadian Public Health Association, an advocacy organization, the original goal for safer supply was to reduce deaths and harms associated with the unregulated toxic drug supply. It was not meant to replace addiction treatment, but to rather act as a bridge to further care.
However, a 2023 report by researchers at McMaster University and Simon Fraser University noted safer supply “does not principally operate toward goals of treatment or recovery.” The report describes safer supply instead as an emergency intervention focused on stabilization and survival.
Evidence gaps
There is a small but growing body of short-term studies on the health effects of Canada’s safer supply programs. Most only track participants’ outcomes for up to 12 months.
Some of those studies suggest safer supply may reduce the immediate harms associated with drug use.
A 2024 study found a 91 per cent reduction in the risk of death among high-risk individuals receiving safer supply in B.C. Critics have raised concerns about the study’s methodology, sample size and confounding variables.
In contrast, a March study suggested B.C.’s safer supply and decriminalization policies may be associated with increased hospitalizations. These findings also sparked controversy, with experts debating how well the data isolate causal impacts.
And a comparative study released in April also showed some positive outcomes from safer supply. It too sparked significant expert debate.
‘Arms-length’
Of all the provinces, B.C. has implemented safer supply most broadly. The province’s health ministry did not directly respond when asked about the long-term goals of its safer supply program, or whether B.C. collects longitudinal data on program participants’ health outcomes.
“Evidence shows [safer supply] helps separate people from the unregulated drug supply, manage their substance use and withdrawal symptoms with regulated medications, and helps connect them to voluntary health and social supports,” a Ministry of Health spokesperson told Canadian Affairs in an email.
The ministry did not provide the evidence it referenced.
At the federal level, Health Canada confirmed that, to date, it has funded just two evaluations of safer supply programs, despite spending more than $100 million on safer supply since April 2023.
The first was a short-term study, funded by the federal government’s Substance Use and Addictions Program program. Conducted over four months, that study assessed 10 safer supply programs in Ontario, B.C., and New Brunswick. It documented initial impacts on participants’ lives and program delivery, primarily through qualitative methods such as interviews and surveys.
The second study is an ongoing, “arms-length evaluation” of 11 safer supply pilot programs funded by the Canadian Institutes of Health Research (CIHR), Canada’s federal health research agency.
When asked about long-term research on safer supply, Health Canada referred Canadian Affairs to a 2022 funding announcement about this multi-year evaluation. While the evaluation is being conducted over several years, it is unclear if it includes long-term tracking of patients’ outcomes.
Barriers and resistance
There are a number of factors that make it challenging to evaluate safer supply programs over long periods.
Ali, of CAMH, says unstable, short-term funding can disrupt long-term research.
“When programs are shut down or scaled back, we lose contact with participants and the ability to track outcomes over time,” she said.
Program participants can also be difficult to track over long periods, she says. Many struggle with housing insecurity, health instability and criminalization.
Frontline staff also face burnout and high turnover, she says, limiting support for such research activities.
Additionally, there are tradeoffs between the anonymity needed to encourage patients to access safer supply programs and the ability to collect detailed data.
“Ethical concerns — like not wanting to burden participants or risk their safety or confidentiality — require us to design studies that are trauma-informed and flexible, which adds complexity to long-term data collection,” Ali said.
Julian Somers, a clinical psychologist and professor at Simon Fraser University, says B.C.’s failure to conduct long-term evaluations of its safer supply programs is not just an oversight, but an act of negligence.
“B.C. has some of the best pharmaceutical data systems in the world,” Somers said, referring to PharmaCare and PharmaNet — databases that capture every prescription drug transaction in the province.
Somers says his team previously used PharmaNet data to examine prescribed opioids’ effects on health and social outcomes. In 2017, he proposed a long-term safer supply evaluation using these tools.
In 2017, he proposed a long-term evaluation of B.C.’s safer supply programs.
The province declined.
According to Ali, “Future research should explore how safer supply impacts people’s long-term health, stability and connection to care.”
“We also need to listen to people’s experiences, how safer supply affects their daily lives, their sense of dignity, and their relationships with care providers through qualitative mechanisms.”
This article was produced through the Breaking Needles Fellowship Program, which provided a grant to Canadian Affairs, a digital media outlet, to fund journalism exploring addiction and crime in Canada. Articles produced through the Fellowship are co-published by Break The Needle and Canadian Affairs.
-
 COVID-192 days ago
COVID-192 days agoSen. Rand Paul: ‘I am officially re-referring Dr. Fauci to the DOJ’
-
 International2 days ago
International2 days agoMatt Walsh slams Trump administration’s move to bury Epstein sex trafficking scandal
-

 National2 days ago
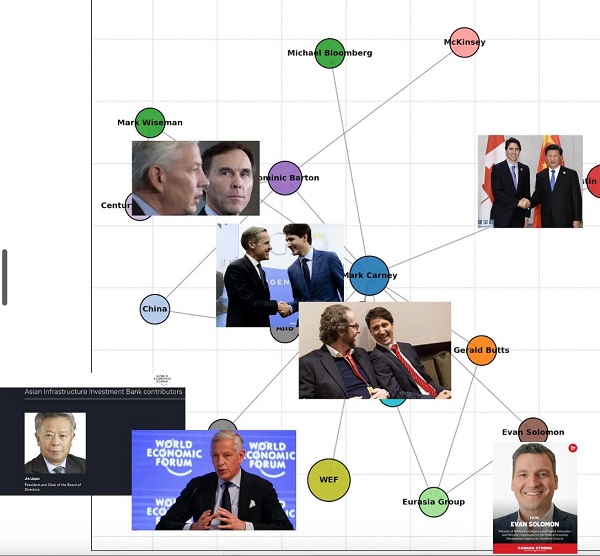
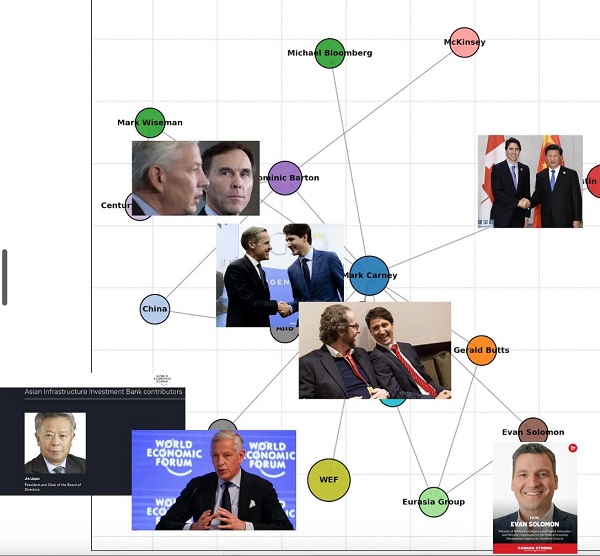
National2 days agoDemocracy Watch Blows the Whistle on Carney’s Ethics Sham
-

 Energy1 day ago
Energy1 day agoIs The Carney Government Making Canadian Energy More “Investible”?
-

 John Stossel2 days ago
John Stossel2 days agoThe Green Industrial Complex: Power, Panic, and Profits
-

 Business1 day ago
Business1 day agoCompetition Bureau is right—Canada should open up competition in the air
-

 Immigration1 day ago
Immigration1 day agoUnregulated medical procedures? Price Edward Islanders Want Answers After Finding Biomedical Waste From PRC-Linked Monasteries
-
 Business1 day ago
Business1 day agoDemocracy Watchdog Says PM Carney’s “Ethics Screen” Actually “Hides His Participation” In Conflicted Investments