Health
RFK Jr. appoints Robert Malone, Martin Kulldorff, other COVID shot critics to overhauled CDC vaccine panel
From LifeSiteNews
By Robert Jones
Health and Human Services Secretary Robert F. Kennedy Jr. has announced eight appointments for the CDC’s top vaccine advisory panel, following his dismissal of all 17 previous members, citing a need to rebuild public trust in the federal immunization process.
On Monday, I took a major step towards restoring public trust in vaccines by reconstituting the Advisory Committee for Immunization Practices (ACIP). I retired the 17 current members of the committee. I’m now repopulating ACIP with the eight new members who will attend ACIP’s…
— Secretary Kennedy (@SecKennedy) June 11, 2025
RFK Jr. said the new Advisory Committee on Immunization Practices (ACIP) will demand “definitive safety and efficacy data” before issuing any new vaccine recommendations and will re-evaluate existing guidance. The restructured panel is set to convene on June 25.
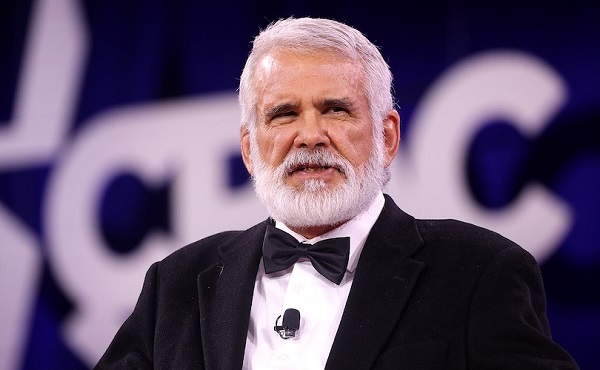
The appointees include several prominent physicians and scientists, including former Harvard epidemiologist Martin Kulldorff and mRNA researcher Robert Malone, both known for their criticism of COVID-19-era public health policy and the COVID-19 shots.
Kulldorff helped draft the Great Barrington Declaration with Jay Bhattacharya and Sunetra Gupta, which called for focused protection rather than mass lockdowns – a position widely debated among epidemiologists. He also spoke out strongly against vaccine passports and mandates, as well as mask mandates and contact tracing. He was dismissed from Harvard in 2024 because of his refusal to receive the COVID-19 injections.
Malone, who conducted early work on mRNA vaccine delivery systems, was banned from several platforms for posts deemed “misleading” during the COVID crisis. He has given related interviews on The Joe Rogan Experience and elsewhere and was reinstated on X following Elon Musk’s revision of COVID-19 policies.
Retsef Levi, a professor at MIT, has raised concerns about potential cardiovascular risks linked to COVID-19 mRNA shots and has called for stricter safety monitoring. In 2023, a petition circulated opposing his work, though it did not gain traction.
Other appointees include:
- Joseph Hibbeln, an NIH psychiatrist and nutrition researcher focused on immune and neurodevelopmental health.
- Cody Meissner, a pediatric infectious disease expert with previous experience on both FDA and CDC vaccine panels.
- James Pagano, a veteran emergency physician with decades of clinical experience.
- Vicky Pebsworth, a nurse-scientist with prior FDA vaccine advisory roles and Pacific Region Director of the National Association of Catholic Nurses. She is also a Lay Dominican.
- Michael Ross, an OB-GYN and clinical researcher with a background in immunology and women’s health policy.
Joseph R. Hibbeln, MD, is a psychiatrist and neuroscientist with a career in clinical research, public health policy, and federal service. As former Acting Chief of the Section on Nutritional Neurosciences at the National Institutes of Health, he led research on immune regulation, neurodevelopment, and mental health. His work has informed U.S. public health guidelines, particularly in maternal and child health. With more than 120 peer-reviewed publications and extensive experience in federal advisory roles, Dr. Hibbeln brings expertise in immune-related outcomes, psychiatric conditions, and evidence-based public health strategies.
