Alberta
Red Deer recovery community slated for fall completion

Construction on the 75-bed recovery community project in Red Deer is on time and on budget and is expected to be completed this fall.
The Red Deer recovery community is a first-of-its-kind project in Alberta that will house a long-term addiction treatment program focused on helping people pursue recovery.
Currently 52 of 72 modular buildings are on site. The installation of mechanical and electrical systems as well as work on the building interiors are scheduled to get underway later this month. The final modular buildings will be arriving soon.
“Alberta’s government is making sure that every Albertan has the opportunity to pursue recovery from the devastating and destructive illness of addiction. I am pleased that this project is on time to start operations in the fall so that Albertans can begin their recovery as soon as possible.”
“Alberta Infrastructure plays a key role in delivering this essential project. Our goal is to have this facility up and running as soon as possible to bring more jobs and specialized care to the people of Red Deer.”
“Addiction and mental health challenges have taken a significant toll on central Alberta over the past decade. Increasing treatment capacity in Red Deer is long overdue. Alberta’s government is proud to make this investment to save lives, support recovery and bring hope to the community of Red Deer.”
“The Red Deer recovery community will be an important part of the recovery-oriented system of care that we are building in Red Deer to help people improve their lives. Our government is proud to invest in projects like this to build up our communities and bring more jobs to Albertans.”
“It is essential that our community have access to quality mental health care. This project will not only expand access to addictions treatment for those in need, but it will also bring jobs to our city and help boost our economic recovery.”
Recovery communities are a form of long-term residential treatment that focus on supporting people who are pursuing recovery. Recovery is seen as a gradual, ongoing process of behavioural change through clinical and peer interventions aimed at improving a person’s overall well-being.
Alberta’s government is helping Albertans access life-saving addiction and mental health-related prevention, intervention, treatment and recovery resources.

Quick facts
- This project is keeping Albertans working, supporting about 135 well-paid construction and construction-related jobs.
- Alberta Health is in the process of opening four recovery community projects.
- Red Deer (75-bed facility)
- Construction slated for fall completion.
- Lethbridge (50-bed facility)
- Groundbreaking took place in May 2022 and the project is on schedule to be completed in late 2022.
- Gunn (100-bed facility)
- The project is in the design stage. Construction and completion dates will be determined as the project progresses.
- Blood Tribe (75-bed facility)
- The project is in the planning phase.
- Red Deer (75-bed facility)
- Contact Alberta 211 for information about addiction treatments and supports available throughout the province.
- Albertans struggling with opioid use anywhere in the province can call the Virtual Opioid Dependency Program seven days a week at 1-844-383-7688 to access same-day treatment.
- Albertans using substances at home alone can download the DORS app to a smartphone free of charge from any app store or via DORSApp.ca. When using the app, Albertans will receive a call from the STARS emergency centre if they become unresponsive to a timer. If an overdose is suspected, STARS will immediately dispatch emergency medical services to the person’s location.
Alberta
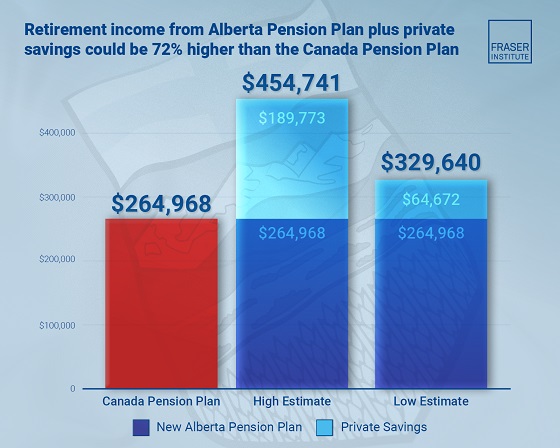
Median workers in Alberta could receive 72% more under Alberta Pension Plan compared to Canada Pension Plan
From the Fraser Institute
By Tegan Hill and Joel Emes
Moving from the CPP to a provincial pension plan would generate savings for Albertans in the form of lower contribution rates (which could be used to increase private retirement savings while receiving the same pension benefits as the CPP under the new provincial pension), finds a new study published today by the Fraser Institute, an independent, non-partisan Canadian public policy think-tank.
“Due to Alberta’s comparatively high rates of employment, higher average incomes, and younger population, Albertans would pay a lower contribution rate through a separate provincial pension plan while receiving the same benefits as under the CPP,” said Tegan Hill, director of Alberta policy at the Fraser Institute and co-author of Illustrating the Potential of an Alberta Pension Plan.
Assuming Albertans invested the savings from moving to a provincial pension plan into a private retirement account, and assuming a contribution rate of 5.85 per cent, workers earning the median income in Alberta ($53,061 in 2025) could accrue a stream of retirement payments totalling $454,741 (pre-tax)—a 71.6 per cent increase from their stream of CPP payments ($264,968).
Put differently, under the CPP, a median worker receives a total of $264,968 in retirement income over their life. If an Alberta worker saved the difference between what they pay now into the CPP and what they would pay into a new provincial plan, the income they would receive in retirement increases. If the contribution rate for the new provincial plan was 5.85 per cent—the lower of the available estimates—the increase in retirement income would total $189,773 (or an increase of 71.6 per cent).
If the contribution rate for a new Alberta pension plan was 8.21 per cent—the higher of the available estimates—a median Alberta worker would still receive an additional $64,672 in retirement income over their life, a marked increase of 24.4 per cent compared to the CPP alone.
Put differently, assuming a contribution rate of 8.21 per cent, Albertan workers earning the median income could accrue a stream of retirement payments totaling $329,640 (pre-tax) under a provincial pension plan—a 24.4 per cent increase from their stream of CPP payments.
“While the full costs and benefits of a provincial pension plan must be considered, its clear that Albertans could benefit from higher retirement payments under a provincial pension plan, compared to the CPP,” Hill said.
Illustrating the Potential of an Alberta Pension Plan
- Due to Alberta’s comparatively high rates of employment, higher average incomes, and younger population, Albertans would pay a lower contribution rate with a separate provincial pension plan, compared with the CPP, while receiving the same benefits as under the CPP.
- Put differently, moving from the CPP to a provincial pension plan would generate savings for Albertans, which could be used to increase private retirement income. This essay assesses the potential savings for Albertans of moving to a provincial pension plan. It also estimates an Albertan’s potential increase in total retirement income, if those savings were invested in a private account.
- Depending on the contribution rate used for an Alberta pension plan (APP), ranging from 5.85 to 8.2 percent, an individual earning the CPP’s yearly maximum pensionable earnings ($71,300 in 2025), would accrue a stream of retirement payments under the total APP (APP plus private retirement savings), yielding a total retirement income of between $429,524 and $584,235. This would be 22.9 to 67.1 percent higher, respectively, than their stream of CPP payments ($349,545).
- An individual earning the median income in Alberta ($53,061 in 2025), would accrue a stream of retirement payments under the total APP (APP plus private retirement savings), yielding a total retirement income of between $329,640 and $454,741, which is between 24.4 percent to 71.6 percent higher, respectively, than their stream of CPP payments ($264,968).

