Addictions
B.C. parents powerless to help their addicted teens

B.C. parents say the province’s safer supply program and legal treatment framework leave them powerless to help their addicted teens
On Aug. 19, 2022, Kamilah Sword took a single hydromorphone pill, believing it to be safe. She overdosed and was found dead by her grandmother the next day. She was 14.
Kamilah believed the drug was safe — despite having bought it illicitly — because she was told it came from a government-run “safer supply” program, according to Kamillah’s best friend Grace Miller and her father.
“I’ll never get to see her get married, never have grandkids, never get to see her graduate,” said Kamilah’s father, Gregory Sword, lowering his chin to keep his voice steady.
“It’s a black hole in the heart that never heals.”
Sword faced significant challenges trying to get his daughter help during the year he was aware she was struggling with addiction. He blames British Columbia’s safer supply program and the province’s legal youth treatment framework for exacerbating his daughter’s challenges and ultimately contributing to her death.
“It’s a B.C. law — you cannot force a minor into rehab without their permission,” said Sword. “You cannot parent your kid between the ages of 12 and 18 without their consent.”
Sword is now pursuing legal action against the B.C. and federal governments and several health agencies, seeking accountability for what he views as systemic failures.
B.C.’s “Safe” supply program
B.C.’s prescribed safer supply program, which was first launched in 2020, is designed to reduce substance users’ reliance on dangerous street drugs. Users are prescribed hydromorphone — an opioid as potent as heroin — as an alternative to using potentially lethal street drugs.
However, participants in the program often sell their hydromorphone, in some cases to teenagers, to get money to buy stronger drugs like fentanyl.
According to Grace Miller, she and Kamilah would obtain hydromorphone — which is commonly referred to as Dilaudid or “dillies” — from a teenage friend who bought them in Vancouver’s Downtown Eastside. The neighbourhood, which is the epicentre of Vancouver’s drug crisis, is a 30-minute SkyTrain ride from the teenagers’ home in Port Coquitlam.
Sword says he initially thought “dillies” referred to Dairy Queen’s Dilly Bars. “My daughter would ask me for $5, [and say], ‘Yeah, we’re going to Dairy Queen for a Dilly Bar.’ I had no idea.”
He says he only learned about hydromorphone after the coroner informed him that Kamilah had three substances in her system: cocaine, MDMA and hydromorphone.
“I had to start talking to people to figure out what [hydromorphone] was and where it was coming from.”
Sword is critical of B.C.’s safer supply program for being presented as safe and for lacking monitoring safeguards. “[Kamilah] knew where [the drugs] were coming from so she felt safe because her dealer would keep on telling her, ‘This is safe supply,’” Sword said.
In February, B.C. changed how it refers to the program from “prescribed safer supply” to “prescribed alternatives.”
Grace says another problem with the program is the quantities of drugs being distributed.
“It would be a big difference if the prescriptions that they were giving out were dosed properly,” she said, noting addicts would typically sell bottles containing 14 pills, with pricing starting at $1 a pill.
‘Safer supply’
Sword estimates his daughter struggled with addiction for about 18 to 24 months before her final, fatal overdose.
After Kamilah overdosed for the first time on Aug. 21, 2021, he tried to get her into treatment. A drug counsellor told him that, because she was over 12, she would need to verbally consent. Kamilah refused treatment.
B.C.’s Infants Act allows individuals aged 12 or older to consent to their own medical treatment if they understand the treatment and its implications. The province’s Mental Health Act requires minors aged 12 to 16 to consent to addiction or mental health treatment.
While parents can request involuntary admission for children under 16, a physician or nurse practitioner must first confirm the presence of a mental disorder that requires treatment. No law specifically addresses substance-use disorders in minors.
When Kamilah was admitted to the hospital on one occasion, she underwent a standard psychiatric evaluation and was quickly discharged — despite Sword’s protests.
Ontario also has a mental health law governing involuntary care. Similar to B.C., they permit involuntary care only where a minor has been diagnosed with a mental disorder.
By contrast, Alberta’s Protection of Children Abusing Drugs Act enables a parent or guardian to obtain a court order to place a child under 18 who is struggling with addiction into a secure facility for up to 15 days for detoxification, stabilization and assessment. Alberta is unique among the provinces and territories in permitting involuntary care of minors for substance-use issues.
Grace, who also became addicted to opioids, says her recovery journey involved several failed attempts.
“I never thought I would have almost died so many times,” said Grace, who is now 16. “I never thought I would even touch drugs in my life.”
Grace’s mother Amanda (a pseudonym) faced similar struggles as Sword in trying to get help for her daughter. Amanda says she was repeatedly told nothing more could be done for Grace, because Grace would not consent to treatment.
“One time, [Grace] overdosed at home, and I had to Narcan her because she was dead in her bed,” Amanda said. “I told the paramedic, ‘Our system is broken.’ And she just said, ‘Yes, I know.’”
Yet Grace, who today has been sober for 10 months, would question whether she even had the capacity to consent to treatment when she was addicted to drugs.
Under B.C.’s Health Care (Consent) and Care Facility (Admission) Act, an adult is only considered to have consented to health care if their consent is voluntary, informed, legitimately obtained and the individual is capable of making a decision about their care.
“Mentally able to give consent?” said Grace. “No, I was never really mentally there.”
Subscribe for free to get BTN’s latest news and analysis – or donate to our investigative journalism fund.
System failure
Today, Sword is one of two plaintiffs leading a class-action lawsuit against several provincial and federal health authorities and organizations, including the B.C. Ministry of Health, Health Canada, Vancouver Coastal Health and Vancouver Island Health.
All four of these agencies declined to comment for this story, citing the ongoing court proceedings.
The lawsuit was filed Aug. 15 and is currently awaiting certification to proceed. It alleges the coroner initially identified safer supply drugs as a cause of Kamilah’s death, but later changed the report to omit this reference due to pressure from the province or for other unknown reasons.
It further alleges B.C. and Ottawa were aware that drugs prescribed under safer supply programs were being diverted as early as March 2021, but failed to monitor or control the drugs’ distribution. It points to a Health Canada report and data showing increased opioid-related problems from safer supply programs.
According to Amanda, Kamilah had wanted to overcome her addiction but B.C.’s system failed her.
“I had multiple conversations with Kamilah, and I know Kamilah wanted to get clean,” she says. “But she felt so stuck, like she couldn’t do it, and she felt guilty and ashamed.”
Grace, who battled addiction for four years, is relieved to be sober.
“I’ve never, ever been happier. I’ve never been healthier. It’s the best thing I’ve done for myself,” she said. “It’s just hard when you don’t have your best friend to do it with.”
This article was produced through the Breaking Needles Fellowship Program, which provided a grant to Canadian Affairs, a digital media outlet, to fund journalism exploring addiction and crime in Canada. Articles produced through the Fellowship are co-published by Break The Needle and Canadian Affairs.
Break The Needle. Our content is always free – but if you want to help us commission more high-quality journalism, consider getting a voluntary paid subscription.
Addictions
New RCMP program steering opioid addicted towards treatment and recovery

