Break The Needle
B.C. crime survey reveals distrust in justice system, regional divides

By Alexandra Keeler
In late August, the RCMP seized nearly 40 kilograms of illegal drugs and half-a-million dollars in cash from a home in Prince George, B.C., while responding to a break-and-enter call.
The RCMP linked the drug operation to organized crime and said it was one of the largest busts in the history of the 80,000-person city, which is located in the B.C. heartland.
“It is obvious we can no longer ignore the effects of the B.C. gang conflict in Prince George, as this is a clear indication that more than our local drug traffickers are using Prince George as a base of operations,” Insp. Darin Rappel, interim detachment commander for the Prince George RCMP, told local media at the time.
It is operations such as these that may be contributing to a perception among British Columbians — particularly those in northern parts of the province — that crime rates are rising.
A survey released Sept. 24 shows a majority of respondents believe B.C. crime rates are up — and often unreported — even though official crime data suggest the opposite.
The survey was commissioned by Save Our Streets, a coalition of more than 100 B.C. community and business groups that is calling for non-partisan, province-wide efforts to establish safer communities in the face of widespread mental health and addiction issues and lack of confidence in the justice system.
“I’m glad that we have our data,” said Jess Ketchum, co-founder of Save Our Streets. “[N]ow we can show that, ‘Look, 88 per cent of the public in B.C. believe that crime is going unreported.’”
“[And] the reason that it’s going unreported is that they’ve lost faith in the justice system,” he said.
‘Revolving doors’
Fifty-five per cent of the 1,200 British Columbians who participated in the survey said they believed criminal activity had increased over the past four years. The survey did not specify types of crime, though it mentioned concerns about violence against employees, vandalism and theft.
But crime data tells a different story. B.C. crime rates fell eight per cent during the years 2020 to 2023, according to Statistics Canada.
Underreporting of crime may partly explain the trend. A 2019 nationwide Statistics Canada survey of individuals aged 15 years and older showed only 29 per cent of violent and non-violent incidents were reported to police. Victims often cited the crime being minor, not important, or no one being harmed as reasons for not reporting.
What is clear is many British Columbians perceive crime is being underreported: 88 per cent of all survey respondents said they believe many crimes go unreported.
 |
Perceptions of Crime & Public Safety in British Columbia. Online survey commissioned by Save Our Streets, conducted by Research Co. with a representative sample of 1,200 British Columbians, Sept 9-12, 2024. (Graphic: Alexandra Keeler)
Mario Canseco, president of Research Co., the public research company that conducted the Save Our Streets survey, attributes the gap between actual and perceived crime rates to the heightened visibility of mental health and addiction issues in the media.
“You look at the reports, you watch television news, listen to the radio, or read the newspaper, and you see that something happened, or that there was a high-profile attack,” said Canseco. “That leads people to believe that things are going badly.”
Survey respondents, though, attributed the lack of crime reporting to a lack of confidence in the justice system, with 75 per cent saying they believe an inadequate court system is to blame. Eighty-seven per cent said they supported bail reform to keep repeat offenders in custody while awaiting trial.
“There was support [in the survey results] for judicial reform that would allow for steps to resolve the revolving doors of the justice system when it comes to repeat offenders,” said Ketchum.
Cowboys
The survey highlighted regional differences in perceptions of B.C. crime rates and views on whether addiction-related crime ought to be addressed as a public health or law enforcement issue.
Respondents from Northern B.C., Prince George and the surrounding Cariboo region were more likely to say they believed criminal activity had increased than respondents from southern and coastal regions of the province.
Canseco suggests that drug use and associated crime are now becoming more apparent in smaller communities, as the drug crisis has spread beyond the major cities of Vancouver and Victoria. Residents of these communities may thus see these problems as more novel and alarming, he says.
Eighty-four per cent of respondents in Northern B.C. said they viewed opioid addiction as a health issue, while only 68 per cent of respondents in Prince George/Cariboo shared this perspective.
