Health
Doctor withholds results of study that fails to show transitioning improves kids’ health
From LifeSiteNews
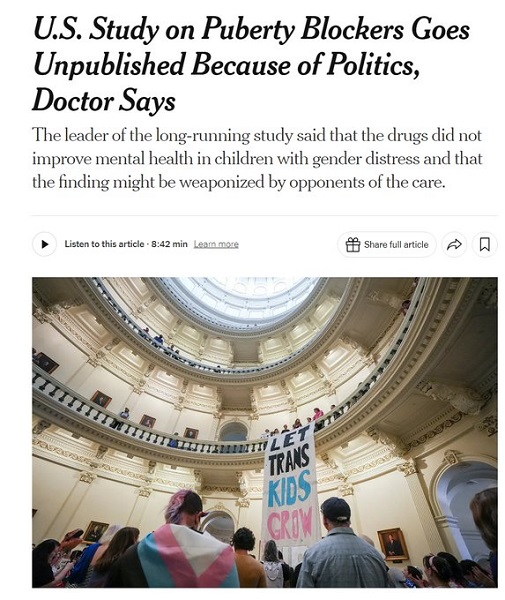
A prominent doctor has been refusing to release the findings of a federally funded “transgender youth” study she began in 2015 because the results did not match the conclusions she hoped for, according to an explosive report in The New York Times.
The Times reported that Johanna Olson-Kennedy, medical director of the Center for Trans Youth Health & Development at Children’s Hospital in Los Angeles, “recruited 95 children from across the country and gave them puberty blockers,” then “followed the children for two years to see if the treatments improved their mental health.” She told the National Institutes of Health (NIH) that she expected to find that the kids would show “decreased symptoms of depression, anxiety, trauma symptoms, self-injury, and suicidality, and increased body esteem and quality of life over time.”
However, the study did not show the children doing better than they started. “Before receiving the drugs, around one-quarter of the group reported depression symptoms and significant anxiety, and one quarter reported ever having thoughts of suicide,” the Times says. “Eight percent reported a past suicide attempt.”
In an interview with the Times, Olson-Kennedy attempted to argue that the children’s starting point actually wasn’t so bad after all, and therefore the lack of change was not concerning: “They’re in really good shape when they come in, and they’re in really good shape after two years.” On follow-up, she claimed her “good shape” comment was referring to data averages, and her conclusion about the full data was still pending.
Regardless, in the nine years since the study commenced, Olson-Kennedy has still yet to publish any of the data for outside observers to analyze for themselves, which she justified by claiming, “I do not want our work to be weaponized. It has to be exactly on point, clear and concise. And that takes time.”
NEW: Azeen Ghorayshi reports in the @nytimes that prominent gender clinician Johanna Olson-Kennedy of @ChildrensLA has refused to publish data from a study on puberty blockers, fearing that the unimpressive results will be "weaponized" by critics of "gender-affirming care." 🧵 pic.twitter.com/DREXSNsFYk
— Leor Sapir (@LeorSapir) October 23, 2024
https://t.co/st0O6ox763 https://t.co/WZbnXv6DO2
— Leor Sapir (@LeorSapir) October 23, 2024
A significant body of evidence shows that “affirming” gender confusion carries serious harms, especially when done with impressionable children who lack the mental development, emotional maturity, and life experience to consider the long-term ramifications of the decisions being pushed on them, or full knowledge about the long-term effects of life-altering, physically transformative, and often-irreversible surgical and chemical procedures.
Studies find that more than 80% of children experiencing gender dysphoria outgrow it on their own by late adolescence, and that even full “reassignment” surgery often fails to resolve gender-confused individuals’ heightened tendency to engage in self-harm and suicide — and may even exacerbate it, including by reinforcing their confusion and neglecting the actual root causes of their mental strife.
Many oft-ignored “detransitioners,” individuals who attempted to live under a different “gender identity” before embracing their sex, attest to the physical and mental harm of reinforcing gender confusion as well as to the bias and negligence of the medical establishment on the subject, many of whom take an activist approach to their profession and begin cases with a predetermined conclusion that “transitioning” is the best solution.
“Gender-affirming” physicians have also been caught on video admitting to more old-fashioned motives for such procedures, as with a 2022 exposé about Vanderbilt University Medical Center’s Clinic for Transgender Health, where Dr. Shayne Sebold Taylor said outright that “these surgeries make a lot of money.”
In December, the U.S. Supreme Court will begin considering arguments about the permissibility of state laws prohibiting the gender “transitioning”” of minors.
Business
Cutting Red Tape Could Help Solve Canada’s Doctor Crisis