Martin Kulldorff, MD, PhD, is a biostatistician and epidemiologist formerly at Harvard Medical School and a leading expert in vaccine safety and infectious disease surveillance. He has served on the Food and Drug Administration’s Drug Safety and Risk Management Advisory Committee and the CDC’s Vaccine Safety Subgroup of the Advisory Committee on Immunization Practices, where he contributed to national vaccine safety monitoring systems. Dr. Kulldorff developed widely used tools such as SaTScan and TreeScan for detecting disease outbreaks and vaccine adverse events. His expertise includes statistical methods for public health surveillance, immunization safety, and infectious disease epidemiology. He has also been an influential voice in public health policy, advocating for evidence-based approaches to pandemic response.
Retsef Levi, PhD, is the Professor of Operations Management at the MIT Sloan School of Management and a leading expert in healthcare analytics, risk management, and vaccine safety. He has served as Faculty Director of MIT Sloan’s Food Supply Chain Analytics and Sensing Initiative and co-led the Leaders for Global Operations Program. Dr. Levi has collaborated with public health agencies to evaluate vaccine safety, including co-authoring studies on mRNA COVID-19 vaccines and their association with cardiovascular risks. His research has contributed to discussions on vaccine manufacturing processes, safety surveillance, and public health policy. Dr. Levi has also served on advisory committees and engaged in policy discussions concerning vaccine safety and efficacy. His expertise spans healthcare systems optimization, epidemiologic modeling, and the application of AI and data science in public health. Dr. Levi’s work continues to inform national and international debates on immunization safety and health system resilience.
Robert W. Malone, MD, is a physician-scientist and biochemist known for his early contributions to mRNA vaccine technology. He conducted foundational research in the late 1980s on lipid-mediated mRNA delivery, which laid the groundwork for later developments in mRNA-based therapeutics. Dr. Malone has held academic positions at institutions including the University of California, Davis, and the University of Maryland, and has served in advisory roles for the U.S. Department of Health and Human Services and the Department of Defense. His expertise spans molecular biology, immunology, and vaccine development.
Cody Meissner, MD, is a Professor of Pediatrics at the Geisel School of Medicine at Dartmouth and a nationally recognized expert in pediatric infectious diseases and vaccine policy. He has served as Section Chief of Pediatric Infectious Disease at Dartmouth-Hitchcock Medical Center and has held advisory roles with both the Centers for Disease Control and Prevention (CDC) and the Food and Drug Administration (FDA). Dr. Meissner has been a voting member of the CDC’s Advisory Committee on Immunization Practices and the FDA’s Vaccines and Related Biological Products Advisory Committee, where he has contributed to national immunization guidelines and regulatory decisions. His expertise spans vaccine development, immunization safety, and pediatric infectious disease epidemiology. Dr. Meissner has also been a contributing author to American Academy of Pediatrics policy statements and immunization schedules, helping shape national standards for pediatric care.
James Pagano, MD, is a board-certified Emergency Medicine physician with over 40 years of clinical experience following his residency at UCLA. He has worked in diverse emergency settings, from Level 1 trauma centers to small community hospitals, caring for patients across all age groups, including infants, pregnant women, and the elderly. Dr. Pagono served on multiple hospital committees, including utilization review, critical care, and medical executive boards. He is strong advocate for evidence-based medicine.
Vicky Pebsworth, OP, PhD, RN, earned a doctorate in public health and nursing from the University of Michigan. She has worked in the healthcare field for more than 45 years, serving in various capacities, including critical care nurse, healthcare administrator, health policy analyst, and research scientist with a focus on public health policy, bioethics, and vaccine safety. She is the Pacific Region Director of the National Association of Catholic Nurses. She is a former member of the Food and Drug Administration’s Vaccine and Related Biological Products Advisory Committee and the National Vaccine Advisory Committee’s 2009 H1N1 Vaccine Safety Risk Assessment Working Group and Vaccine Safety Working Group (Epidemiology and Implementation Subcommittees).
