Health
How the once-blacklisted Dr. Jay Bhattacharya could help save healthcare

From LifeSiteNews
Now seated at the helm of the National Institutes of Health, Dr. Jay Bhattacharya is poised to reshape not only the agency’s research priorities but the very culture that pushed him to the fringe.
Imagine spending your career studying infectious diseases, only to find that the real virus spreading uncontrollably is censorship. That was the reality for Dr. Jay Bhattacharya, a Stanford epidemiologist who committed the unpardonable sin of questioning the COVID-19 lockdown orthodoxy. His punishment? Digital exile, courtesy of Silicon Valley’s Ministry of Truth.
In December 2022, the Twitter Files exposed what many had long suspected: Twitter had quietly placed Bhattacharya’s account on a Trends Blacklist. This ensured that his posts, often critical of lockdowns and mask mandates, would never see the light of day on the platform’s trending topics. In other words, Twitter’s algorithm worked like a digital bouncer, making sure his dissenting opinions never made it past the velvet rope.

And Twitter wasn’t alone. Facebook, ever eager to please its government handlers, scrubbed the Great Barrington Declaration from its pages. That document, co-authored by Bhattacharya and other esteemed scientists, dared to suggest that maybe, just maybe, locking down entire populations wasn’t the best strategy. Instead, it proposed focused protection for the most vulnerable while allowing the rest of society to function. For this, it was sent to the digital equivalent of a gulag.
These experiences took center stage during Bhattacharya’s Senate confirmation hearing for the directorship of the National Institutes of Health (NIH). Republican lawmakers, who suddenly found themselves cast as the last defenders of free speech in scientific discourse, saw his nomination as a win.
During his testimony, Bhattacharya didn’t mince words. He detailed how the Biden administration played an active role in orchestrating the suppression of alternative views. It wasn’t enough for officials to push their own pandemic policies — they needed to ensure that no one, regardless of expertise, could challenge them in the public square.
The Science™ vs. The Science
Bhattacharya’s testimony laid bare an uncomfortable truth: the pandemic was a crisis of speech. “The root problem was that people who had alternative ideas were suppressed,” he told Sen. Ashley Moody (R-Fla.). “I personally was subject to censorship by the actions of the Biden administration during the pandemic.”
In a functioning society, that statement would spark bipartisan outrage. Instead, it barely registered. The people who spent years chanting “trust the science” were never interested in science at all.
Real science thrives on debate, skepticism, and the understanding that no single expert — no matter how credentialed—holds absolute truth. But during COVID, science became The Science™ — a government-approved doctrine enforced by Silicon Valley moderators and federal bureaucrats. Deviate from it, and you weren’t just wrong. You were dangerous.
A government-sanctioned muzzle
Bhattacharya wasn’t silenced in some haphazard, accidental way. The Biden administration actively leaned on social media companies to “moderate” voices like his. In practice, that meant tech executives — most of whom couldn’t tell a virus from a viral tweet — decided which epidemiologists the public was allowed to hear.
He responded with a lawsuit against the administration, accusing it of colluding with Big Tech to crush dissent. But in a ruling as predictable as it was revealing, the Supreme Court dismissed the case, arguing that Bhattacharya and his fellow plaintiffs lacked standing. Meaning: Yes, the government may have pressured private companies into silencing critics, but unless you can prove exactly how that harmed you, don’t expect the courts to care.
The real role of science
Despite everything, Bhattacharya didn’t argue for scientists to dictate policy. Unlike the public health bureaucrats who spent the pandemic issuing commandments from their Zoom thrones, he made it clear: “Science should be an engine for freedom,” he said. “Not something where it stands on top of society and says, ‘You must do this, this or this, or else.’”
That distinction matters. Science informs, but policy is about trade-offs. The problem wasn’t that officials got things wrong — it’s that they refused to admit the possibility. Instead of allowing open debate, they silenced critics. Instead of acknowledging uncertainty, they imposed rules with absolute certainty.
Bhattacharya wasn’t censored because he was wrong. He was censored because he questioned people who couldn’t afford to be.
His confirmation hearing made one thing clear: science wasn’t about data. It was about power. And in Washington, power doesn’t like to be questioned.
Science, money and power
At the heart of the hearing was a fundamental question: Who controls science that people are allowed to talk about? The NIH, with its $48 billion budget, is less a research institution and more a financial leviathan, shaping the direction of American science through the projects it funds (or doesn’t) fund.
Bhattacharya’s nomination comes at a moment when the battle lines around scientific freedom, government intervention, and public trust in research are more entrenched than ever. The pandemic shattered the illusion that science was above politics. Instead, it exposed just how much political and corporate interests shape what counts as “settled” science.
The irony is thick enough to cut with a knife. The man once branded too dangerous for social media, blacklisted for questioning lockdowns, and effectively erased from mainstream discourse is now being handed a key role in the very government that tried to silence him. Dr. Jay Bhattacharya, once forced to the margins, is now at the center of power.
A new administration has decided that maybe — just maybe — silencing dissenting scientists wasn’t the best pandemic strategy. And in a twist no Hollywood scriptwriter would dare to pitch for being too on-the-nose, Bhattacharya wasn’t being welcomed back into the conversation — he’s being put in charge of it.
Bhattacharya was confirmed following a party-line vote Tuesday evening. The decision came after a similarly partisan endorsement from the Senate Committee on Health, Education, Labor and Pensions (HELP), clearing the final hurdle for President Donald Trump’s nominee.
Equally central to his testimony was Bhattacharya’s call for a sweeping shift in NIH priorities. He proposed a decentralization of research funding, stressing the need for greater inclusion of dissenting voices in the scientific process, an apparent rebuke of the consensus-driven culture that dominated during the pandemic. He emphasized targeting resources toward projects with a clear and measurable impact on public health, dismissing other NIH initiatives as “frivolous.”
Now seated at the helm of the National Institutes of Health, Dr. Jay Bhattacharya is poised to reshape not only the agency’s research priorities but the very culture that pushed him to the fringe. His confirmation, hard-won and unapologetically political, is already shaking the scaffolding of a scientific establishment that long equated conformity with consensus.
Reprinted with permission from Reclaim The Net.
Health
CDC Vaccine Panel Votes to End Universal Hep B Vaccine for Newborns

