Addictions
A conversation with Premier Smith’s outgoing chief of staff, architect of Alberta’s recovery-focused drug policies

Marshall Smith, Alberta’s Chief of Staff, sits in his office at the Alberta Legislature in Edmonton
Marshall Smith, on what he has learned as an addict and policy leader and what’s next for him
Alberta Premier Danielle Smith’s chief of staff, Marshall Smith, is leaving his post at the end of October.
Since taking office in 2022, he has been instrumental in shaping Alberta’s drug policies and developing the Alberta Model — a recovery-focused addiction treatment policy that has gained international recognition for enhancing access to mental health and addiction services.
Under his guidance, Alberta has prioritized building recovery communities over harm-reduction programs. Government data show a 53 per cent decrease in opioid-related overdose deaths in June 2024 from the prior year, which may suggest Smith’s initiatives are having an impact.
In a statement on social media, the Premier shared that Smith informed her of his decision to retire earlier this year, after dedicating 32 years to public service. His departure comes just ahead of the United Conservative Party’s leadership review on Nov. 2.
Smith met with reporter Alexandra Keeler on Sept. 10 to discuss his personal journey from addiction to recovery and how it has shaped Alberta’s drug policies. On Oct. 10, they spoke by phone to discuss his recent decision to step down and what lies ahead for him.
AK: What emotional and psychological impact did your addiction have on your sense of self?
MS: It makes you feel powerless. Addiction is an illness of isolation, despair, loneliness and powerlessness. One of the hallmarks of addiction is continuing to use a substance despite a complete lack of control over your using, and over the circumstances that you’re in.
AK: Do you think that sense of powerlessness impacts an individual’s ability to provide informed consent for involuntary treatment?
MS: I think that, over time, if addiction is left unchecked or untreated, or is allowed to progress to its very latter stages, you absolutely lose agency over your ability to make decisions.
I used to get the question a lot: ‘Is it a disease? Is it a choice?’ And I say it’s both. It’s actually a disease of choices, which is to say that it’s a disease or an illness that affects my brain’s ability to make good choices.
AK: Were you the driving force behind Alberta’s shift away from harm reduction towards a recovery-focused approach, or was there a broader change in attitudes within the community?
MS: Certainly I’m not solely responsible. I’m a member of a broad community of people in recovery who have been advocating for these policies for two decades. I think that I have a background [and] certain skills that have found me in positions like this, where I can be most effective helping my community advance these ideas and concepts and actually get them implemented into policy and action.
AK: Obviously your lived experience with addiction brings a valuable perspective to the table. But what data sources are the province using to inform its addiction and recovery policies?
MS: We have a very broad literature base that we use to inform a lot of our policy decisions … Alberta [also] has the most comprehensive data collection and data analytics system in North America, bar none.
A practical example of how that’s useful is … [if] the data shows us that a very high number of people who were in custody — whether that’s corrections or police custody — went on to fatally overdose in a period after their release, that tells us that we need to focus on correctional programs, and we need to focus on policing programs.
And we’ve done that. We have amazing new correctional treatment programs that are second to none. I don’t know of anybody in Canada that’s doing this — we’ve taken [jail units where inmates sleep and live] and turned them into treatment centres, and connected them with our new treatment centres outside of jails. We partnered with police, because police have probably the most amount of contact with people who are using substances, and we gave them the ability to help people get on to opioid-substitution medications.
We’re going to go even further. Minister [of Mental Health and Addiction Dan] Williams has just announced the creation of the Centre of Recovery Excellence (CoRE), which is a first of its kind in Canada. It’s a Crown corporation not beholden to pharmaceutical money, which is a big change for us, and we were very deliberate about that.
[CoRE] will give us the ability to pull in data from across systems in government and have that data analyzed … So we’re entering into a very exciting time in terms of data and analytics around this issue.
AK: Without CoRE fully operational yet, what made you confident the recovery-focused approach would succeed?
MS: I see hundreds of thousands of Canadians every day entering recovery and maintaining their recovery … What I see in the alternative is a lot of drug use, homelessness, despair, disease [and] crime.
We spend a lot of time talking about data and evidence and science, and all of those things are good and necessary … but it’s not the only component of the decision-making process. … The policies that we’re making and the pathways that we take also have to be informed by the values of the community that we serve. … For far too long in Canada, that hasn’t been a consideration.
I think that we are at a place in Canada where the country is saying to us it’s time to revisit the direction that we’ve been going. I think that they’re saying to us, as policymakers, that we gave this a chance. We had become convinced by experts and the media … to give [pro-drug, harm-reduction policies like safer supply] a try …
[A]fter 20 years of that, I think that Canadians are ready to throw in the towel and to say, ‘We’re done with this. We’ve given you enough time to prove out your thesis. It’s not worked, and now we’re looking for fresh ideas.’
So Alberta is here leading that conversation of fresh and different ideas, and we’re happy to have that role.
The remainder of this interview took place on Oct. 10.
AK: Premier Smith announced your retirement at the end of October. What prompted your decision to step down?
MS: My time in Alberta has been a lengthy and intense role of system transformation over two premiers and standing up government twice.
While there’s still a lot of work to be done here, we have a tremendous team in Alberta that is leading that work under Minister Williams. I just felt that it’s time for me to step out of the role and continue to serve in other capacities.
AK: Looking ahead, what aspects of the Alberta Model will you carry with you into your future endeavours?
MS: I would say all aspects of the model need to be expanded across Canada, for jurisdictions that are interested.
Where I can be of the most assistance to other governments is talking to them about how to effectively organize themselves to be successful in this area. I think that governments across the country are struggling to figure out how to do that.
AK: What new opportunities do you hope to pursue that you haven’t been able to explore during your time in this role? Will your focus continue to be in addiction and drug policy?
MS: The majority of my focus will be on addiction and drug policy, but I have other areas of interest.
I’m passionate about the work that we’re doing with Indigenous people … I’m also very passionate about emerging technology and how we’re going to use that to uncover some of the answers that we’re looking for on these models.
I’m looking forward to having a little bit more freedom and focus.
This interview has been edited and condensed for clarity.
This article was produced through the Breaking Needles Fellowship Program, which provided a grant to Canadian Affairs, a digital media outlet, to fund journalism exploring addiction and crime in Canada. Articles produced through the Fellowship are co-published by Break The Needle and Canadian Affairs.
Subscribe to Break The Needle. Our content is always free – but if you want to help us commission more high-quality journalism, consider getting a voluntary paid subscription.
Addictions
Activists Claim Dealers Can Fix Canada’s Drug Problem