Michael A. Ross, MD, is a Clinical Professor of Obstetrics and Gynecology at George Washington University and Virginia Commonwealth University, with a career spanning clinical medicine, research, and public health policy. He has served on the CDC’s Advisory Committee for the Prevention of Breast and Cervical Cancer, where he contributed to national strategies for cancer prevention and early detection, including those involving HPV immunization. With research experience in hormone therapies, antibiotic trials, and immune-related conditions such as breast cancer prevention, Dr. Ross has engaged in clinical investigations with immunologic relevance. He has advised major professional organizations, including the American College of Obstetricians and Gynecologists, and contributed to federal advocacy efforts around women’s health and preventive care. His continued service on biotech and healthcare boards reflects his commitment to advancing innovation in immunology, reproductive medicine, and public health.
Kennedy framed the move as part of a broader campaign to remove conflicts of interest and restore credibility to federal vaccine recommendations. Just a few days ago, he accused the panel of having been “little more than a rubber stamp for any vaccine” and pledged that the new members would not have direct ties with the vaccine industry.
The new ACIP, he said, will be focused on what RFK called “gold-standard science” and “common sense.” The June meeting will mark the beginning of its work.
Agriculture
“We Made it”: Healthy Ostriches Still Alive in Canada

Looks like we made it. For another weekend at least. Until sanity settles down into the head into the head of the federal government that remains fixated on the killing of 399 healthy ostriches. As the clock wound down today, an announcement from the farm proclaimed, “We made it today,” calling it another “miracle Friday.”
WATCH TODAY’S Miracle Friday Announcement
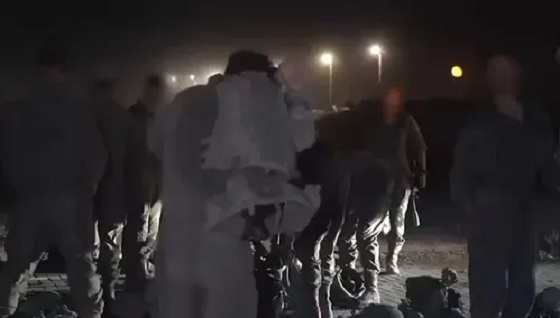
Earlier in the day, Rebel News’ Drea Humphrey reported, “There’s apparently a SWAT team up the road, I hope that doesn’t mean they’ve gotten bad news,” wondering “if the police were preparing to aid the CFIA in the cull.”
Dacey Media reported that the farm said that “Ostrich Hunters” were also spotted at Universal Ostrich Farms according to Katie Pasitney The “kill pen” is fully set up and CFIA have been luring ostriches into it.
But as of 5:30 ET, it seems the farm and the ostriches may have escaped to live another day as the Supreme Court of Canada (SCC) did not hand down a decision to grant a further leave to the farm to prepare its case, or dismiss the case, allowing the Canadian Food Inspection Agency (CFIA) to proceed with their “cull” to kill 399 healthy ostriches.
The palpable, raw government over-reach that includes over 100 Royal Canadian Mounted Police (RCMP) that have occupied the farm highlights the mismanagement of the CFIA and may be one of the reasons that the SCC has hesitated in making a decision before the weekend.
Call to Dismantle the CFIA
On today’s Stand on Guard interview Katie Pastiney, spokeswoman for the Universal Ostrich Farms in British Columbia called for the dismantlement of the Canadian Food Inspection Agency. She says that the CFIA:
“Needs to be dismantled and we need to rebuild this organization back up from the ground up and we need to have a new vision.
“We need to have a new mission and a brand-new face for Canadians that will give us hope that we will be protected not attacked.”
“The Canadian Food Inspection Agency continues to overuse their authority, overuse their excessive freedom that they’ve been given, and they have zero accountability for their actions.”
The farm has been embroiled in a dispute with the federal government and its CFIA agency for close to a year. The agency claims the flock of ostriches has the avian flu, but it refuses to test the farmers’ birds, even though they have been healthy for 258 days. At the same time the CFIA will not let the farmers pay for the tests themselves, saying they will charge them $250,000 per ostrich and put them in jail for 6 months.
