Alberta
Health Care Overhaul: AHS to be laser focused on Acute Care and Continuing Care outcomes
Refocusing on patient-centred care
A refocused health care system will improve health outcomes for Albertans and empower health care workers to deliver quality care across the province.
Alberta’s front-line health workers provide exceptional care to patients and families, and Alberta’s government is committed to supporting their work by providing a high-functioning health care system. Alberta’s government has been working to address wait times and health care service disruptions, but challenges still exist in the system, including accessing community care like family doctors and local health services. The current health care system’s structure limits the government’s ability to provide system-wide oversight, set system priorities, and to require accountability for those priorities on behalf of Albertans.
To overcome current challenges and deliver the right care for Albertans at the right time, Alberta is refocusing the health care system. These changes will focus on the priority sectors of primary care, acute care, continuing care and mental health and addiction to ensure Albertans receive the best care within a single, fully integrated, high-functioning system.
These changes will improve front-line service delivery, and front-line jobs will be protected during this transition. Albertans will continue to access health care services where they regularly receive their care during the system’s transition period and beyond.
“Albertans deserve access to the health care they need, when and where they need it. Health care workers move mountains for their patients every day. For too many years, Alberta’s health care system has been too complex and uncoordinated, leading to unacceptable wait times and poorer health outcomes for Albertans. It’s time to change that. It’s time to put Albertans first in every health care decision and give our front-line experts the right space to properly care for Albertans. This is why we are refocusing the health system to provide better care for generations of Albertans to come.”
“We are at a critical juncture when it comes to health care in Alberta. We need to refocus how the system is structured and create a path forward that will get us the outcomes Albertans deserve. This work will take time and it will not be easy. We will lean on the world-class talent and expertise that exists in our health care system every step of the way. I ask health care workers to join us on this important journey so they can work in a better system – for them and for their patients.”
“Minister LaGrange has acknowledged that our health care system needs urgent reform. This work will only succeed with the involvement and leadership of physicians. The AMA looks forward to meaningful consultation and collaboration as these reforms are further elaborated.”
Alberta
‘Far too serious for such uninformed, careless journalism’: Complaint filed against Globe and Mail article challenging Alberta’s gender surgery law
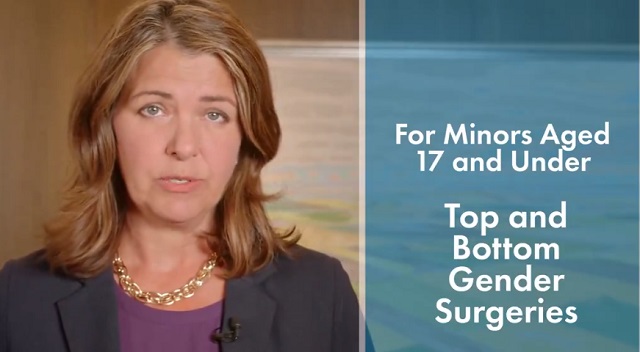
Macdonald Laurier Institute challenges Globe article on gender medicine
The complaint, now endorsed by 41 physicians, was filed in response to an article about Alberta’s law restricting gender surgery and hormones for minors.
On June 9, the Macdonald-Laurier Institute submitted a formal complaint to The Globe and Mail regarding its May 29 Morning Update by Danielle Groen, which reported on the Canadian Medical Association’s legal challenge to Alberta’s Bill 26.
Written by MLI Senior Fellow Mia Hughes and signed by 34 Canadian medical professionals at the time of submission to the Globe, the complaint stated that the Morning Update was misleading, ideologically slanted, and in violation the Globe’s own editorial standards of accuracy, fairness, and balance. It objected to the article’s repetition of discredited claims—that puberty blockers are reversible, that they “buy time to think,” and that denying access could lead to suicide—all assertions that have been thoroughly debunked in recent years.
Given the article’s reliance on the World Professional Association for Transgender Health (WPATH), the complaint detailed the collapse of WPATH’s credibility, citing unsealed discovery documents from an Alabama court case and the Cass Review’s conclusion that WPATH’s guidelines—and those based on them—lack developmental rigour. It also noted the newsletter’s failure to mention the growing international shift away from paediatric medical transition in countries such as the UK, Sweden, and Finland. MLI called for the article to be corrected and urged the Globe to uphold its commitment to balanced, evidence-based journalism on this critical issue.