By Adam Zivo
We should learn from misguided experiments with activist-driven drug ideologies.
Some Canadian public-health researchers have argued that the nation’s drug dealers, far from being a public scourge, are central to the cause of “harm reduction,” and that drug criminalization makes it harder for them to provide this much-needed “mutual aid.” Incredibly, these ideas have gained traction among Canada’s policymakers, and some have even been put into practice.
Gillian Kolla, an influential harm-reduction activist and researcher, spearheaded the push to whitewash drug trafficking in Canada. Over the past decade, she has advocated for many of the country’s failed laissez-faire drug policies. In her 2020 doctoral dissertation, she described her hands-on research into Toronto’s “harm reduction satellite sites”—government-funded programs that paid drug users to provide services out of their homes.
The sites Kolla studied were operated by the nonprofit South Riverdale Community Health Centre (SRCHC) in Toronto. Addicts participating in the programs received $250 per month in exchange for distributing naloxone and clean paraphernalia (needles and crack pipes, for example), as well as for reversing overdoses and educating acquaintances on safer consumption practices. At the time of Kolla’s research (2016–2017), the SRCHC was operating nine satellite sites, which reportedly distributed about 1,500 needles and syringes per month.
Canada permits supervised consumption sites—facilities where people can use drugs under staff oversight—to operate so long as they receive an official exemption via the federal Controlled Drugs and Substances Act. As the sites Kolla observed did not receive exemptions, they were certainly illegal. Kolla herself acknowledged this in her dissertation, writing that she, with the approval of the University of Toronto, never recorded real names or locations in her field notes, in case law enforcement subpoenaed her research data.
Even so, the program seems to have enjoyed the blessing of Toronto’s public health officials and police. The satellite sites received local funding from 2010 onward, after a decade of operating on a volunteer basis, apparently with special protection from law enforcement. In her dissertation, Kolla described how SRCHC staff trained police officers to leave their sites alone, and how satellite-site workers received special ID badges and plaques to ward off arrest.
Kolla made it clear that many of these workers were not just addicts but dealers, too, and that tolerance of drug trafficking was a “key feature” of the satellite sites. She even described, in detail, how she observed one of the site workers packaging and selling heroin alongside crackpipes and needles.
In her dissertation, Kolla advocated expanding this permissive approach. She claimed that traffickers practice harm reduction by procuring high-quality drugs for their customers and avoiding selling doses that are too strong.
“Negative framings of drug selling as predatory and inherently lacking in care make it difficult to perceive the wide variety of acts of mutual aid and care that surround drug buying and selling as practices of care,” she wrote.
In truth, dealers routinely sell customers tainted or overly potent drugs. Anyone who works in the addiction field can testify that this is a major reason that overdose deaths are so common.
Ultimately, Kolla argued that “real harm reduction” should involve drug traffickers, and that criminalization creates “tremendous barriers” to this goal.
The same year she published her dissertation, Kolla cowrote a paper in the Harm Reduction Journal with her Ph.D. supervisor at the Dalla Lana School of Public Health. The article affirmed the view that drug traffickers are essential to the harm-reduction movement. Around this time, the SRCHC collaborated with the Toronto-based Parkdale Queen West Community Health Centre— the only other organization running such sites—to produce guidelines on how to replicate and scale up the experiment.
Thankfully, despite its local adoption, this idea did not catch on at the national level. It was among the few areas in the early 2020s where Canada did not fully descend into addiction-enabling madness. Yet, like-minded researchers still echo Kolla’s work.
In 2024, for example, a group of American harm-reduction advocates published a paper in Drug and Alcohol Dependence Reports that concluded, based on just six interviews with drug traffickers in Indianapolis, that dealers are “uniquely positioned” to provide harm-reduction services, partly because they are motivated by “the moral imperative to provide mutual aid.” Among other things, the authors argued that drug criminalization is harmful because it removes dealers from their social networks and prevents them from enacting “community-based practices of ethics and care.”
It’s instructive to review what ultimately happened with the originators of this movement—Kolla and the SRCHC. Having failed to whitewash drug trafficking, Kolla moved on to advocating for “safer supply”—an experimental strategy that provides addicts with free recreational drugs to dissuade use of riskier street substances. The Canadian government funded and expanded safer supply, thanks in large part to Kolla’s academic work. It abandoned the experiment after news broke that addicts resell their safer supply on the black market to buy illicit fentanyl, flooding communities with diverted opioids and fueling addiction.
The SRCHC was similarly discredited after a young mother, Karolina Huebner-Makurat, was shot and killed near the organization’s supervised consumption site in 2023. Subsequent media reports revealed that the organization had effectively ignored community complaints about public safety, and that staff had welcomed, and even supported, drug traffickers. One of the SRCHC’s harm-reduction workers was eventually convicted of helping Huebner-Makurat’s shooter evade capture by hiding him from the police in an Airbnb apartment and lying to the police.
There is no need for policymakers to repeat these mistakes, or to embrace its dysfunctional, activist-driven drug ideologies. Let this be another case study of why harm-reduction policies should be treated with extreme skepticism.
Our content is always free
If you want to help us commission more high-quality journalism,
consider getting a voluntary paid subscription.
Addictions
Canadian gov’t not stopping drug injection sites from being set up near schools, daycares