The federal agency and the RCMP have seized and occupied the farm since September 22, 2025. they have conducted a campaign of harassment of the farm family and their flock of ostriches that included: arresting the farmers when they were told to go feed their birds; using lights and heavy equipment at night’; sending drones to chase the birds that resulted in pushing one bird over the fence so it hurt its leg, not treating the animals properly; and not feeding the ostriches full rations of food and water and not treating the birds the CFIA injured. These activities have continued as the CFIA continues to construct a “kill box” of hay bales that have been on fire four times while under the CFIA’s supervision and occupation.
Running Out of Time
In a stunning report on X October 2nd, however, before the Supreme Court of Canada had made decision, the CFIA has daily continued to move forward to kill the ostriches ignoring the SCC legal “stay.”
Karen Esperson, Pasitney’s mother yesterday reported on X:
“We need to put CFIA in check.
“This organization feels they are greater than the Supreme Court of Canada. they are still positioning the birds and putting them in the position to be killed immediately. They are assuming they know the outcome of the Supreme Court oof Canada. Do they think they are better than the Supreme court? That they are going to for sure win?
“The Supreme Court has not decided.
“What is happening?
“We are on a stay order and yet I just got a call that they have a whole bunch of birds herded in a little circle in the kill pen.
“Waiting. This is animal cruelty.”
Efforts to Save the Ostriches
More and more Members of Parliament have been speaking up on behalf of the farmers including the local provincial representative, the local Member of Parliament Scott Anderson, who visited the farm trying to talk to the CFIA and also the Official Leader of the Opposition Pierre Poilievre spek out yesterday.
A second press conference hosted by John Catsimatidis, a New York radio host, billionaire and friend of Donald Trump and Dr. Oz, was also held yesterday. The USA Trump administration representatives including Robert F. Kennedy say they want to either pay for the ostrich testing or help re-locate them to the United States for further research opportunities. This outreach has been ignored.
CFIA Has Staff Enough to Kill but NOT Enough Staff to Test?
In my interview today with Pastiney she explained how the CFIA did originally give their ostrich farm an exemption that was later rescinded because the CFIA told them they were “understaffed and we’re not able to perform these tests.”
“There was an exemption package that was given to us on January 2nd. We have an email from Canadian Food Inspection Agency stating that we qualify for special rare genetics within our herd and that we could be exempt.
“Now when we followed through with that because we needed to test them just to show their DNA and their genetics and show their lineage that between January 2nd and January 10th something happened.
“Now we didn’t qualify we lost that right.
“And on January 10th they said sorry you don’t qualify for special rare genetics because we are understaffed and we’re not able to perform these tests.”
Why does the CFIA have staff to occupy the farm for weeks and to kill 399 ostriches as well as requisition the Royal Canadian Mounted Police (RCMP) over 40 cars and reportedly more than 100 police on the farm since September 22nd, and not have the money to test the birds for the exemption?
How much has this debacle and exercise into Carney Government overreach been charged to Canadian taxpayers?
More than the tests to see if the ostriches are healthy or if they qualify for the exemption?
Other Farmers May Join in Efforts to Disband the CFIA
Pastiney says:
“I just did an interview with a farmer that this very same thing happened to them and it was based off a suspicion of tuberculosis outbreak on their farm.
“They [the farmers] had over 600 head of cattle, they had sheep, they had goats, they had pig or pigs, they had chickens.
“They [the CFIA] came in based off suspicion and off their own negligence they killed everything this beautiful older farm had to find out in the end that they tested after everything was dead and there was no tuberculosis.”
“I asked her a very important question, and I said could you trust this organization again? And she said, absolutely not.
“So, it became very clear to me after this about talking to two or three farmers that the Canadian Food Inspection Agency needs to be dismantled.”
“It is an organization that has lost the trust of Canadians.
CONCLUSION
WATCH Katie is Fighting For Everyone’s Freedom | Stand on Guard
www.kraydensrightnews.com is a reader-supported publication.