News release from Alberta RCMP
Virtual Opioid Dependency Program serves vulnerable population in Red Deer
Since April 2024, your Alberta RCMP’s Community Safety and Well-being Branch (CSWB) has been piloting the Virtual Opioid Dependency Program (VODP) program in Red Deer to assist those facing opioid dependency with initial-stage intervention services. VODP is a collaboration with the Government of Alberta, Recovery Alberta, and the Alberta RCMP, and was created to help address opioid addiction across the province.
Red Deer’s VODP consists of two teams, each consisting of a police officer and a paramedic. These teams cover the communities of Red Deer, Innisfail, Blackfalds and Sylvan Lake. The goal of the program is to have frontline points of contact that can assist opioid users by getting them access to treatment, counselling, and life-saving medication.
The Alberta RCMP’s role in VODP:
- Conducting outreach in the community, on foot, by vehicle, and even UTV, and interacting with vulnerable persons and talking with them about treatment options and making VODP referrals.
- Attending calls for service in which opioid use may be a factor, such as drug poisonings, open drug use in public, social diversion calls, etc.
- Administering medication such as Suboxone and Sublocade to opioid users who are arrested and lodged in RCMP cells and voluntarily wish to participate in VODP; these medications help with withdrawal symptoms and are the primary method for treating opioid addiction. Individuals may be provided ongoing treatment while in police custody or incarceration.
- Collaborating with agencies in the treatment and addiction space to work together on client care. Red Deer’s VODP chairs a quarterly Vulnerable Populations Working Group meeting consisting of a number of local stakeholders who come together to address both client and community needs.
While accountability for criminal actions is necessary, the Alberta RCMP recognizes that opioid addiction is part of larger social and health issues that require long-term supports. Often people facing addictions are among offenders who land in a cycle of criminality. As first responders, our officers are frequently in contact with these individuals. We are ideally placed to help connect those individuals with the VODP. The Alberta RCMP helps those individuals who wish to participate in the VODP by ensuring that they have access to necessary resources and receive the medical care they need, even while they are in police custody.
Since its start, the Red Deer program has made nearly 2,500 referrals and touchpoints with individuals, discussing VODP participation and treatment options. Some successes of the program include:
- In October 2024, Red Deer VODP assessed a 35-year-old male who was arrested and in police custody. The individual was put in contact with medical care and was prescribed and administered Suboxone. The team members did not have any contact with the male again until April 2025 when the individual visited the detachment to thank the team for treating him with care and dignity while in cells, and for getting him access to treatment. The individual stated he had been sober since, saying the treatment saved his life.
- In May 2025, the VODP team worked with a 14-year-old female who was arrested on warrants and lodged in RCMP cells. She had run away from home and was located downtown using opioids. The team spoke to the girl about treatment, was referred to VODP, and was administered Sublocade to treat her addiction. During follow-up, the team received positive feedback from both the family and the attending care providers.
The VODP provides same-day medication starts, opioid treatment transition services, and ongoing opioid dependency care to people anywhere in Alberta who are living with opioid addiction. Visit vodp.ca to learn more.
“This collaboration between Alberta’s Government, Recovery Alberta and the RCMP is a powerful example of how partnerships between health and public safety can change lives. The Virtual Opioid Dependency Program can be the first step in a person’s journey to recovery,” says Alberta’s Minister of Mental Health and Addiction Rick Wilson. “By connecting people to treatment when and where they need it most, we are helping build more paths to recovery and to a healthier Alberta.”
“Part of the Alberta RCMP’s CSWB mandate is the enhancement of public safety through community partnerships,” says Supt. Holly Glassford, Detachment Commander of Red Deer RCMP. “Through VODP, we are committed to building upon community partnerships with social and health agencies, so that we can increase accessibility to supports in our city and reduce crime in Red Deer. Together we are creating a stronger, safer Alberta.”
Addictions
Saskatchewan launches small fleet of wellness buses to expand addictions care