From LifeSiteNews
Canada’s health department told MPs there is not a minimum distance requirement between safe consumption sites and schools, daycares or playgrounds.
So-called “safe” drug injection sites do not require a minimum distance from schools, daycares, or even playgrounds, Health Canada has stated, and that has puzzled some MPs.
Canadian Health Minister Marjorie Michel recently told MPs that it was not up to the federal government to make rules around where drug use sites could be located.
“Health Canada does not set a minimum distance requirement between safe consumption sites and nearby locations such as schools, daycares or playgrounds,” the health department wrote in a submission to the House of Commons health committee.
“Nor does the department collect or maintain a comprehensive list of addresses for these facilities in Canada.”
Records show that there are 31 such “safe” injection sites allowed under the Controlled Drugs And Substances Act in six Canadian provinces. There are 13 are in Ontario, five each in Alberta, Quebec, and British Columbia, and two in Saskatchewan and one in Nova Scotia.
The department noted, as per Blacklock’s Reporter, that it considers the location of each site before approving it, including “expressions of community support or opposition.”
Michel had earlier told the committee that it was not her job to decide where such sites are located, saying, “This does not fall directly under my responsibility.”
Conservative MP Dan Mazier had asked for limits on where such “safe” injection drug sites would be placed, asking Michel in a recent committee meeting, “Do you personally review the applications before they’re approved?”
Michel said that “(a)pplications are reviewed by the department.”
Mazier stated, “Are you aware your department is approving supervised consumption sites next to daycares, schools and playgrounds?”
Michel said, “Supervised consumption sites were created to prevent overdose deaths.”
Mazier continued to press Michel, asking her how many “supervised consumption sites approved by your department are next to daycares.”
“I couldn’t tell you exactly how many,” Michel replied.
Mazier was mum on whether or not her department would commit to not approving such sites near schools, playgrounds, or daycares.
An injection site in Montreal, which opened in 2024, is located close to a kindergarten playground.
Conservative Party leader Pierre Poilievre has called such sites “drug dens” and has blasted them as not being “safe” and “disasters.”
Records show that the Liberal government has spent approximately $820 million from 2017 to 2022 on its Canadian Drugs and Substances Strategy. However, even Canada’s own Department of Health admitted in a 2023 report that the Liberals’ drug program only had “minimal” results.
Recently, LifeSiteNews reported that the British Columbia government decided to stop a so-called “safe supply” free drug program in light of a report revealing many of the hard drugs distributed via pharmacies were resold on the black market.
British Columbia Premier David Eby recently admitted that allowing the decriminalization of hard drugs in British Columbia via a federal pilot program was a mistake.
Former Prime Minister Justin Trudeau’s loose drug initiatives were deemed such a disaster in British Columbia that Eby’s government asked Trudeau to re-criminalize narcotic use in public spaces, a request that was granted.
Official figures show that overdoses went up during the decriminalization trial, with 3,313 deaths over 15 months, compared with 2,843 in the same time frame before drugs were temporarily legalized.
-

