Fraser Institute
Endless spending increases will not fix Canada’s health-care system

From the Fraser Institute
By Mackenzie Moir and Jake Fuss
Canada’s health-care system ranked as the most expensive (as a share of the economy) among 30 universal health-care countries. And despite these relatively high levels of spending, Canada continues to lag behind its peers on key indicators of performance.
In February 2023, the federal government announced the money they send to the provinces for health care would increase, yet again. Despite being billed as a fix for health care, these spending increases will not actually provide any relief for Canadian patients.
The Canada Health Transfer (CHT), the main federal financial tool for funding provincial health care, has increased from $34.0 billion in 2015/16 to $52.1 billion this year (2024/25), a 53.1 per cent increase in about a decade. Moreover, the federal government has committed to increases in the transfer at a guaranteed 5 per cent until 2027/28.
This latest increase in the CHT, however, is only one part of the $46.2 billion in new money being doled out over the next 10 years. More than half (roughly $25 billion) is currently being given to provinces who’ve signed up to work towards a number of “shared priorities” with Ottawa, such as mental health and substance abuse.
Clearly, the federal government has decided to substantially increase health-care spending in more than one way. But will it produce results?
These periodic “fixes” occasionally championed by Ottawa every few years are nothing new. And unfortunately, the data show that longstanding problems, including long waits for medical care and doctor shortages, will persist even though Canada is certainly no slouch when compared to its peers on health-care spending.
A recent study found that, when adjusted for differences in age (because older populations tend to spend more on health care), Canada’s health-care system ranked as the most expensive (as a share of the economy) among 30 universal health-care countries. And despite these relatively high levels of spending, Canada continues to lag behind its peers on key indicators of performance.
For example, Canada had some of the fewest physicians (ranked 28th of 30 countries), hospital beds (ranked 23rd of 29) and diagnostic technology such as MRIs (ranking 25th of 29 countries) and CT scanners (ranking 26th out of 30 countries) compared to other high-income countries with universal health care.
It also ranked at or near the bottom on measures such as same-day medical appointments, how easy it is to find afterhours care, and the timeliness of specialist appointments and surgical care.
And wait times have been getting worse. Just last year Canada recorded the longest ever delay for non-emergency care at 27.7 weeks, a 198 per cent increase from the 9.3 week wait experienced in 1993 (the first year national estimates were published).
But it’s not just the health-care system that’s in shambles, despite our high spending. Our federal finances are, too. Years of substantial increases in federal spending have strained the country’s finances. The Trudeau government’s latest budget projects a deficit of $39.8 billion this year, with more spent on debt interest ($54.1 billion) than on what the federal government gives to the provinces for health care.
Again, these periodic injections of federal funds to the provinces to supposedly fix health care are nothing new. Ottawa has relied on this strategy in the past and wait times have grown longer over the last three decades. Endless increases in spending will not fix our health-care system.
Authors:
Business
State of the Canadian Economy: Number of publicly listed companies in Canada down 32.7% since 2010