Respondents from Prince George/Cariboo exhibited the strongest preference for punitive measures regarding addiction and mental health, with nearly unanimous support for harsher penalties, bail reform and increased police presence.
“It’s one of the tougher areas in the province … somewhat more cowboys,” Ketchum said about Prince George and the Cariboo region, where his hometown of Quesnel is located. “I think there’s less tolerance.”
Subscribe for free to get BTN’s latest news and analysis, or donate to our journalism fund.
Differences in each region’s demographic makeup may also help to explain differing sentiments.
Northern B.C. has the highest concentration of B.C.’s Indigenous population, with about 17 per cent of the population identifying as Indigenous, versus eight per cent in Prince George.
Indigenous communities tend to emphasize addiction as a health issue rooted in historical trauma and social inequities, and prefer community-based healing over punitive measures. Indigenous communities are also frequently distrustful of the RCMP, given its history of being used to extend colonial control.
A majority of all survey respondents favoured investing in mental health facilities, drug education campaigns and rehabilitation over harm-reduction strategies such as safer supply programs, supervised injection sites and drug decriminalization.
“People want to see a more holistic approach [to the drug crisis],” said Canseco. “[T]he voter who hasn’t been exposed to something like [harm reduction], and who may be reacting to what they see on social media, is having a harder time understanding whether this is actually going to help.”
“I was pleased to see the level of support for more investments in recovery, more investments in treatment, around the province,” said Ketchum.
But Ketchum says the preference of some respondents for punitive approaches to B.C. crime rates – particularly in the province’s more northern regions — worries him.
“I believe that if governments don’t respond adequately now, and this is allowed to escalate, that there’ll be more and more instances of people taking these things into their own hands.”
This article was produced through the Breaking Needles Fellowship Program, which provided a grant to Canadian Affairs, a digital media outlet, to fund journalism exploring addiction and crime in Canada. Articles produced through the Fellowship are co-published by Break The Needle and Canadian Affairs.
Subscribe to Break The Needle. Our content is always free – but if you want to help us commission more high-quality journalism, consider getting a voluntary paid subscription.
Addictions
Why B.C.’s new witnessed dosing guidelines are built to fail

Photo by Acceptable at English Wikipedia, ‘Two 1 mg pills of Hydromorphone, prescribed to me after surgery.’ [Licensed under CC BY-SA 3.0, via Wikimedia Commons]
By Alexandra Keeler
B.C. released new witnessed dosing guidelines for safer supply opioids. Experts say they are vague, loose and toothless
This February, B.C pledged to reintroduce witnessed dosing to its controversial safer supply program.
Safer supply programs provide prescription opioids to people who use drugs. Witnessed dosing requires patients to consume those prescribed opioids under the supervision of a health-care professional, rather than taking their drugs offsite.
The province said it was reintroducing witnessed dosing to “prevent the diversion of prescribed opioids and hold bad actors accountable.”
But experts are saying the government’s interim guidelines, released April 29, are fundamentally flawed.
“These guidelines — just as any guidelines for safer supply — do not align with addiction medicine best practices, period,” said Dr. Leonara Regenstreif, a primary care physician specializing in substance use disorders. Regenstreif is a founding member of Addiction Medicine Canada, an advocacy group that represents 23 addiction specialists.
Addiction physician Dr. Michael Lester, who is also a founding member of the group, goes further.
“Tweaking a treatment protocol that should not have been implemented in the first place without prior adequate study is not much of an advancement,” he said.
Witnessed dosing
Initially, B.C.’s safer supply program was generally administered through witnessed dosing. But in 2020, to facilitate access amidst pandemic restrictions, the province moved to “take-home dosing,” allowing patients to take their prescription opioids offsite.
After pandemic restrictions were lifted, the province did not initially return to witnessed dosing. Rather, it did so only recently, after a bombshell government report alleged more than 60 B.C. pharmacies were boosting sales by encouraging patients to fill unnecessary opioid prescriptions. This incentivized patients to sell their medications on the black market.
B.C.’s interim guidelines, developed by the BC Centre on Substance Use at the government’s request, now require all new safer supply patients to begin with witnessed dosing.