From the Frontier Centre for Public Policy
By Ian Madsen
Doctors waste millions of hours on useless admin. It’s enough to end Canada’s doctor shortage. Ian Madsen says slashing red tape, not just recruiting, is the fastest fix for the clogged system.
Doctors spend more time on paperwork than on patients and that’s fueling Canada’s health care wait lists
Canada doesn’t just lack doctors—it squanders the ones it has. Mountains of paperwork and pointless admin chew up tens of millions of physician hours every year, time that could erase the so-called shortage and slash wait lists if freed for patient care.
Recruiting more doctors helps, but the fastest cure for our sick system is cutting the bureaucracy that strangles the ones already here.
The Canadian Medical Association found that unnecessary non-patient work consumes millions of hours annually. That’s the equivalent of 50.5 million patient visits, enough to give every Canadian at least one appointment and likely erase the physician shortage. Meanwhile, the Canadian Institute for Health Information estimates more than six million Canadians don’t even have a family doctor. That’s roughly one in six of us.
And it’s not just patients who feel the shortage—doctors themselves are paying the price. Endless forms don’t just waste time; they drive doctors out of the profession. Burned out and frustrated, many cut their hours or leave entirely. And the foreign doctors that health authorities are trying to recruit? They might think twice once they discover how much time Canadian physicians spend on paperwork that adds nothing to patient care.
But freeing doctors from forms isn’t as simple as shredding them. Someone has to build systems that reduce, rather than add to, the workload. And that’s where things get tricky. Trimming red tape usually means more Information Technology (IT), and big software projects have a well-earned reputation for spiralling in cost.
Bent Flyvbjerg, the global guru of project disasters, and his colleagues examined more than 5,000 IT projects in a 2022 study. They found outcomes didn’t follow a neat bell curve but a “power-law” distribution, meaning costs don’t just rise steadily, they explode in a fat tail of nasty surprises as variables multiply.
Oxford University and McKinsey offered equally bleak news. Their joint study concluded: “On average, large IT projects run 45 per cent over budget and seven per cent over time while delivering 56 per cent less value than predicted.” If that sounds familiar, it should. Canada’s Phoenix federal payroll fiasco—the payroll software introduced by Ottawa that left tens of thousands of federal workers underpaid or unpaid—is a cautionary tale etched into the national memory.
The lesson isn’t to avoid technology, but to get it right. Canada can’t sidestep the digital route. The question is whether we adapt what others have built or design our own. One option is borrowing from the U.S. or U.K., where electronic health record (EHR) systems (the digital patient files used by doctors and hospitals) are already in place. Both countries have had headaches with their systems, thanks to legal and regulatory differences. But there are signs of progress.
The U.K. is experimenting with artificial intelligence to lighten the administrative load, and a joint U.K.-U.S. study gives a glimpse of what’s possible:
“… AI technologies such as Robotic Process Automation (RPA), predictive analytics, and Natural Language Processing (NLP) are transforming health care administration. RPA and AI-driven software applications are revolutionizing health care administration by automating routine tasks such as appointment scheduling, billing, and documentation. By handling repetitive, rule-based tasks with speed and accuracy, these technologies minimize errors, reduce administrative burden, and enhance overall operational efficiency.”
For patients, that could mean fewer missed referrals, faster follow-up calls and less time waiting for paperwork to clear before treatment. Still, even the best tools come with limits. Systems differ, and customization will drive up costs. But medicine is medicine, and AI tools can bridge more gaps than you might think.
Run the math. If each “freed” patient visit is worth just $20—a conservative figure for the value of a basic appointment—the payoff could hit $1 billion in a single year.
Updating costs would continue, but that’s still cheap compared to the human and financial toll of endless wait lists. Cost-sharing between provinces, Ottawa, municipalities and even doctors themselves could spread the risk. Competitive bidding, with honest budgets and realistic timelines, is non-negotiable if we want to dodge another Phoenix-sized fiasco.
The alternative—clinging to our current dysfunctional patchwork of physician information systems—isn’t really an option. It means more frustrated doctors walking away, fewer new ones coming in, and Canadians left to languish on wait lists that grow ever longer.
And that’s not health care—it’s managed decline.
Ian Madsen is a senior policy analyst at the Frontier Centre for Public Policy.
Addictions
BC premier admits decriminalizing drugs was ‘not the right policy’