“While I question whether any baby should receive a vaccine against a rare disease in infancy, I am pleased that this is now a matter for parents and their healthcare practitioner to decide — not a state mandate based on a federal pharma-backed recommendation.”
Advisers to the Centers for Disease Control and Prevention (CDC) have voted to end a decades-long recommendation that all infants born in the U.S. receive the hepatitis B vaccine (Hep B) within 12-24 hours of birth.
Instead, for babies born to mothers who test negative for hepatitis B, the committee recommends that families determine whether to give their child the Hep B shot at birth through individual decision-making with their physician.
For infants who don’t get the birth dose, the committee recommends the initial dose of the vaccine not be administered until infants are at least 2 months old.
Three of the 11 committee members — Dr. Raymond Pollack, Dr. Cody Meissner and Dr. Joseph R. Hibbeln — opposed the recommendation. The remaining eight members supported it.
Andrew Johnson from the Centers for Medicare & Medicaid Services assured the committee that the language change will not affect Medicaid or insurance coverage of the vaccine.
For mothers whose hepatitis B status is unknown or who test positive, the birth dose recommendation remains in place.
Children’s Health Defense CEO Mary Holland, a long-time critic of the universal birth dose policy, welcomed the committee’s vote to “end the ill-considered universal recommendation for the Hep B birth vaccine dose.”
Holland added:
“The science behind that universal recommendation was a sham, based on thoroughly inadequate clinical trials. Hundreds of babies unquestionably died because of it. While I question whether any baby should receive a vaccine against a rare disease in infancy, I am pleased that this is now a matter for parents and their healthcare practitioner to decide — not a state mandate based on a federal pharma-backed recommendation.
“And while the ACIP [Advisory Committee on Immunization Practices] debate on this issue was tedious and rancorous at times, it is an extremely positive change that actual debate about childhood vaccines is occurring in government venues with impact. This is the transparency that Secretary Kennedy promised.”
Dr. Monique Yohanan, senior fellow for health policy at Independent Women, told The Defender there was never “a good science-based reason to have a universal vaccination that 99% of babies born in the United States are not at any risk,” and that the vote was “good news for babies.”
She added that she hoped it would “provide an opportunity to actually have outreach to the moms who are positive for hepatitis B, women who are immigrants, women who are IV drug users.” She said the previous policy was “performative compassion. And these are really underserved women who we ignored the outreach that they needed.”
The committee also voted 6-4 with one abstention that after the initial Hep B shot, parents should consult with healthcare providers to consider whether their child should have a serology test, which would show whether they had antibodies considered sufficient to protect them against the disease.
The committee voted to update the CDC Vaccines for Children (VFC) Program funding to match ACIP’s recommendations. Several committee members, including Meissner and Hibbeln, abstained from voting on the VFC resolution, protesting that they didn’t understand the implications of the vote — reflecting some of the disagreement that pervaded the two-day meeting.
The votes on the Hep B vaccine were originally scheduled for the September meeting, but were deferred to allow the CDC work group to put together more data to inform the committee’s decision.
Sunday’s vote was postponed from Saturday so members could have more time to review the language of the proposal.
Like flying in a plane that wasn’t safety tested?
The decision to postpone followed a contentious day-long meeting on Thursday, during which some members of the committee and liaisons from professional associations argued there was no need to change the recommendation, because there was no “evidence of harm” from the vaccine.
Advocates for changing the recommendation pointed to a near-complete lack of safety data — small clinical trials for the vaccines tracked infants for a week or less after the shot and little follow-up research on autoimmune and neurological disorders.
Big differences of opinion persisted at Sunday’s meeting.
ACIP member Retsef Levi, Ph.D., said that for parents whose children were at extremely low risk, the decision to give them the vaccine was analogous to flying in a plane — they wouldn’t get in a plane that hadn’t been safety tested, why should they give their child a vaccine that hadn’t been safety tested.
Meissner disagreed, saying, “We know vaccines are safe. There is no question that the COVID vaccine recommendations were dishonest, disingenuous, but the hepatitis B vaccine is very well established.”
In opening remarks, Dr. Robert Malone — who chaired the meeting because the newly named committee chairperson, Dr. Kirk Milhoun, is traveling — said “the credibility of the ACIP rests not on speed, but on rigor.”
Commenting on the heated discussions during Thursday’s meeting, Milhoun said that scientific debates are necessarily contentious.