But for existing patients, the guidelines say prescribers have discretion to determine whether to require witnessed dosing. The guidelines define an existing patient as someone who was dispensed prescription opioids within the past 30 days.
The guidelines say exemptions to witnessed dosing are permitted under “extraordinary circumstances,” where witnessed dosing could destabilize the patient or where a prescriber uses “best clinical judgment” and determines diversion risk is “very low.”
Holes
Clinicians say the guidelines are deliberately vague.
Regenstreif described them as “wordy, deliberately confusing.” They enable prescribers to carry on as before, she says.
Lester agrees. Prescribers would be in compliance with these guidelines even if “none of their patients are transferred to witnessed dosing,” he said.
In his view, the guidelines will fail to meet their goal of curbing diversion.
And without witnessed dosing, diversion is nearly impossible to detect. “A patient can take one dose a day and sell seven — and this would be impossible to detect through urine testing,” Lester said.
He also says the guidelines do not remove the incentive for patients to sell their drugs to others. He cites estimates from Addiction Medicine Canada that clients can earn up to $20,000 annually by selling part of their prescribed supply.
“[Prescribed safer supply] can function as a form of basic income — except that the community is being flooded with addictive and dangerous opioids,” Lester said.
Regenstreif warns that patients who had been diverting may now receive unnecessarily high doses. “Now you’re going to give people a high dose of opioids who don’t take opioids,” she said.
She also says the guidelines leave out important details on adjusting doses for patients who do shift from take-home to witnessed dosing.
“If a doctor followed [the guidelines] to the word, and the patient followed it to the word, the patient would go into withdrawal,” she said.
The guidelines assume patients will swallow their pills under supervision, but many crush and inject them instead, Regenstreif says. Because swallowing is less potent, a higher dose may be needed.
“None of that is accounted for in this document,” she said.
Survival strategy
Some harm reduction advocates oppose a return to witnessed dosing, saying it will deter people from accessing a regulated drug supply.
Some also view diversion as a life-saving practice.
Diversion is “a harm reduction practice rooted in mutual aid,” says a 2022 document developed by the National Safer Supply Community of Practice, a group of clinicians and harm reduction advocates.
The group supports take-home dosing as part of a broader strategy to improve access to safer supply medications. In their document, they say barriers to accessing safer supply programs necessitate diversion among people who use drugs — and that the benefits of diversion outweigh the risks.
However, the risks — and harms — of diversion are mounting.
People can quickly develop a tolerance to “safer” opioids and then transition to more dangerous substances. Some B.C. teenagers have said the prescription opioid Dilaudid was a stepping stone to them using fentanyl. In some cases, diversion of these drugs has led to fatal overdoses.
More recently, a Nanaimo man was sentenced to prison for running a highly organized drug operation that trafficked diverted safer supply opioids. He exchanged fentanyl and other illicit drugs for prescription pills obtained from participants in B.C.’s safer supply program.
Recovery
Lester, of Addiction Medicine Canada, believes clinical discretion has gone too far. He says take-home dosing should be eliminated.
“Best practices in addiction medicine assume physicians prescribing is based on sound and thorough research, and ensuring that their prescribing does not cause harm to the broader community, as well as the patient,” he said.
“[Safer supply] for opioids fails in both these regards.”
He also says safer supply should only be offered as a short-term bridge to patients being started on proven treatments like buprenorphine or methadone, which help reduce drug cravings and manage withdrawal symptoms.
B.C.’s witnessed dosing guidelines say prescribers can discuss such treatment options with patients. However, the guidelines remain neutral on whether safer supply is intended as a transitional step toward longer-term treatment.
Regenstreif says this neutrality undermines care.
“[M]ost patients I’ve seen with opioid use disorder don’t want to have [this disorder],” she said. “They would rather be able to set goals and do other things.”
Oversight gaps
Currently, about 3,900 people in B.C. participate in the safer supply program — down from 5,200 in March 2023.