 Health2 days ago
Health2 days agoCDC’s Autism Reversal: Inside the Collapse of a 25‑Year Public Health Narrative
-

 Health2 days ago
Health2 days agoBREAKING: CDC quietly rewrites its vaccine–autism guidance
-

 Crime2 days ago
Crime2 days agoCocaine, Manhunts, and Murder: Canadian Cartel Kingpin Prosecuted In US
-

 Daily Caller2 days ago
Daily Caller2 days agoBREAKING: Globalist Climate Conference Bursts Into Flames
-
 Alberta2 days ago
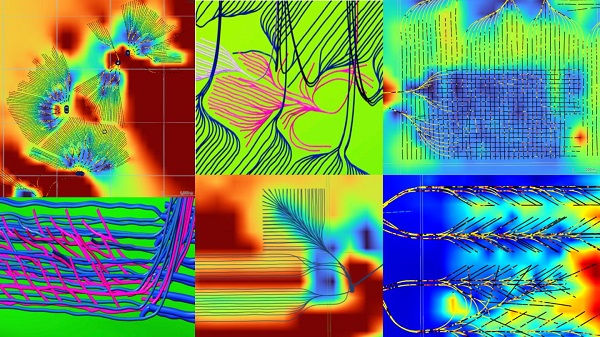
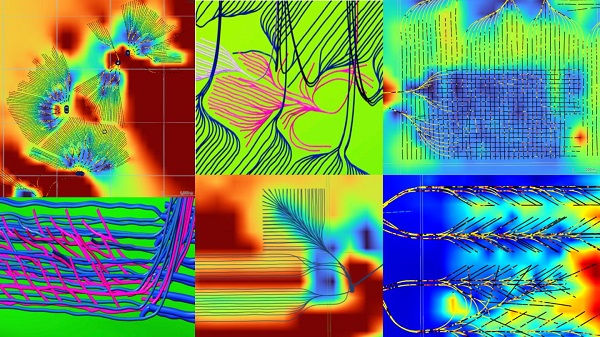
Alberta2 days ago‘Weird and wonderful’ wells are boosting oil production in Alberta and Saskatchewan
-

 Energy2 days ago
Energy2 days agoHere’s what they don’t tell you about BC’s tanker ban
-

 Business11 hours ago
Business11 hours agoNew airline compensation rules could threaten regional travel and push up ticket prices
-

 Bruce Dowbiggin1 day ago
Bruce Dowbiggin1 day agoBurying Poilievre Is Job One In Carney’s Ottawa