Fraser Institute
Cost of Ottawa’s gun ban fiasco may reach $6 billion

From the Fraser Institute
By Gary Mauser
According to the government, it has already spent $67.2 million, which includes compensation for 60 federal employees working on the “buyback,” which still doesn’t exist.
Four years ago, the Trudeau government banned “1,500 types” of “assault-style firearms.” It’s time to ask if public safety has improved as promised.
This ban instantly made it a crime for federally-licensed firearms owners to buy, sell, transport, import, export or use hundreds of thousands formerly legal rifles and shotguns. According to the government, the ban targets “assault-style weapons,” which are actually classic semi-automatic rifles and shotguns that have been popular with hunters and sport shooters for more than 100 years. When announcing the ban, the prime minister said the government would confiscate the banned firearms and their legal owners would be “grandfathered” or receive “fair compensation.” That hasn’t happened.
As of October 2024, the government has revealed no plans about how it will collect the newly-banned firearms nor has it made any provisions for compensation in any federal budget since the announcement in 2020. Originally, the government enacted a two-year amnesty period to allow compliance with the ban. This amnesty expired in April 2022 and has been twice extended, first to Oct. 30, 2023, then to Oct. 30, 2025.
Clearly, the ban—which the government calls a “buyback”—has been a gong show from the beginning. Since Trudeau’s announcement four years ago, virtually none of the banned firearms have been surrendered. The Ontario government refuses to divert police resources to cooperate with this federal “buyback” scheme. The RCMP’s labour union has said it’s a “misdirected effort when it comes to public safety.” The Canadian Sporting Arms & Ammunition Association, which represents firearms retailers, said it will have “zero involvement” in helping confiscate these firearms. Even Canada Post wants nothing to do with Trudeau’s “buyback” plan. And again, the government has revealed no plan for compensation—fair or otherwise.
And yet, according to the government, it has already spent $67.2 million, which includes compensation for 60 federal employees working on the “buyback,” which still doesn’t exist.
It remains unclear just how many firearms the 2020 ban includes. The Parliamentary Budget Officer estimates range between 150,000 to more than 500,000, with an estimated total value between $47 million and $756 million. These costs only include the value of the confiscated firearms and exclude the administrative costs to collect them and the costs of destroying the collected firearms. The total cost of this ban to taxpayers will be more than $4 billion and possibly more than $6 billion.
Nevertheless, while the ban of remains a confusing mess, after four years we should be able to answer one key question. Has the ban made Canadians safer?
According to Statistics Canada, firearm-related violent crime swelled by 10 per cent from 2020 to 2022 (the latest year of comparable data), from 12,614 incidents to 13,937 incidents. And in “2022, the rate of firearm-related violent crime was 36.7 incidents per 100,000 population, an 8.9% increase from 2021 (33.7 incidents per 100,000 population). This is the highest rate recorded since comparable data were first collected in 2009.”
Nor have firearm homicides decreased since 2020. Perhaps this is because lawfully-held firearms are not the problem. According to StatsCan, “the firearms used in homicides were rarely legal firearms used by their legal owners.” However, crimes committed by organized crime have increased by more than 170 per cent since 2016 (from 4,810 to 13,056 crimes).
Meanwhile, the banned firearms remain locked in the safes of their legal owners who have been vetted by the RCMP and are monitored nightly for any infractions that might endanger public safety.
Indeed, hunters and sport shooters are among the most law-abiding people in Canada. Many Canadian families and Indigenous peoples depend on hunting to provide food for the family dinner table through legal harvesting, with the added benefit of getting out in the wilderness and spending time with family and friends. In 2015, hunting and firearm businesses alone contributed more than $5.9 billion to Canada’s economy and supported more than 45,000 jobs. Hunters are the largest contributors to conservation efforts, contributing hundreds of millions of dollars to secure conservation lands and manage wildlife. The number of licensed firearms owners has increased 17 per cent since 2015 (from 2.026 million to 2.365 million) in 2023.
If policymakers in Ottawa and across the country want to reduce crime and increase public safety, they should enact policies that actually target criminals and use our scarce tax dollars wisely to achieve these goals.
Author:
Economy
Affordable housing out of reach everywhere in Canada