On June 18, Globe and Mail Standards Editor Sandra Martin responded, defending the article as a brief summary that provided a variety of links to offer further context. However, the three Globe and Mail news stories linked to in the article likewise lacked the necessary balance and context. Martin also pointed to a Canadian Paediatric Society (CPS) statement linked to in the newsletter. She argued it provided “sufficient context and qualification”—despite the fact that the CPS itself relies on WPATH’s discredited guidelines. Notwithstanding, Martin claimed the article met editorial standards and that brevity justified the lack of balance.
MLI responded that brevity does not excuse misinformation, particularly on a matter as serious as paediatric medical care, and reiterated the need for the Globe to address the scientific inaccuracies directly. MLI again called for the article to be corrected and for the unsupported suicide claim to be removed. As of this writing, the Globe has not responded.
Letter of complaint
June 9, 2025
To: The Globe and Mail
Attn: Sandra Martin, standards editor
CC: Caroline Alphonso, health editor; Mark Iype, deputy national editor and Alberta bureau chief
To the editors;
Your May 29 Morning Update: The Politics of Care by Danielle Groen, covering the Canadian Medical Association’s legal challenge to Alberta’s Bill 26, was misleading and ideologically slanted. It is journalistically irresponsible to report on contested medical claims as undisputed fact.
This issue is far too serious for such uninformed, careless journalism lacking vital perspectives and scientific context. At stake is the health and future of vulnerable children, and your reporting risks misleading parents into consenting to irreversible interventions based on misinformation.
According to The Globe and Mail’s own Journalistic Principles outlined in its Editorial Code of Conduct, the credibility of your reporting rests on “solid research, clear, intelligent writing, and maintaining a reputation for honesty, accuracy, fairness, balance and transparency.” Moreover, your principles go on to state that The Globe will “seek to provide reasonable accounts of competing views in any controversy.” The May 29 update violated these principles. There is, as I will show, a widely available body of scientific information that directly contests the claims and perspectives presented in your article. Yet this information is completely absent from your reporting.
The collapse of WPATH’s credibility
The article’s claim that Alberta’s law “falls well outside established medical practice” and could pose the “greatest threat” to transgender youth is both false and inflammatory. There is no global medical consensus on how to treat gender-distressed young people. In fact, in North America, guidelines are based on the Standards of Care developed by the World Professional Association for Transgender Health (WPATH)—an organization now indisputably shown to place ideology above evidence.
For example, in a U.S. legal case over Alabama’s youth transition ban, WPATH was forced to disclose over two million internal emails. These revealed the organization commissioned independent evidence reviews for its latest Standards of Care (SOC8)—then suppressed those reviews when they found overwhelmingly low-quality evidence. Yet WPATH proceeded to publish the SOC8 as if it were evidence-based. This is not science. It is fraudulent and unethical conduct.
These emails also showed Admiral Rachel Levine—then-assistant secretary for Health in the Biden administration—pressured WPATH to remove all lower age recommendations from the guidelines—not on scientific grounds, but to avoid undermining ongoing legal cases at the state level. This is politics, not sound medical practice.
The U.K.’s Cass Review, a major multi-year investigation, included a systematic review of the guidelines in gender medicine. A systematic review is considered the gold standard because it assesses and synthesizes all the available research in a field, thereby reducing bias and providing a large comprehensive set of data upon which to reach findings. The systematic review of gender medicine guidelines concluded that WPATH’s standards of care “lack developmental rigour” and should not be used as a basis for clinical practice. The Cass Review also exposed citation laundering where medical associations endlessly recycled weak evidence across interlocking guidelines to fabricate a false consensus. This led Cass to suggest that “the circularity of this approach may explain why there has been an apparent consensus on key areas of practice despite the evidence being poor.”