The B.C. government has not provided data on how many have been transitioned to witnessed dosing. Investigative journalist Rob Shaw recently reported that these data do not exist.
“The government … confirmed recently they don’t have any mechanism to track which ‘safe supply’ participants are witnessed and which [are] not,” said Elenore Sturko, a Conservative MLA for Surrey-Cloverdale, who has been a vocal critic of safer supply.
“Without a public report and accountability there can be no confidence.”
The BC Centre on Substance Use, which developed the interim guidelines, says it does not oversee policy decisions or data tracking. It referred Canadian Affairs’ questions to B.C.’s Ministry of Health, which has yet to clarify whether it will track and publish transition data. The ministry did not respond to requests for comment by deadline.
B.C. has also not indicated when or whether it will release final guidelines.
Regenstreif says the flawed guidelines mean many people may be misinformed, discouraged or unsupported when trying to reduce their drug use and recover.
“We’re not listening to people with lived experience of recovery,” she said.
This article was produced through the Breaking Needles Fellowship Program, which provided a grant to Canadian Affairs, a digital media outlet, to fund journalism exploring addiction and crime in Canada. Articles produced through the Fellowship are co-published by Break The Needle and Canadian Affairs.
Subscribe to Break The Needle
Addictions
Can addiction be predicted—and prevented?

These four personality traits are predictive of addiction. A new program is using this knowledge to prevent addiction from ever developing
In classrooms across Canada, addiction prevention is getting personal.
Instead of warning students about the dangers of drugs, a program called PreVenture teaches students about themselves — and it’s working.
Developed by Canadian clinical psychologist Patricia Conrod, PreVenture helps young people recognize how traits like risk-taking or negative thinking shape their reactions to stress.
“When you intervene around these traits and help people learn new cognitive behavioural strategies to manage these traits, you are able to reduce their substance use,” said Conrod, who is also a professor at the Université de Montréal.
By tailoring addiction prevention strategies to individual personality profiles, the program is changing how we think about addiction — from something we react to, to something we might stop before it starts.
And now, scientists say the potential for early intervention is going even deeper — down to our genes.
Personality and addiction
PreVenture is a personality-targeted prevention program that helps young people understand and manage traits linked to a higher propensity for future substance use.
The program focuses on four core traits — anxiety sensitivity, sensation seeking, impulsivity and hopelessness — that shape how individuals experience the world and respond to stress, social situations and emotional challenges.
“They don’t only predict who’s at risk,” said Conrod in an interview with Canadian Affairs. “They predict what you’re at risk for with quite a lot of specificity.”
Anxiety sensitivity shows up in people who feel overwhelmed by physical symptoms like a racing heart or dizziness. People with this trait may ultimately turn to alcohol, benzodiazepines such as Xanax, or opioids to calm their bodies.
Sensation seeking is characterized by a desire for excitement and novel experiences. This trait is associated with a higher likelihood of being drawn to substances like cannabis, MDMA, psilocybin or other hallucinogens.
“[Cannabis] alters their perceptual experiences, and so makes things feel more novel,” said Conrod.
Sensation seeking is also associated with binge drinking or use of stimulants such as cocaine.
The trait of impulsivity involves difficulty controlling urges and delaying gratification. This trait is associated with a higher likelihood of engaging in risky behaviours and an increased risk of addiction to a broad range of substances.
“Young people with attentional problems and a core difficulty with response inhibition have a hard time putting a stop on a behaviour once they’ve initiated it,” said Conrod.
Finally, the trait of hopelessness is tied to a pessimistic, self-critical mindset. People with this trait often expect rejection or assume others are hostile, so they may use alcohol or opioids to dull emotional pain.
“We call it negative attributional style,” said Conrod. “They have come to believe that the world is against them, and they need to protect themselves.”
These traits also cluster into two broader categories — internalizing and externalizing.
Anxiety sensitivity and hopelessness direct distress inward, while sensation seeking and impulsivity are characterized by outward disinhibition.
“These traits change your perception,” said Conrod. “You see the world differently through these traits.”
Conrod also notes that these traits appear across cultures, making targeted addiction prevention broadly applicable.