From the Fraser Institute
By Steven Globerman, Joel Emes and Austin Thompson
According to our new study, in 2023 (the latest year of comparable data), typical homes on the market were unaffordable for families earning the local median income in every major Canadian city
The dream of homeownership is alive, but not well. Nearly nine in ten young Canadians (aged 18-29) aspire to own a home—but share a similar worry about the current state of housing in Canada.
Of course, those worries are justified. According to our new study, in 2023 (the latest year of comparable data), typical homes on the market were unaffordable for families earning the local median income in every major Canadian city. It’s not just Vancouver and Toronto—housing affordability has eroded nationwide.
Aspiring homeowners face two distinct challenges—saving enough for a downpayment and keeping up with mortgage payments. Both have become harder in recent years.
For example, in 2014, across 36 of Canada’s largest cities, a 20 per cent downpayment for a typical home—detached house, townhouse, condo—cost the equivalent of 14.1 months (on average) of after-tax income for families earning the median income. By 2023, that figure had grown to 22.0 months—a 56 per cent increase. During the same period for those same families, a mortgage payment for a typical home increased (as a share of after-tax incomes) from 29.9 per cent to 56.6 per cent.
No major city has been spared. Between 2014 and 2023, the price of a typical home rose faster than the growth of median after-tax family income in 32 out of 36 of Canada’s largest cities. And in all 36 cities, the monthly mortgage payment on a typical home grew (again, as a share of median after-tax family income), reflecting rising house prices and higher mortgage rates.
While the housing affordability crisis is national in scope, the challenge differs between cities.
In 2023, a median-income-earning family in Fredericton, the most affordable large city for homeownership in Canada, had save the equivalent of 10.6 months of after-tax income ($56,240) for a 20 per cent downpayment on a typical home—and the monthly mortgage payment ($1,445) required 27.2 per cent of that family’s after-tax income. Meanwhile, a median-income-earning family in Vancouver, Canada’s least affordable city, had to spend the equivalent of 43.7 months of after-tax income ($235,520) for a 20 per cent downpayment on a typical home with a monthly mortgage ($6,052) that required 112.3 per cent of its after-tax income—a financial impossibility unless the family could rely on support from family or friends.
The financial barriers to homeownership are clearly greater in Vancouver. But, crucially, neither city is truly “affordable.” In Fredericton and Vancouver, as in every other major Canadian city, buying a typical home with the median income produces a debt burden beyond what’s advisable. Recent house price declines in cities such as Vancouver and Toronto have provided some relief, but homeownership remains far beyond the reach of many families—and a sharp slowdown in homebuilding threatens to limit further gains in affordability.
For families priced out of homeownership, renting doesn’t offer much relief, as rent affordability has also declined in nearly every city. In 2014, rental rates for the median-priced rental unit required 19.8 per cent of median after-tax family income, on average across major cities. By 2023, that figure had risen to 23.5 per cent. And in the least affordable cities for renters, Toronto and Vancouver, a median-priced rental required more than 30 per cent of median after-tax family income. That’s a heavy burden for Canada’s renters who typically earn less than homeowners. It’s also an added financial barrier to homeownership— many Canadian families rent for years before buying their first home, and higher rents make it harder to save for a downpayment.
In light of these realities, Canadians should ask—why have house prices and rental rates outpaced income growth?
Poor public policy has played a key role. Local regulations, lengthy municipal approval processes, and costly taxes and fees all combine to hinder housing development. And the federal government allowed a historic surge in immigration that greatly outpaced new home construction. It’s simple supply and demand—when more people chase a limited (and restricted) supply of homes, prices rise. Meanwhile, after-tax incomes aren’t keeping pace, as government policies that discourage investment and economic growth also discourage wage growth.
Canadians still want to own homes, but a decade of deteriorating affordability has made that a distant prospect for many families. Reversing the trend will require accelerated homebuilding, better-paced immigration and policies that grow wages while limiting tax bills for Canadians—changes governments routinely promise but rarely deliver.
Agriculture
Canada’s air quality among the best in the world

From the Fraser Institute
By Annika Segelhorst and Elmira Aliakbari
Canadians care about the environment and breathing clean air. In 2023, the share of Canadians concerned about the state of outdoor air quality was 7 in 10, according to survey results from Abacus Data. Yet Canada outperforms most comparable high-income countries on air quality, suggesting a gap between public perception and empirical reality. Overall, Canada ranks 8th for air quality among 31 high-income countries, according to our recent study published by the Fraser Institute.
A key determinant of air quality is the presence of tiny solid particles and liquid droplets floating in the air, known as particulates. The smallest of these particles, known as fine particulate matter, are especially hazardous, as they can penetrate deep into a person’s lungs, enter the blood stream and harm our health.
Exposure to fine particulate matter stems from both natural and human sources. Natural events such as wildfires, dust storms and volcanic eruptions can release particles into the air that can travel thousands of kilometres. Other sources of particulate pollution originate from human activities such as the combustion of fossil fuels in automobiles and during industrial processes.
The World Health Organization (WHO) and the Canadian Council of Ministers of the Environment (CCME) publish air quality guidelines related to health, which we used to measure and rank 31 high-income countries on air quality.
Using data from 2022 (the latest year of consistently available data), our study assessed air quality based on three measures related to particulate pollution: (1) average exposure, (2) share of the population at risk, and (3) estimated health impacts.
The first measure, average exposure, reflects the average level of outdoor particle pollution people are exposed to over a year. Among 31 high-income countries, Canadians had the 5th-lowest average exposure to particulate pollution.
Next, the study considered the proportion of each country’s population that experienced an annual average level of fine particle pollution greater than the WHO’s air quality guideline. Only 2 per cent of Canadians were exposed to fine particle pollution levels exceeding the WHO guideline for annual exposure, ranking 9th of 31 countries. In other words, 98 per cent of Canadians were not exposed to fine particulate pollution levels exceeding health guidelines.
Finally, the study reviewed estimates of illness and mortality associated with fine particle pollution in each country. Canada had the fifth-lowest estimated death and illness burden due to fine particle pollution.
Taken together, the results show that Canada stands out as a global leader on clean air, ranking 8th overall for air quality among high-income countries.
Canada’s record underscores both the progress made in achieving cleaner air and the quality of life our clean air supports.
-