Countries like Sweden, Finland, and the U.K. have now abandoned WPATH and limited or halted medicalized youth transitions in favour of a therapy-first approach. In Norway, UKOM, an independent government health agency, has made similar recommendations. This shows the direction of global practice is moving away from WPATH’s medicalized approach—not toward it. As part of any serious effort to “provide reasonable accounts of competing views,” your reporting should acknowledge these developments.
Any journalist who cites WPATH as a credible authority on paediatric gender medicine—especially in the absence of contextualizing or competing views—signals a lack of due diligence and a fundamental misunderstanding of the field. It demonstrates that either no independent research was undertaken, or it was ignored despite your editorial standards.
Puberty blockers don’t ‘buy time’ and are not reversible
Your article repeats a widely debunked claim: that puberty blockers are a harmless pause to allow young people time to explore their identity. In fact, studies have consistently shown that between 98 per cent and 100 per cent of children placed on puberty blockers go on to take cross-sex hormones. Before puberty blockers, most children desisted and reconciled with their birth sex during or after puberty. Now, virtually none do.
This strongly suggests that blocking puberty in fact prevents the natural resolution of gender distress. Therefore, the most accurate and up-to-date understanding is that puberty blockers function not as a pause, but as the first step in a treatment continuum involving irreversible cross-sex hormones. Indeed, a 2022 paper found that while puberty suppression had been “justified by claims that it was reversible … these claims are increasingly implausible.” Again, adherence to the Globe’s own editorial guidelines would require, at minimum, the acknowledgement of the above findings alongside the claims your May 29 article makes.
Moreover, it is categorically false to describe puberty blockers as “completely reversible.” Besides locking youth into a pathway of further medicalization, puberty blockers pose serious physical risks: loss of bone density, impaired sexual development, stunted fertility, and psychosocial harm from being developmentally out of sync with peers. There are no long-term safety studies. These drugs are being prescribed to children despite glaring gaps in our understanding of their long-term effects.
Given the Globe’s stated editorial commitment to principles such as “accuracy,” the crucial information from the studies linked above should be provided in any article discussing puberty blockers. At a bare minimum, in adherence to the Globe’s commitment to “balance,” this information should be included alongside the contentious and disputed claims the article makes that these treatments are reversible.
No proof of suicide prevention
The most irresponsible and dangerous claim in your article is that denying access to puberty blockers could lead to “depression, self-harm and suicide.” There is no robust evidence supporting this transition-or-suicide narrative, and in fact, the findings of the highest-quality study conducted to date found no evidence that puberty suppression reduces suicide risk.
Suicide is complex and attributing it to a single cause is not only false—it violates all established suicide reporting guidelines. Sensationalized claims like this risk creating contagion effects and fuelling panic. In the public interest, reporting on the topic of suicide must be held to the most rigorous standards, and provide the most high-quality and accurate information.
Euphemism hides medical harm
Your use of euphemistic language obscures the extreme nature of the medical interventions being performed in gender clinics. Calling double mastectomies for teenage girls “paediatric breast surgeries for gender-affirming reasons” sanitizes the medically unnecessary removal of a child’s healthy organs. Referring to phalloplasty and vaginoplasty as “gender-affirming surgeries on lower body parts” conceals the fact that these are extreme operations involving permanent disfigurement, high complication rates, and often requiring multiple revisions.
Honest journalism should not hide these facts behind comforting language. Your reporting denies youth, their parents, and the general public the necessary information to understand the nature of these interventions. Members of the general public rely greatly on the news media to equip them with such information, and your own editorial standards claim you will fulfill this core responsibility.
Your responsibility to the public
As a flagship Canadian news outlet, your responsibility is not to amplify activist messaging, but to report the truth with integrity. On a subject as medically and ethically fraught as paediatric gender medicine, accuracy is not optional. The public depends on you to scrutinize claims, not echo ideology. Parents may make irreversible decisions on behalf of their children based on the narratives you promote. When reporting is false or ideologically distorted, the cost is measured in real-world harm to some of our society’s most vulnerable young people.
I encourage the Globe and Mail to publish an updated version on this article in order to correct the public record with the relevant information discussed above, and to modify your reporting practices on this matter going forward—by meeting your own journalistic standards—so that the public receives balanced, correct, and reliable information on this vital topic.