Personality-based prevention
Unlike most one-size-fits-all drug prevention programs, PreVenture tailors its prevention strategies for each individual trait category to reduce substance use risk.
The program uses a brief personality assessment tool to identify students’ dominant traits. It then delivers cognitive-behavioural strategies to help users manage stress, emotions and risky behaviours associated with them.

Recreation of the personality assessment tool based on the substance use risk profile scale — a scale measuring traits linked to reinforcement-specific substance use profiles. | Alexandra Keeler
Students learn to recognize how their dominant trait influences their thoughts and reactions — and how to shift those patterns in healthier directions.
“We’re trying to raise awareness to young people about how these traits are influencing their automatic thinking,” said Conrod. “You’re having them be a little more critical of their thoughts.”
Hopelessness is addressed by teaching strategies to challenge depressive thoughts; those high in sensation seeking explore safer ways to satisfy their need for stimulation; anxiety sensitivity is managed through calming techniques; and impulsivity is reduced by practicing pausing before acting.
Crucially, the program emphasizes the strengths of each trait as well.
“We try to present [traits] in a more positive way, not just a negative way,” said Sherry Stewart, a clinical psychologist at Dalhousie University who collaborates with Conrod.
“Your personality gets you into trouble — certainly, we discuss that — but also, what are the strengths of your personality?”
While a main goal of the program is preventing substance use disorders, the program barely discusses substances.
“You don’t really have to talk about substances very much,” said Conrod. “You talk more about how you’re managing the trait, and it has this direct impact on someone’s motivation to use, as well as how severely they experience mental health symptoms.”
The workshops make it clear, however, that while substances may offer temporary relief, they often worsen the very symptoms participants are trying to manage.
The genetic angle
Catherine Brownstein, a Harvard Medical School professor and geneticist at Boston Children’s Hospital, says genetic factors also help explain why some people are more vulnerable to addiction.
“A lot of personality is genetic,” she said in an interview with Canadian Affairs.
Her research has identified 47 locations in human DNA that affect brain development and shape personality traits.
While substance use risk cannot yet be detected genetically, certain gene variants — like SHANK3, NRXN1 and CRY1 — are linked to psychiatric disorders that often co-occur with substance use, including ADHD and schizophrenia.
Brownstein also says genetic variations influence pain perception.
Some variants increase pain sensitivity, while others eliminate it altogether. One such gene, SCN9A, may make individuals more likely to seek opioids for relief.
“If you’re in pain all the time, you want it to stop, and opioids are effective,” said Brownstein.
While we cannot yet predict addiction risk from genetics alone, Brownstein says she thinks genetic screening combined with psychological profiling could one day personalize prevention even further.
Expansion and challenges
Conrod’s personality-targeted intervention program, PreVenture, has proven highly effective.
A five-year study published in January found that students who participated in PreVenture workshops were 23 to 80 per cent less likely to develop substance use disorders by Grade 11.
Stewart says that the concept of PreVenture began with adults with substance use disorders, but research suggests earlier intervention can alter life trajectories. That insight has driven PreVenture’s expansion to younger age groups.
Conrod’s team delivers PreVenture to middle and high school students, UniVenture to university students and OpiVenture to adults in treatment for opioid dependence.
PreVenture has been implemented in schools across the U.S. and Canada, including in B.C., Ontario, Quebec, Nova Scotia and Newfoundland and Labrador. Five Canadian universities are participating in the UniVenture study.
However, currently, Canada’s flagship youth prevention strategy is based on the Icelandic Prevention Model — a 1990s framework that aims to reduce youth substance use by focusing on environmental factors such as family, school and peer influence.
While the Icelandic Prevention Model has shown success in Iceland, it has serious limitations. It lacks a mental health component, does not specifically address opioid use and has demonstrated mixed results by gender.
Despite strong evidence for personality-targeted prevention, programs like PreVenture remain underused.
Conrod says education systems often default to less effective, generic methods like one-off guest speakers. She also cites staffing shortages and burnout in schools, along with insufficient mental health services, as major barriers to implementing a new program.