From the Fraser Institute
By Ben Cherniavsky and Jock Finlayson
Initial public offerings down 94% since 2010, reflecting country’s economic stagnation
Canadian equity markets are flashing red lights reflective of the larger stagnation, lack of productivity growth and lacklustre innovation of the
country’s economy, with the number of publicly listed companies down 32.7 per cent and initial public offerings down 92.5 per cent since 2010, finds a new report published Friday by the Fraser Institute, an independent, non-partisan Canadian public policy think-tank.
“Even though the value of the companies trading on Canada’s stock exchanges has risen substantially over time, there has been an alarming decrease in the number of companies listed on the exchanges as well as the number of companies choosing to go public,” said Ben Cherniavsky, co-author of Canada’s Shrinking Stock Market: Causes and Implications for Future Economic Growth.
The study finds that over the past 15 years, the number of companies listed on Canada’s two stock markets (the TSX and the TSXV) has fallen from 3,141 in 2010 to 2,114 in 2024—a 32.7 per cent decline.
Similarly, the number of new public stock listings (IPOs) on the two Canadian exchanges has also plummeted from 67 in 2010 to just four in 2024, and only three the year before.
Previous research has shown that well-functioning, diverse public stock markets are significant contributors to economic growth, higher productivity and innovation by supplying financing (i.e. money) to the business sector to enable growth and ongoing investments.
At the same time, the study also finds an explosion of investment in what’s known as private equity in Canada, increasing assets under management from $21.7 billion (US) in 2010 to over $93.1 billion (US) in 2024.
“The shift to private equity has enormous implications for average investors, since it’s difficult if not impossible for average investors to access private equity funds for their savings and investments,” explained Cherniavsky.
Crucially, the study makes several recommendations to revitalize Canada’s stagnant capital markets, including reforming Canada’s complicated regulatory regime for listed companies, scaling back corporate disclosure requirements, and pursuing policy changes geared to improving Canada’s lacklustre performance on business investment, productivity growth, and new business formation.
“Public equity markets play a vital role in raising capital for the business sector to expand, and they also provide an accessible and low-cost way for Canadians to invest in the commercial success of domestic businesses,” said Jock Finlayson, a senior fellow with the Fraser Institute and study co-author.
“Policymakers and all Canadians should be concerned by the alarming decline in the number of publicly traded companies in Canada, which risks economic stagnation and lower living standards ahead.”
Canada’s Shrinking Stock Market: Causes and Implications for Future Economic Growth
- Public equity markets are an important part of the wider financial system.
- Since the early 2000s, the number of public companies has fallen in many countries, including Canada. In 2008, for instance, Canada had 3,520 publicly traded companies on its two exchanges, compared to 2,114 in 2024.
- This trend reflects [1] the impact of mergers and acquisitions, [2] greater access to private capital, [3] increasing regulatory and governance costs facing publicly traded businesses, and [4] the growth of index investing.
- Canada’s poor business climate, including many years of lacklustre business investment and little or no productivity growth, has also contributed to the decline in stock exchange listings.
- The number of new public stock listings (IPOs) on Canadian exchanges has plummeted: between 2008 and 2013, the average was 47 per year, but this dropped to 16 between 2014 and 2024, with only 5 new listings recorded in 2024.
- At the same time, the value of private equity in Canada has skyrocketed from $12.8 billion in 2008 to $93.2 billion in 2024. These trends are concerning, as most Canadians cannot easily access private equity investment vehicles, so their domestic investment options are shrinking.
- The growth of index investing is contributing to the decline in public listings, particularly among smaller companies. In 2008, there were 1,232 listed companies on the TSX Composite and 84 exchange-traded funds; in 2024, there were only 709 listed companies on the TSX and 1,052 exchange-traded funds.
- The trends discussed in this study are also important because Canada has relied more heavily than other jurisdictions on public equity markets to finance domestic businesses.
- Revitalizing Canada’s stagnant stock markets requires policy reforms, particularly regulatory changes to reduce costs to issuers and policies to improve the conditions for private-sector investment and business growth.
Alberta
Alberta’s new diagnostic policy appears to meet standard for Canada Health Act compliance

From the Fraser Institute
By Nadeem Esmail, Mackenzie Moir and Lauren Asaad
In October, Alberta’s provincial government announced forthcoming legislative changes that will allow patients to pay out-of-pocket for any diagnostic test they want, and without a physician referral. The policy, according to the Smith government, is designed to help improve the availability of preventative care and increase testing capacity by attracting additional private sector investment in diagnostic technology and facilities.
Unsurprisingly, the policy has attracted Ottawa’s attention, with discussions now taking place around the details of the proposed changes and whether this proposal is deemed to be in line with the Canada Health Act (CHA) and the federal government’s interpretations. A determination that it is not, will have both political consequences by being labeled “non-compliant” and financial consequences for the province through reductions to its Canada Health Transfer (CHT) in coming years.
This raises an interesting question: While the ultimate decision rests with Ottawa, does the Smith government’s new policy comply with the literal text of the CHA and the revised rules released in written federal interpretations?
According to the CHA, when a patient pays out of pocket for a medically necessary and insured physician or hospital (including diagnostic procedures) service, the federal health minister shall reduce the CHT on a dollar-for-dollar basis matching the amount charged to patients. In 2018, Ottawa introduced the Diagnostic Services Policy (DSP), which clarified that the insured status of a diagnostic service does not change when it’s offered inside a private clinic as opposed to a hospital. As a result, any levying of patient charges for medically necessary diagnostic tests are considered a violation of the CHA.
Ottawa has been no slouch in wielding this new policy, deducting some $76.5 million from transfers to seven provinces in 2023 and another $72.4 million in 2024. Deductions for Alberta, based on Health Canada’s estimates of patient charges, totaled some $34 million over those two years.
Alberta has been paid back some of those dollars under the new Reimbursement Program introduced in 2018, which created a pathway for provinces to be paid back some or all of the transfers previously withheld on a dollar-for-dollar basis by Ottawa for CHA infractions. The Reimbursement Program requires provinces to resolve the circumstances which led to patient charges for medically necessary services, including filing a Reimbursement Action Plan for doing so developed in concert with Health Canada. In total, Alberta was reimbursed $20.5 million after Health Canada determined the provincial government had “successfully” implemented elements of its approved plan.
Perhaps in response to the risk of further deductions, or taking a lesson from the Reimbursement Action Plan accepted by Health Canada, the province has gone out of its way to make clear that these new privately funded scans will be self-referred, that any patient paying for tests privately will be reimbursed if that test reveals a serious or life-threatening condition, and that physician referred tests will continue to be provided within the public system and be given priority in both public and private facilities.
Indeed, the provincial government has stated they do not expect to lose additional federal health care transfers under this new policy, based on their success in arguing back previous deductions.
This is where language matters: Health Canada in their latest CHA annual report specifically states the “medical necessity” of any diagnostic test is “determined when a patient receives a referral or requisition from a medical practitioner.” According to the logic of Ottawa’s own stated policy, an unreferred test should, in theory, be no longer considered one that is medically necessary or needs to be insured and thus could be paid for privately.
It would appear then that allowing private purchase of services not referred by physicians does pass the written standard for CHA compliance, including compliance with the latest federal interpretation for diagnostic services.
But of course, there is no actual certainty here. The federal government of the day maintains sole and final authority for interpretation of the CHA and is free to revise and adjust interpretations at any time it sees fit in response to provincial health policy innovations. So while the letter of the CHA appears to have been met, there is still a very real possibility that Alberta will be found to have violated the Act and its interpretations regardless.
In the end, no one really knows with any certainty if a policy change will be deemed by Ottawa to run afoul of the CHA. On the one hand, the provincial government seems to have set the rules around private purchase deliberately and narrowly to avoid a clear violation of federal requirements as they are currently written. On the other hand, Health Canada’s attention has been aroused and they are now “engaging” with officials from Alberta to “better understand” the new policy, leaving open the possibility that the rules of the game may change once again. And even then, a decision that the policy is permissible today is not permanent and can be reversed by the federal government tomorrow if its interpretive whims shift again.
The sad reality of the provincial-federal health-care relationship in Canada is that it has no fixed rules. Indeed, it may be pointless to ask whether a policy will be CHA compliant before Ottawa decides whether or not it is. But it can be said, at least for now, that the Smith government’s new privately paid diagnostic testing policy appears to have met the currently written standard for CHA compliance.