“If they are not contentious, if they are not approached with rigor, then we end up with bad decisions. We end up with bad science. We must actively engage in responsible debate concerning contentious issues. We must boldly address change, risk new ideas, and conflicting hypotheses, which is the proper nature of evidence-based science.”
Dr. Jason Goldman, a liaison to the ACIP for the American College of Physicians, attacked opposing viewpoints as unscientific. Goldman said the Hep B vaccine discussion was “an unnecessary solution looking for a problem.”
‘If adults won’t go for the shots, then give them to babies’
The Hep B vaccine has been universally recommended for infants since 1991. The first shot is currently given within 24 hours after birth to prevent infection with hepatitis B from mothers who carry the disease — less than 0.5% of mothers.
Mothers can be tested in the hospital to determine whether they have the disease, and current tests have a 100% accuracy rate, according to FDA ex officio ACIP participant Tracy Beth Høeg, M.D., Ph.D.
However, a 1991 New York Times article posted on Substack yesterday by Dr. Meryl Nass showed that when the universal shot was rolled out, the goal was not to prevent maternal transmission — the goal was to prevent adult cases, at a time when adult cases were deemed a national crisis. However, adults commonly didn’t get the shot.
“If adults won’t go for the shots, then give them to babies,” the article said.
Following Thursday’s meeting, legacy media attacked the committee and the CDC’s presenters and highlighted charges of misinformation by liaison members. Liaisons are nonvoting members from professional medical organizations who can offer their opinions and advice to the committee.
Representatives from some of those groups, including the American Academy of Pediatrics (AAP) and the American Medical Association, were disinvited in August from participation in the workgroups due to conflicts of interest.
Since then, the AAP has boycotted the ACIP meetings
At the start of today’s meeting, Meissner castigated AAP for this move. He said he was concerned that by not participating, they would be seen as being more focused on making a political statement than attending to the health of children.
He said that pediatricians should be part of the discussions. “Refusal to participate in the ACIP meetings does not appear to be in the best interest of children.”
Immediately following today’s vote, the Times quoted “experts” from some of the staunchest advocates for all vaccines on the childhood schedule, such as the director of the Center for Infectious Disease Research & Policy, Michael Osterholm, Ph.D., saying that the vote shows federal health authorities can no longer be trusted.
Osterholm, a member of the COVID-19 Advisory Board under the Biden administration, is one of the key players in the “Vaccine Integrity Project,” funded by iAlumbra, a nonprofit founded by Walmart heiress and philanthropist Christy Walton. The project plans to make its own vaccine recommendations.
This Substack is reader-supported.
To receive new posts and support my work, consider becoming a free or paid subscriber.
Vaccine recommendations ‘should not be treated as mandates’
During the day-and-a-half-long discussion about the Hep B vaccine, several committee members, including Dr. Evelyn Griffin, raised concerns that the birth recommendation posed challenges for informed consent, because mothers who had just delivered babies were not in a position to calmly evaluate risks and benefits.
Others, including Levi, argued that the vaccine requirements for children to attend school effectively functioned as mandates.
Liaison members universally disagreed that the recommendations were mandates and argued that ACIP recommendations were really only recommendations, and parents could do what they wanted.
CDC ex officio member, Dr. Adam Langer, who was opposed to changing the recommendation, said that the recommendations had come to function as mandates, but that was not the intention. He proposed the committee make a formal statement that “all vaccine recommendations are recommendations. They should not be treated as mandates.”
He added that mandates put in place by state and local jurisdictions were “problematic.”
“We have a lot of challenges with our culture and our traditions in this country, with telling people what they must and must not do. But that’s not what we’re saying here. We’re saying that at the population level, in the majority of cases, this is what the sign shows is the best practice.”
He said providers should always make the best decision for the individual patient they are working with. “That’s the reason why you’ve been entrusted with a license to practice medicine.”
Watch the ACIP meeting here:
Focal Points
Common Vaccines Linked to 38-50% Increased Risk of Dementia and Alzheimer’s
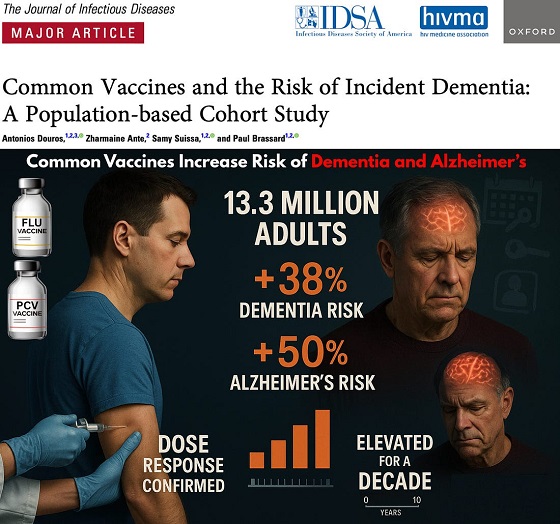
The single largest vaccine–dementia study ever conducted (n=13.3 million) finds risk intensifies with more doses, remains elevated for a full decade, and is strongest after flu and pneumococcal shots.
The single largest and most rigorous study ever conducted on vaccines and dementia — spanning 13.3 million UK adults — has uncovered a deeply troubling pattern: those who received common adult vaccines faced a significantly higher risk of both dementia and Alzheimer’s disease.