By Alexandra Keeler
Across Canada, mobile health models are increasingly being used to offer care to rural and underserved communities
Saskatchewan has launched a small fleet of mobile wellness buses to improve access to primary health care, mental health and addiction services in the province.
The first bus began operating in Regina on Feb. 12. Another followed in Prince Albert on March 21. Saskatoon’s bus was unveiled publicly on April 9. All three are former coach buses that have been retrofitted to provide health care to communities facing barriers to access.
“Mobile health units are proven to improve outcomes for people facing barriers to healthcare,” Kayla DeMong, the executive director of addiction treatment centre Prairie Harm Reduction, told Canadian Affairs in an email.
“We fully support this innovative approach and are excited to work alongside the health bus teams to ensure the people we support receive the care they need, when and where they need it.”
Wellness buses
Like all provinces, Saskatchewan has been grappling with the opioid crisis.
In 2023, an estimated 457 individuals died from overdoses in the province. In 2024, that number fell to 346. But the province continues to struggle with fatal and non-fatal overdoses.
In late February, Saskatoon firefighters responded to more than 25 overdoses in a single 24-hour period. Just over a week later, they responded to 37 overdoses within another 24-hour window.
Saskatchewan’s wellness buses are part of the province’s plan to address these problems. In April 2025, the province announced $2.4 million to purchase and retrofit three coach buses, plus $1.5 million in annual operating funds.
The buses operate on fixed schedules at designated locations around each city. Each bus is staffed with a nurse practitioner, nurse and assessor coordinator who offer services such as overdose reversal kits, addiction medicine and mental health referrals.
“By bringing services directly to where people are, the health buses foster safer, more welcoming spaces and help build trusting relationships between community members and care providers,” said DeMong, executive director of Prairie Harm Reduction.
Saskatoon-based Prairie Harm Reduction is one of the local organizations that partners with the buses to provide additional support services. Prairie Harm Reduction provides a range of family, youth and community supports, and also houses the province’s only fixed supervised consumption site.
The mobile model
Saskatchewan is not the only province using wellness buses. Across Canada, mobile health models are increasingly being used to expand access to care in rural and underserved communities.
In Kingston, Ont., the Street Health Centre operates a retrofitted RV called PORCH (Portable Outreach Care Hub) that serves individuals struggling with homelessness and addiction.
“Our outreach services are extremely popular with our clients and community partners,” Donna Glasspoole, manager at Street Health Centre, said in an emailed statement.
“PORCH hits the road two to three days/week and offers a variety of services, which are dependent on the health care providers and community partners aboard.”
Street Health Centre also has a shuttle service that picks up clients in shelters and brings them to medical clinics or addiction medicine clinics.
The PORCH vehicles are not supported by provincial funding, but instead rely on support from the United Way and other grants. Glasspoole says the centre’s permanent location — which does receive government funding — is more cost-effective to operate.
“The vehicles are expensive to operate and our RV is not great in winter months and requires indoor parking,” she said.

