From The Center Square
“Most powerful executive order on pharmacy pricing and health care ever in the history of our nation.”
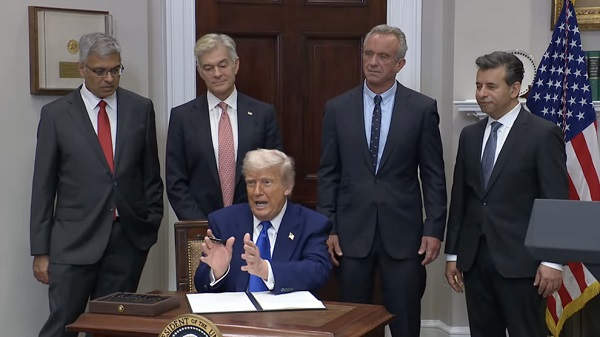
President Donald Trump hosted a press conference with Secretary of Health and Human Services Robert F. Kennedy, Jr., and other health administration officials Monday morning formally announcing an executive order aiming to drastically reduce what Americans pay for their prescription drugs up to 90%, according to Trump.
The order seeks to reform how much the U.S. pays for pharmaceutical drugs compared to other countries. On average, Americans pay nearly four times more than other countries for their prescription drugs, effectively subsidizing pharmaceutical companies’ research and development costs for others around the world, according to the administration.
The order was immediately met with skepticism by some critics.
“If Trump is serious about making real change rather than just issuing a press release, he will support legislation I will introduce to ensure we pay no more for prescription drugs than people in other major countries,” Sen. Bernie Sanders, I-Vt., posted on X after the press conference, touting his own legislation and saying Trump’s order will be “thrown out by the courts.”
“If we come together, we can get it passed in a few weeks,” Sanders said.
Food and Drug Administration Commissioner and Johns Hopkins surgical oncologist Marty Makary was one of the officials who spoke at the press conference Monday morning.
“We didn’t take an oath to heal patients and then watch their life get ruined financially with their home, mortgage, retirement going down the drain with Go Fund Me campaigns, raising money from church communities and synagogues and friends they haven’t seen in 20 years to try to raise money – for what?” said Food and Drug Administration Commissioner Marty Makary.
“For a system where Americans have been getting ripped off by 10, 12, 15 times higher prices than we see in other countries?”
Makary and others said the “fundamental problem” with American prescription drug costs is a lack of competition in the global marketplace, with Americans comprising only about 4% of the global population but supplying at least two-thirds of drug companies’ revenue globally.
“The fundamental problem in health care is that we’ve had non-competitive markets,” Makary continued. “We can do little things around the edges, or we can transform those markets into competitive markets, and that’s what this executive order does.”
The order intends to secure the “most-favored-nation” price for pharmaceutical drugs for the U.S., or the lowest price among its economic peer countries, through a series of actions. It instructs the U.S. secretary of commerce and the U.S. trade representative to “ensure” that other countries aren’t engaging in practices that “[force] American patients to pay for a disproportionate amount of global pharmaceutical research and development.” Kennedy is to work in coordination with Centers for Medicare and Medicaid Administrator Mehmet Oz and others to develop most-favored-nation target pricing for pharmaceutical companies. It also directs Kennedy to devise direct-to-consumer purchasing programs for drug companies that abide by the president’s most-favored-nation pricing mandate for the U.S.
Oz called the order the “most powerful executive order on pharmacy pricing and health care ever in the history of our nation.”
If drug companies don’t comply, then the order directs Kennedy to create a rulemaking plan to impose the targeted pricing, or certify to Congress that the U.S. can import the drugs that remain too expensive under certain importation waivers. Certain drugs may even have their FDA approvals revoked by Makary.
Kennedy said some politicians, including Sanders, have been promising to “equalize” what the U.S. and Europe pay for pharmaceutical drugs for years, while knowing they can’t deliver on the promise because of the deep entanglement between the pharmaceutical industry and Congress. And even though he too has been promising to do something about the issue for years, he didn’t think he would see a solution emerge in his lifetime.
“I’m just so grateful to be here today. I never thought this would happen in my lifetime,” Kennedy said. “I have a couple of kids who are Democrats, who are big Bernie Sanders fans. When I told them what was going to happen, they had tears in their eyes, because they thought this was never going to happen in our lifetime.”
Kennedy and the other health administration officials who spoke praised the president for being willing to stand up to the industry and its powerful lobby, which has one to three times as many lobbyists in Washington as there are members of Congress and the Supreme Court, according to Kennedy.
“We finally have a president who’s willing to stand up for the American people,” Kennedy said.