From LifeSiteNews
Premier David Eby acknowledged that British Columbia’s liberal policy on hard drugs ‘became was a permissive structure that … resulted in really unhappy consequences.’
The Premier of Canada’s most drug-permissive province admitted that allowing the decriminalization of hard drugs in British Columbia via a federal pilot program was a mistake.
Speaking at a luncheon organized by the Urban Development Institute last week in Vancouver, British Columbia, Premier David Eby said, “I was wrong … it was not the right policy.”
Eby said that allowing hard drug users not to be fined for possession was “not the right policy.
“What it became was a permissive structure that … resulted in really unhappy consequences,” he noted, as captured by Western Standard’s Jarryd Jäger.
LifeSiteNews reported that the British Columbia government decided to stop a so-called “safe supply” free drug program in light of a report revealing many of the hard drugs distributed via pharmacies were resold on the black market.
Last year, the Liberal government was forced to end a three-year drug decriminalizing experiment, the brainchild of former Prime Minister Justin Trudeau’s government, in British Columbia that allowed people to have small amounts of cocaine and other hard drugs. However, public complaints about social disorder went through the roof during the experiment.
This is not the first time that Eby has admitted he was wrong.
Trudeau’s loose drug initiatives were deemed such a disaster in British Columbia that Eby’s government asked Trudeau to re-criminalize narcotic use in public spaces, a request that was granted.
Records show that the Liberal government has spent approximately $820 million from 2017 to 2022 on its Canadian Drugs and Substances Strategy. However, even Canada’s own Department of Health in a 2023 report admitted that the Liberals’ drug program only had “minimal” results.
Official figures show that overdoses went up during the decriminalization trial, with 3,313 deaths over 15 months, compared with 2,843 in the same time frame before drugs were temporarily legalized.
-

 International14 hours ago
International14 hours agoPoland’s president signs new zero income tax law for parents with two children
-

 Business4 hours ago
Business4 hours agoFord’s Whisky War
-

 International14 hours ago
International14 hours agoAustralian territory bans men from women’s prisons in national first
-

 Business2 days ago
Business2 days agoCutting Red Tape Could Help Solve Canada’s Doctor Crisis
-

 Automotive1 hour ago
Automotive1 hour ago$15 Billion, Zero Assurances: Stellantis Abandons Brampton as Trudeau-Era Green Deal Collapses
-

 Business1 day ago
Business1 day agoFederal Budget 2025: A responsible media would ensure Canadians know about the dismal state of federal finance
-
 Business1 day ago
Business1 day agoEthics on Ice: See You Next Year
-

 Alberta23 hours ago
Alberta23 hours agoDiploma Exams Affected: No school Monday as ATA rejects offer of enhanced mediation