Still, momentum is building.
B.C. has aligned their prevention services with the PreVenture model. And organizations such as the youth wellness networks Foundry B.C. and Youth Wellness Hubs Ontario are offering the program and expanding its reach.
Conrod believes the power of the program lies in helping young people feel seen and understood.
“It’s really important that a young person is provided with the space and focus to recognize what’s unique about [their] particular trait,” she said.
“Recognize that there are other people in the world that also think this way [and tell them] you’re not going crazy.”
This article was produced through the Breaking Needles Fellowship Program, which provided a grant to Canadian Affairs, a digital media outlet, to fund journalism exploring addiction and crime in Canada. Articles produced through the Fellowship are co-published by Break The Needle and Canadian Affairs.
-
 Opinion1 day ago
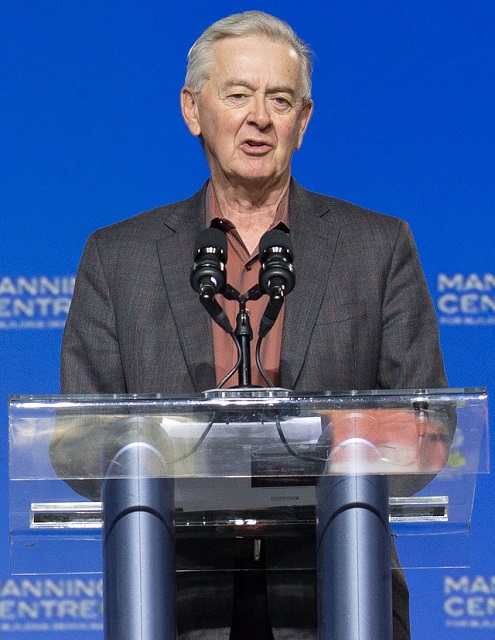
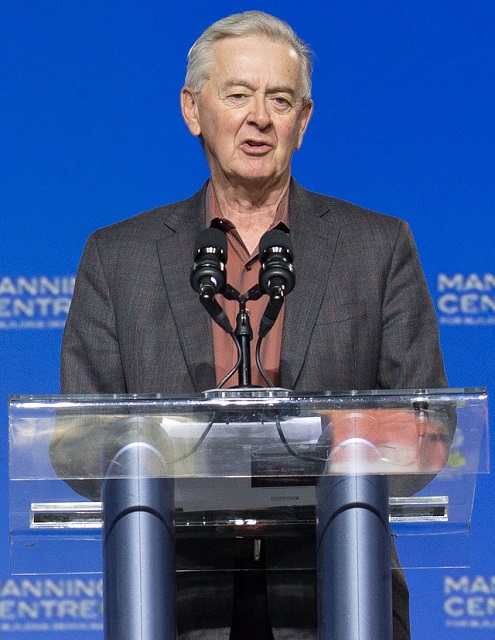
Opinion1 day agoPreston Manning: Three Wise Men from the East, Again
-

 Addictions1 day ago
Addictions1 day agoWhy B.C.’s new witnessed dosing guidelines are built to fail
-

 Uncategorized2 days ago
Uncategorized2 days agoCNN’s Shock Climate Polling Data Reinforces Trump’s Energy Agenda
-
 Business1 day ago
Business1 day agoCarney Liberals quietly award Pfizer, Moderna nearly $400 million for new COVID shot contracts
-

 Business1 day ago
Business1 day agoMark Carney’s Fiscal Fantasy Will Bankrupt Canada
-

 Daily Caller20 hours ago
Daily Caller20 hours ago‘Strange Confluence Of Variables’: Mike Benz Wants Transparency Task Force To Investigate What Happened in Butler, PA
-

 Alberta14 hours ago
Alberta14 hours agoAlberta ban on men in women’s sports doesn’t apply to athletes from other provinces
-

 National14 hours ago
National14 hours agoCanada’s immigration office admits it failed to check suspected terrorists’ background