Joel Emes
Alberta
Alberta ban on men in women’s sports doesn’t apply to athletes from other provinces

From LifeSiteNews
Alberta’s Fairness and Safety in Sport Act bans transgender males from women’s sports within the province but cannot regulate out-of-province transgender athletes.
Alberta’s ban on gender-confused males competing in women’s sports will not apply to out-of-province athletes.
In an interview posted July 12 by the Canadian Press, Alberta Tourism and Sport Minister Andrew Boitchenko revealed that Alberta does not have the jurisdiction to regulate out-of-province, gender-confused males from competing against female athletes.
“We don’t have authority to regulate athletes from different jurisdictions,” he said in an interview.
Ministry spokeswoman Vanessa Gomez further explained that while Alberta passed legislation to protect women within their province, outside sporting organizations are bound by federal or international guidelines.
As a result, Albertan female athletes will be spared from competing against men during provincial competition but must face male competitors during inter-provincial events.
In December, Alberta passed the Fairness and Safety in Sport Act to prevent biological men who claim to be women from competing in women’s sports. The legislation will take effect on September 1 and will apply to all school boards, universities, as well as provincial sports organizations.
The move comes after studies have repeatedly revealed what almost everyone already knew was true, namely, that males have a considerable advantage over women in athletics.
Indeed, a recent study published in Sports Medicine found that a year of “transgender” hormone drugs results in “very modest changes” in the inherent strength advantages of men.
Additionally, male athletes competing in women’s sports are known to be violent, especially toward female athletes who oppose their dominance in women’s sports.
Last August, Albertan male powerlifter “Anne” Andres was suspended for six months after a slew of death threats and harassments against his female competitors.
In February, Andres ranted about why men should be able to compete in women’s competitions, calling for “the Ontario lifter” who opposes this, apparently referring to powerlifter April Hutchinson, to “die painfully.”
Interestingly, while Andres was suspended for six months for issuing death threats, Hutchinson was suspended for two years after publicly condemning him for stealing victories from women and then mocking his female competitors on social media. Her suspension was later reduced to a year.
-

 Business24 hours ago
Business24 hours agoMark Carney’s Fiscal Fantasy Will Bankrupt Canada
-

 Business2 days ago
Business2 days agoCarney government should apply lessons from 1990s in spending review
-

 Entertainment2 days ago
Entertainment2 days agoStudy finds 99% of late-night TV guests in 2025 have been liberal
-

 Alberta23 hours ago
Alberta23 hours agoTemporary Alberta grid limit unlikely to dampen data centre investment, analyst says
-

 Opinion1 day ago
Opinion1 day agoCharity Campaigns vs. Charity Donations
-

 Frontier Centre for Public Policy2 days ago
Frontier Centre for Public Policy2 days agoCanada’s New Border Bill Spies On You, Not The Bad Guys
-

 Daily Caller19 hours ago
Daily Caller19 hours ago‘Strange Confluence Of Variables’: Mike Benz Wants Transparency Task Force To Investigate What Happened in Butler, PA
-

 Uncategorized2 days ago
Uncategorized2 days agoCNN’s Shock Climate Polling Data Reinforces Trump’s Energy Agenda



