Brownstone Institute
Covid was Spreading Across the U.S. in 2019

BY
If it could be proven that the virus that causes COVID-19 was spreading throughout the world by November 2019 (or even earlier), the shift in the Covid narrative might be seismic.
For example, if the virus had already infected large numbers of people, the justification for the lockdowns of mid-March 2020 to “slow or stop the spread” of a newly arrived virus would be shown to be nonsense.
Estimates of the number of people who had already developed natural immunity as well as of the infection fatality rate (IFR) might be dramatically different. It would suggest the disease was not nearly as lethal as experts proclaimed. The mass fear in the public – a prerequisite for lockdowns and later for mass vaccinations – might be much lower.
Given these points, it’s odd public health officials and investigative journalists have eschewed serious investigations that might confirm this virus had already spread around the world before January 1st, 2020.
A common-sense project to ‘prove’ early spread was occurring would be simply to test tranches of blood that were donated before the birth date of the official outbreak (December 31st 2019).
Surprisingly, however, very few antibody studies of archived blood collected before December 31st 2019 have occurred. Will Jones of The Daily Skeptic recently highlighted one such study published by researchers in France as well as a sewage study from Brazil. The first provides antibody evidence and the second RNA evidence the novel coronavirus was spreading by November 2019 in these countries.
To Will’s list, I’d add the only antibody study of archived Red Cross blood conducted by the US CDC to date. This study found 39 antibody-positive serum samples collected December 13th-16th, 2019 in California, Washington and Oregon (2% of blood samples collected from these states tested positive for antibodies).
As it takes the human body one to two weeks to produce detectable levels of antibodies, most of these 39 antibody-positive donors had been infected in November 2019 if not earlier.
For some reason, American officials performed only one antibody study of blood collected by blood bank organizations. It’s also strange that results of this study were not published until November 30th, 2020 – more than 11 months after the first tranche of archived Red Cross blood had been collected.
In a CDC press briefing held May 29th, 2020, CDC officials stated they’d searched for and could find no evidence the novel coronavirus had been “introduced” anywhere in America prior to January 20th, 2020.
I believe this statement was false, as by the time this press briefing was held, copious evidence of early spread had already been disseminated via published news accounts. For example, I’ve identified at least 17 Americans who were sick with definite Covid symptoms in November and December 2019 and all 17 had antibody evidence of prior infection. Also, all 17 of these reports were published by prominent news organizations at least 13 days before this press conference.
While a source of important evidence, antibody studies are not necessary to prove that early spread almost certainly occurred in America. Close examination of individual case histories also allows one confidently to reach this conclusion. What follows is a summary of three individual histories that lead me to conclude community spread was already occurring in America by November 2019 and probably October 2019.
For details on other American cases that date to December 2019, see this Seattle Times story and a feature story I wrote that, for some reason, was completely ignored by the mainstream press and public health officials, a fact I document in this follow-up article.
Case 1: Michael Melham of Belleville, NJ
Michael Melham, the Mayor of Belleville, NJ, was among a large group of New Jersey municipal employees who attended a conference in Atlantic City on November 19th-21st 2019. While at the conference, Melham experienced symptoms common to COVID-19.
“I was definitely feeling sick when I was there, and fought my way through it,” Mayor Melham told NJ Advance Media on April 30th, 2020.
“I have never been sicker in my entire life,” the Mayor said. “These symptoms included a 102-degree fever, chills, hallucinations and a sore throat that lasted for three weeks.” In a story published by Fox News, Mayor Melham said the illness made him feel “like a heroin addict going through withdrawals… I didn’t know what was happening to me. I never felt that I could be so sick.“
Mayor Melham felt sick enough to contact his doctor who diagnosed him with the flu. However, this diagnosis was given “over the phone” and Melham never actually received a flu test.
In late April 2020, Melham visited his doctor for his annual physical and brought up his November illness. The doctor administered an antibody test, which came back positive for Covid antibodies.