 Censorship Industrial Complex2 days ago
Censorship Industrial Complex2 days agoUS Condemns EU Censorship Pressure, Defends X
-

 Banks2 days ago
Banks2 days agoTo increase competition in Canadian banking, mandate and mindset of bank regulators must change
-

 Dan McTeague2 days ago
Dan McTeague2 days agoWill this deal actually build a pipeline in Canada?
-
 Opinion2 days ago
Opinion2 days agoThe day the ‘King of rock ‘n’ roll saved the Arizona memorial
-
 Focal Points2 days ago
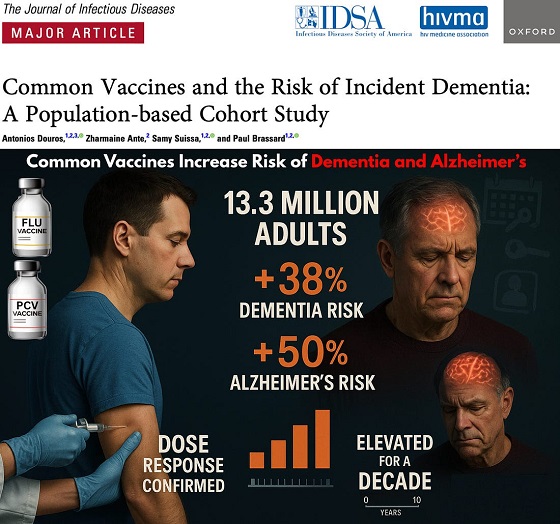
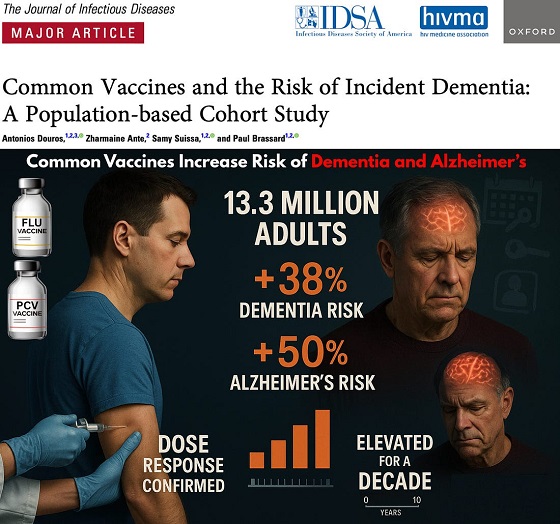
Focal Points2 days agoCommon Vaccines Linked to 38-50% Increased Risk of Dementia and Alzheimer’s
-
 espionage1 day ago
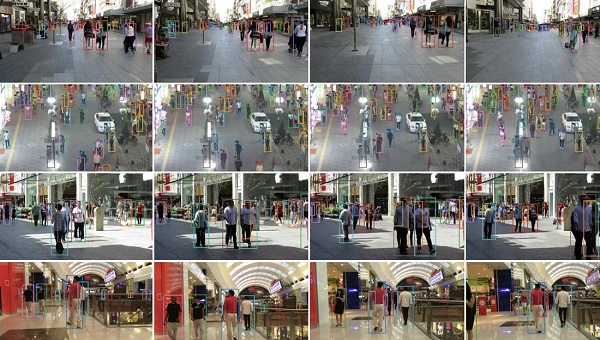
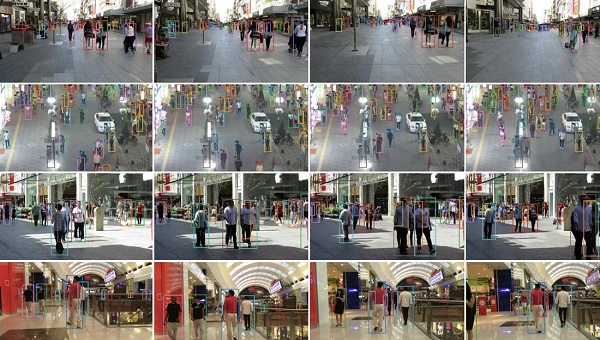
espionage1 day agoWestern Campuses Help Build China’s Digital Dragnet With U.S. Tax Funds, Study Warns
-

 Bruce Dowbiggin1 day ago
Bruce Dowbiggin1 day agoWayne Gretzky’s Terrible, Awful Week.. And Soccer/ Football.
-

 Business2 days ago
Business2 days agoLoblaws Owes Canadians Up to $500 Million in “Secret” Bread Cash