The risk intensifies with more doses, remains elevated for a full decade, and is strongest after influenza and pneumococcal vaccination. With each layer of statistical adjustment, the signal doesn’t fade — it becomes sharper, more consistent, and increasingly difficult to explain away.
And critically, these associations persisted even after adjusting for an unusually wide range of potential confounders, including age, sex, socioeconomic status, BMI, smoking, alcohol-related disorders, hypertension, atrial fibrillation, heart failure, coronary artery disease, stroke/TIA, peripheral vascular disease, diabetes, chronic kidney and liver disease, depression, epilepsy, Parkinson’s disease, cancer, traumatic brain injury, hypothyroidism, osteoporosis, and dozens of medications ranging from NSAIDs and opioids to statins, antiplatelets, immunosuppressants, and antidepressants.
Even after controlling for this extensive list, the elevated risks remained strong and remarkably stable.
Vaccinated Adults Had a 38% Higher Risk of Dementia
The primary adjusted model showed that adults receiving common adult vaccines (influenza, pneumococcal, shingles, tetanus, diphtheria, pertussis) had a:
38% increased risk of developing dementia (OR 1.38)
This alone dismantles the narrative of “vaccines protect the brain,” but the deeper findings are far worse.
Alzheimer’s Disease Risk Is Even Higher — 50% Increased Risk
Buried in the supplemental tables is a more shocking result: when the authors restricted analyses to Alzheimer’s disease specifically, the association grew even stronger.
50% increased risk of Alzheimer’s (Adjusted OR 1.50)
This indicates the effect is not random. The association intensifies for the most devastating subtype of dementia.
Clear Dose–Response Pattern: More Vaccines = Higher Risk
The authors ran multiple dose–response models, and every one of them shows the same pattern:
Dementia (all types)
From eTable 2:
- 1 vaccine dose → Adjusted OR 1.26 (26% higher risk)
- 2–3 doses → Adjusted OR 1.32 (32% higher risk)
- 4–7 doses → Adjusted OR 1.42 (42% higher risk)
- 8–12 doses → Adjusted OR 1.50 (50% higher risk)
- ≥13 doses → Adjusted OR 1.55 (55% higher risk)
Alzheimer’s Disease (AD) Shows the Same—and Even Stronger—Trend
From eTable 7:
- 1 dose → Adjusted OR 1.32 (32% higher risk)
- 2–3 doses → Adjusted OR 1.41 (41% higher risk)
- ≥4 doses → Adjusted OR 1.61 (61% higher risk)
This is one of the most powerful and unmistakable signals in epidemiology.
Time–Response Curve: Risk Peaks Soon After Vaccination and Remains Elevated for Years
Another signal strongly inconsistent with mere bias: a time-response relationship.
The highest dementia risk occurs 2–4.9 years after vaccination (Adjusted OR 1.56). The risk then slowly attenuates but never returns to baseline, remaining elevated across all time windows.
After 12.5 years, the risk is still meaningfully elevated (Adjusted OR 1.28) — a persistence incompatible with short-term “detection bias” and suggestive of a long-lasting biological impact.
This pattern is what you expect from a biological trigger with long-latency neuroinflammatory or neurodegenerative consequences.
Even After a 10-Year Lag, the Increased Risk Does Not Disappear
When the authors apply a long 10-year lag — meant to eliminate early detection bias — the elevated risk persists:
- Dementia: OR 1.20
- Alzheimer’s: OR 1.26
If this were simply “people who see doctors more often get diagnosed earlier,” the association should disappear under long lag correction.
Influenza and Pneumococcal Vaccines Drive the Signal
Two vaccines show particularly strong associations:
Influenza vaccine
- Dementia: OR 1.39 → 39% higher risk
- Alzheimer’s: OR 1.49 → 49% higher risk
Pneumococcal vaccine
- Dementia: OR 1.12 → 12% higher risk
- Alzheimer’s: OR 1.15 → 15% higher risk
And again, both exhibit dose–response escalation — the hallmark pattern of a genuine exposure–outcome relationship.
Taken together, the findings across primary, supplemental, dose–response, time–response, stratified, and sensitivity analyses paint the same picture:
• A consistent association between cumulative vaccination and increased dementia risk
• A stronger association for Alzheimer’s than for general dementia
• A dose–response effect — more vaccines, higher risk
• A time–response effect — risk peaks after exposure and persists long-term
• Influenza and pneumococcal vaccines strongly drive the signal
• The association remains after 10-year lag correction and active comparator controls
This is what a robust epidemiologic signal looks like.
In the largest single study ever conducted on vaccines and dementia, common adult vaccinations were associated with a 38% higher risk of dementia and a 50% higher risk of Alzheimer’s disease. The risk increases with more doses, persists for a decade, and is strongest for influenza and pneumococcal vaccines.
Epidemiologist and Foundation Administrator, McCullough Foundation
Support our mission: mcculloughfnd.org
Please consider following both the McCullough Foundation and my personal account on X (formerly Twitter) for further content.
FOCAL POINTS (Courageous Discourse) is a reader-supported publication.
To receive new posts and support my work, consider becoming a free or paid subscriber.
-