Trustworthy journalism is a cornerstone of public health—and on the issue of paediatric gender medicine, the stakes could not be higher.
Sincerely,
Mia Hughes
Senior Fellow, Macdonald-Laurier Institute
Author of The WPATH Files
The following 41 physicians have signed to endorse this letter:
Dr. Mike Ackermann, MD
Dr. Duncan Veasey, Psy MD
Dr. Rick Gibson, MD
Dr. Benjamin Turner, MD, FRCSC
Dr. J.N. Mahy, MD, FRCSC, FACS
Dr. Khai T. Phan, MD, CCFP
Dr. Martha Fulford, MD
Dr. J. Edward Les, MD, FRCPC
Dr. Darrell Palmer, MD, FRCPC
Dr. Jane Cassie, MD, FRCPC
Dr. David Lowen, MD, FCFP
Dr. Shawn Whatley, MD, FCFP (EM)
Dr. David Zitner, MD
Dr. Leonora Regenstreif, MD, CCFP(AM), FCFP
Dr. Gregory Chan, MD
Dr. Alanna Fitzpatrick, MD, FRCSC
Dr. Chris Millburn, MD, CCFP
Dr. Julie Curwin, MD, FRCPC
Dr. Roy Eappen, MD, MDCM, FRCP (c)
Dr. York N. Hsiang, MD, FRCSC
Dr. Dion Davidson, MD, FRCSC, FACS
Dr. Kevin Sclater, MD, CCFP (PC)
Dr. Theresa Szezepaniak, MB, ChB, DRCOG
Dr. Sofia Bayfield, MD, CCFP
Dr. Elizabeth Henry, MD, CCFP
Dr. Stephen Malthouse, MD
Dr. Darrell Hamm, MD, CCFP
Dr. Dale Classen, MD, FRCSC
Dr. Adam T. Gorner, MD, CCFP
Dr. Wesley B. Steed, MD
Dr. Timothy Ehmann, MD, FRCPC
Dr. Ryan Torrie, MD
Dr. Zachary Heinricks, MD, CCFP
Dr. Jessica Shintani, MD, CCFP
Dr. Mark D’Souza, MD, CCFP(EM), FCFP*
Dr. Joanne Sinai, MD, FRCPC*
Dr. Jane Batt, MD*
Dr. Brent McGrath, MD, FRCPC*
Dr. Leslie MacMillan MD FRCPC (emeritus)*
Dr. Ian Mitchell, MD, FRCPC*
Dr. John Cunnington, MD
*Indicates physician who signed following the letter’s June 9 submission to the Globe and Mail, but in advance of this letter being published on the MLI website.
Alberta
COWBOY UP! Pierre Poilievre Promises to Fight for Oil and Gas, a Stronger Military and the Interests of Western Canada

Fr0m Energy Now
As Calgarians take a break from the incessant news of tariff threat deadlines and global economic challenges to celebrate the annual Stampede, Conservative party leader Pierre Poilievre gave them even more to celebrate.
Poilievre returned to Calgary, his hometown, to outline his plan to amplify the legitimate demands of Western Canada and not only fight for oil and gas, but also fight for the interests of farmers, for low taxes, for decentralization, a stronger military and a smaller federal government.
Speaking at the annual Conservative party BBQ at Heritage Park in Calgary (a place Poilievre often visited on school trips growing up), he was reminded of the challenges his family experienced during the years when Trudeau senior was Prime Minister and the disastrous effect of his economic policies.
“I was born in ’79,” Poilievre said. “and only a few years later, Pierre Elliott Trudeau would attack our province with the National Energy Program. There are still a few that remember it. At the same time, he hammered the entire country with money printing deficits that gave us the worst inflation and interest rates in our history. Our family actually lost our home, and we had to scrimp and save and get help from extended family in order to get our little place in Shaughnessy, which my mother still lives in.”
This very personal story resonated with many in the crowd who are now experiencing an affordability crisis that leaves families struggling and young adults unable to afford their first house or condo. Poilievre said that the experience was a powerful motivator for his entry into politics. He wasted no time in proposing a solution – build alliances with other provinces with mutual interests, and he emphasized the importance of advocating for provincial needs.