Politically palatable
Many mobile health models currently do not provide controversial services such as supervised drug consumption.
The Saskatchewan Health Authority told Canadian Affairs the province’s new wellness buses will not offer supervised consumption services or safer supply, where drug users are given prescribed opioids as an alternative to toxic street drugs.
“There are no plans to provide supervised consumption services from the wellness buses,” Saskatchewan Health Authority spokesperson Courtney Markewich told Canadian Affairs in a phone call.
This limited scope may make mobile services more politically palatable in provinces that have resisted harm reduction measures.
In Ontario, some harm reduction programs have shifted to mobile models following Premier Doug Ford’s decision to suspend supervised consumption services located within 200 metres of schools and daycares.
In April, Toronto Public Health ended operations at its Victoria Street fixed consumption site, replacing it with street outreach and mobile vans.
The Ontario government’s decision to close the sites is part of a broader pivot away from harm reduction. The province is investing $378 million to transition suspended sites into 19 new “HART Hubs” that offer primary care, mental health, addictions treatment and other supports.
Glasspoole says that what matters most is not whether services are provided at fixed or mobile locations, but how care is delivered.
Models that “reduce barriers to care, [are] non-judgemental, and [are staffed by] trauma-informed providers” are what lead more people toward treatment and recovery, she said in her email.
In Saskatchewan, DeMong hopes the province’s new wellness buses help address persistent service gaps and build trust with underserved communities.
“This initiative is a vital step toward filling long-standing gaps in the continuum of care by providing low-barrier, community-based access to health-care services,” she said.
This article was produced through the Breaking Needles Fellowship Program, which provided a grant to Canadian Affairs, a digital media outlet, to fund journalism exploring addiction and crime in Canada. Articles produced through the Fellowship are co-published by Break The Needle and Canadian Affairs.
Subscribe to Break The Needle
-

 Alberta1 day ago
Alberta1 day agoAlberta judge sides with LGBT activists, allows ‘gender transitions’ for kids to continue
-
 Crime14 hours ago
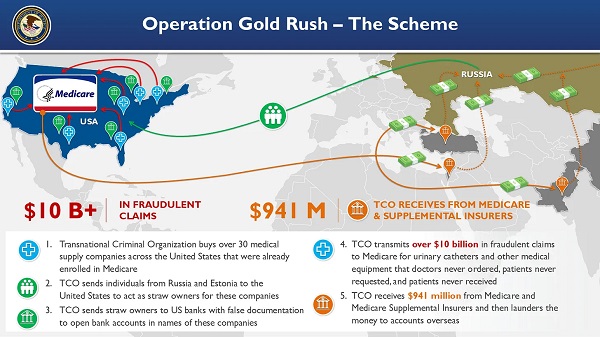
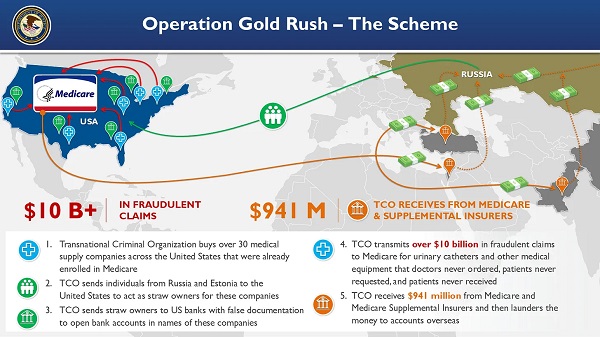
Crime14 hours agoNational Health Care Fraud Takedown Results in 324 Defendants Charged in Connection with Over $14.6 Billion in Alleged Fraud
-

 Health14 hours ago
Health14 hours agoRFK Jr. Unloads Disturbing Vaccine Secrets on Tucker—And Surprises Everyone on Trump
-

 Business3 hours ago
Business3 hours agoElon Musk slams Trump’s ‘Big Beautiful Bill,’ calls for new political party
-

 Business1 day ago
Business1 day agoCanada Caves: Carney ditches digital services tax after criticism from Trump
-

 Crime1 day ago
Crime1 day agoSuspected ambush leaves two firefighters dead in Idaho
-

 Alberta1 day ago
Alberta1 day agoAlberta Independence Seekers Take First Step: Citizen Initiative Application Approved, Notice of Initiative Petition Issued
-

 Censorship Industrial Complex2 hours ago
Censorship Industrial Complex2 hours agoGlobal media alliance colluded with foreign nations to crush free speech in America: House report