 Business2 days ago
Business2 days agoWhy Does Canada “Lead” the World in Funding Racist Indoctrination?
-

 Automotive2 days ago
Automotive2 days agoTrump Deals Biden’s EV Dreams A Death Blow
-

 Automotive2 days ago
Automotive2 days agoCanada’s EV Mandate Is Running On Empty
-
 Media2 days ago
Media2 days agoThey know they are lying, we know they are lying and they know we know but the lies continue
-

 Focal Points2 days ago
Focal Points2 days agoThe West Needs Bogeymen (Especially Russia)
-

 Censorship Industrial Complex1 day ago
Censorship Industrial Complex1 day agoUS Condemns EU Censorship Pressure, Defends X
-

 Dan McTeague1 day ago
Dan McTeague1 day agoWill this deal actually build a pipeline in Canada?
-
 Opinion23 hours ago
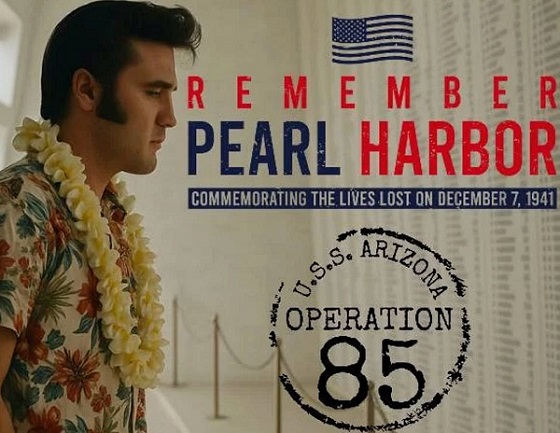
Opinion23 hours agoThe day the ‘King of rock ‘n’ roll saved the Arizona memorial