“Let’s build an alliance with British Columbians who want to ship liquefied natural gas out of the Pacific Coast to Asia, and with Saskatchewanians, Newfoundlanders and Labradorians who want to develop their oil and gas and aren’t interested in having anyone in Ottawa cap how much they can produce. Let’s build alliances with Manitobans who want to ship oil in the port of Churchill… with Quebec and other provinces that want to decentralize our country and get Ottawa out of our business so that provinces and people can make their own decisions.”
Poilievre heavily criticized the federal government’s spending and policies of the last decade, including the increase in government costs, and he highlighted the negative impact of those policies on economic stability and warned of the dangers of high inflation and debt. He advocated strongly for a free-market economy, advocating for less government intervention, where businesses compete to impress customers rather than impress politicians. He also addressed the decade-long practice of blocking and then subsidizing certain industries. Poilievre referred to a famous quote from Ronald Reagan as the modus operandi of the current federal regime.
“The Government’s view of the economy could be summed up in a few short phrases. If anything moves, tax it. If it keeps moving, regulate it. And if it stops moving, subsidize it.”
The practice of blocking and then subsidizing is merely a ploy to grab power, according to Poilievre, making industry far too reliant on government control.
“By blocking you from doing something and then making you ask the government to help you do it, it makes you reliant. It puts them at the center of all power, and that is their mission…a full government takeover of our economy. There’s a core difference between an economy controlled by the government and one controlled by the free market. Businesses have to clamour to please politicians and bureaucrats. In a free market (which we favour), businesses clamour to impress customers. The idea is to put people in charge of their economic lives by letting them have free exchange of work for wages, product for payment and investment for interest.”
Poilievre also said he plans to oppose any ban on gas-powered vehicles, saying, “You should be in the driver’s seat and have the freedom to decide.” This is in reference to the Trudeau-era plan to ban the sale of gas-powered cars by 2035, which the Carney government has said they have no intention to change, even though automakers are indicating that the targets cannot be met. He also intends to oppose the Industrial Carbon tax, Bill C-69 the Impact Assessment Act, Bill C-48 the Oil tanker ban, the proposed emissions cap which will cap energy production, as well as the single-use plastics ban and Bill C-11, also known as the Online Streaming Act and the proposed “Online Harms Act,” also known as Bill C-63. Poilievre closed with rallying thoughts that had a distinctive Western flavour.
“Fighting for these values is never easy. Change, as we’ve seen, is not easy. Nothing worth doing is easy… Making Alberta was hard. Making Canada, the country we love, was even harder. But we don’t back down, and we don’t run away. When things get hard, we dust ourselves off, we get back in the saddle, and we gallop forward to the fight.”
Cowboy up, Mr. Poilievre.
Maureen McCall is an energy professional who writes on issues affecting the energy industry.
-

 COVID-192 days ago
COVID-192 days agoFDA requires new warning on mRNA COVID shots due to heart damage in young men
-

 Indigenous2 days ago
Indigenous2 days agoInternal emails show Canadian gov’t doubted ‘mass graves’ narrative but went along with it
-
 Business2 days ago
Business2 days agoCarney’s new agenda faces old Canadian problems
-

 Bruce Dowbiggin2 days ago
Bruce Dowbiggin2 days agoEau Canada! Join Us In An Inclusive New National Anthem
-

 Alberta2 days ago
Alberta2 days agoCOWBOY UP! Pierre Poilievre Promises to Fight for Oil and Gas, a Stronger Military and the Interests of Western Canada
-

 International1 day ago
International1 day agoChicago suburb purchases childhood home of Pope Leo XIV
-

 Daily Caller1 day ago
Daily Caller1 day agoBlackouts Coming If America Continues With Biden-Era Green Frenzy, Trump Admin Warns
-
 Daily Caller1 day ago
Daily Caller1 day ago‘I Know How These People Operate’: Fmr CIA Officer Calls BS On FBI’s New Epstein Intel