To receive new posts and support my work, consider becoming a free or paid subscriber.
Health
Disabled man needs help as hospital continues to pressure him with assisted suicide

From LifeSiteNews
Roger Foley has been pressured to consider euthanasia while being denied adequate care, prompting a new campaign to cover his medical costs and support his fight to return home.
Roger Foley, an Ontario man, has been forced to turn to charity after being denied sufficient care from hospitals which continue to push euthanasia on him.
On September 30, the Life Care Network launched a LifeFunder to cover medical costs for Roger Foley, a disabled Canadian who is struggling to receive support in an Ontario hospital which is encouraging him to end his life with Medical Assistance in Dying (MAiD).
“Hospital staff have repeatedly offered and pressured me to consider Canada’s infamous assisted suicide program Medical Assistance in Dying (MAiD) while simultaneously obstructing the very services and supports I need to live safely,” Foley revealed in a write-up for the fundraiser.
“Despite my condition, I have fought tirelessly for my rights, dignity, and the ability to return to the community,” he continued.
Foley, who is well known for speaking out against the injustice of Canada’s euthanasia regime, suffers from spinocerebellar ataxia, an incurable brain disease that makes it difficult to move.
As a result of his, he requires caregivers to assist him in eating, drinking, and getting up. According to Foley, his caregivers mistreated him while caring for him at his home. In 2016, Foley was admitted to the London Health Sciences Centre (LHSC) in Ontario for food poisoning and has been there ever since.
Foley revealed that over the past nine years he has repeatedly been offered MAiD despite his desire to be released from the hospital and return home with the help of caregivers.
In May, Foley began enduring even more pain when the LHSC switched out the amber lights in his room for bright bulbs. Foley, who is light sensitive, is now in so much pain that he is unable to be lifted for meals.
“I can only tolerate fluids for a few minutes at a time using makeshift taped-together ski goggles. I am unable to eat solid food or take oral medications,” Foley explained.
“I live in constant pain, severe fatigue, and cognitive decline from dehydration and lack of sleep,” he continued. “Staff continue to impose arbitrary and unsafe ‘rules,’ including denying me side rails during transfers and barging in with bright lights – despite knowing it causes me extreme harm.”
Now Foley is seeking private funding for a Personal Support Worker to assist him with feeding, medication, hydration, and basic hygiene support. Life Care Network, an organization which assists vulnerable Canadians at risk for MAiD, has intervened to raise the necessary funds for Foley’s care.
In an interview with LifeSiteNews, Lino DeFacendis, founder and CEO of Life Care Network, stressed the importance of defending Foley from a medical system which appears to prioritize ending his life with MAiD over providing proper care.
“There needs to be a re-awakening that every life is precious and must be treated with true dignity and compassion no matter how difficult the circumstance,” DeFacendis said.
“Killing oneself via MAiD is never the answer to one’s problems,” he declared.
To support Foley’s medical care, please visit his LifeFunder page.
-

 Alberta2 days ago
Alberta2 days agoFact, fiction, and the pipeline that’s paying Canada’s rent
-

 Business1 day ago
Business1 day agoTrump Warns Beijing Of ‘Countermeasures’ As China Tightens Grip On Critical Resources
-

 International1 day ago
International1 day agoTrump gets an honourable mention: Nobel winner dedicates peace prize to Trump
-

 Business19 hours ago
Business19 hours agoCarney government plans to muddy the fiscal waters in upcoming budget
-
 Alberta2 days ago
Alberta2 days agoAlberta Is Where Canadians Go When They Want To Build A Better Life
-
 International2 days ago
International2 days agoTrump-brokered Gaza peace agreement enters first phase
-

 Crime1 day ago
Crime1 day agoCanada’s safety minister says he has not met with any members of damaged or destroyed churches
-

 COVID-191 day ago
COVID-191 day agoTamara Lich says she has no ‘remorse,’ no reason to apologize for leading Freedom Convoy