Lauren Asaad
Policy Analyst, Fraser Institute
-

 Business1 day ago
Business1 day agoCanada Hits the Brakes on Population
-
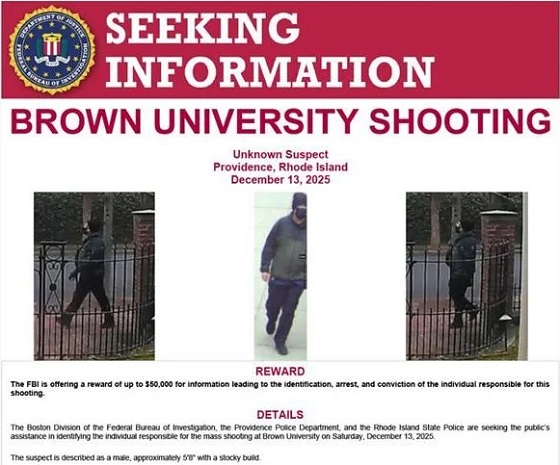
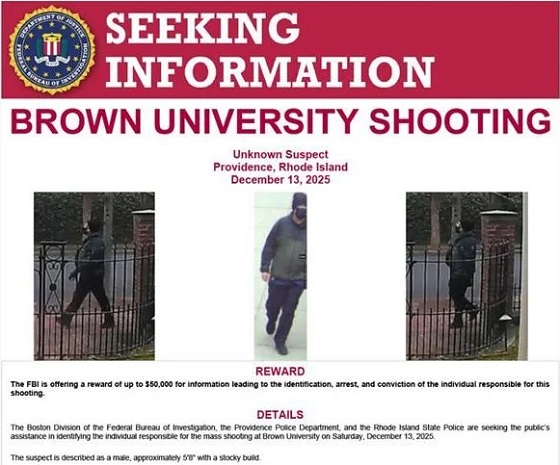 Crime19 hours ago
Crime19 hours agoBrown University shooter dead of apparent self-inflicted gunshot wound
-

 Crime2 days ago
Crime2 days agoBondi Beach Survivor Says Cops Prevented Her From Fighting Back Against Terrorists
-

 Agriculture1 day ago
Agriculture1 day agoWhy is Canada paying for dairy ‘losses’ during a boom?
-

 International2 days ago
International2 days agoHouse Rejects Bipartisan Attempt To Block Trump From Using Military Force Against Venezuela
-

 Automotive2 days ago
Automotive2 days agoFord’s EV Fiasco Fallout Hits Hard
-

 Frontier Centre for Public Policy1 day ago
Frontier Centre for Public Policy1 day agoCanada Lets Child-Porn Offenders Off Easy While Targeting Bible Believers
-

 International2 days ago
International2 days agoTOTAL AND COMPLETE BLOCKADE: Trump cuts off Venezuela’s oil lifeline