Melham later told me he actually received two positive antibody tests (previous reports mentioned just one).
“My first antibody test was a rapid test. My second was a blood test that was sent to a lab. Both were positive for the longer antibody,” Mayor Melham wrote in one email.
Mayor Melham has repeatedly made the important (if ignored) point that he tested positive for the ‘long’ (IgG) antibody. He tested negative for the IgM antibody. The presence of IgM antibodies indicate more recent infection and, per studies, these antibodies fade and are only detectable for about a month after infection.
This combination of antibody results would seem to rule out the possibility Mayor Melham experienced an asymptomatic case of Covid in the month before receiving his first antibody test. The only time Melham was sick was November 2020.
He added: “I will also tell you that since the media attention surrounding my claim, many others have come forward. I have emails from those who were actually at the same conference in Atlantic City NJ, who became just as sick as I was.”
Those who wish to gauge the credibility of the Mayor’s claims can view this four-minute YouTube interview with Mayor Melham.
I also asked Mayor Melham a question no other journalist seems to have asked him. “Did any public health official ever contact you to investigate your possible case?”
Melham’s email response: “No, nothing.”
DISCUSSION
Multiple acquaintances as well as his physician would confirm Melham was sick with symptoms common to Covid victims in November. Since he received two positive antibody tests, if the results were a false positive, he received two false positives.
As noted, Mayor Melham reports receiving emails from “multiple people… who were at the same conference who became just as sick as I was”. This would suggest the presence of community spread – a possibility which might have been confirmed if contact tracers had tested the people who’d been sick at the same conference for antibodies.
We know no public health officials contacted Mayor Melham to investigate his claim. We also know, thanks to nj.com‘s reporting, that state health officials were aware of his claim:
“Asked about the Mayor’s statements, the state health department declined comment. A spokesperson for Gov. Phil Murphy did not immediately respond to a message.”
The following points should also be emphasized. If his diagnosis had been confirmed by public health officials, Mayor Melham would have been the first known Covid case in the world, and would have been the first confirmed case in America by approximately 61 days (the first official case in America is still recorded as January 20th, 2020 – a man from Washington state who had recently returned from Wuhan).
Significantly, Mayor Melham can date the onset of his symptoms. Per numerous studies, it takes two to 14 days after infection for symptoms to manifest. This means Mayor Melham would have been infected some time between November 5th and November 19th, 2019.
Since Mayor Melham did not give the virus to himself, logic tells us the chain of transmission that ended with Michael Melham being symptomatic around November 20th, 2019 very possibly began before November 1st, 2019. This would mean that community spread was possibly occurring in New Jersey as early as October 2019.
Case 2: Uf Tukel of Delray Beach, Florida
As reported by the Palm Beach Post on May 16th, 2020:
“At least 11 people… on two small blocks alone… in a small Delray Beach (Florida) neighborhood tested positive for coronavirus antibodies in April. They felt symptoms as early as November (2019). “It didn’t have a name back then, but I have no doubt now that it was the coronavirus,” one neighbor said.”
The article names seven of these individuals and provides details and quotes about their symptoms. These seven people include Uf Tukel who was “first among (residents of the neighborhood) to feel sick in late November (2019)… For weeks, he had body aches, a severe cough and night sweats.”
While “Tukel is reluctant to say he had the coronavirus a month before Chinese officials reported the outbreak to the World Health Organisation, ‘I had all the symptoms though,’ Tukel said.”
The same logic applied to Michael Melham’s possible case would apply to Mr. Tukel’s possible case. That is, the unknown person who infected Mr. Tukel was infected earlier than Tukel, and the unknown person who infected this person contracted the virus even earlier, suggesting early spread was also happening by some point in November, if not October, in Delray Beach, Florida.
If confirmed, Mr. Tukel’s case would indicate that American cases in November were not isolated to the state of New Jersey.
Several other points included in the Post’s coverage deserve attention.
These possible Delray Beach cases include two couples, with one spouse presumably infecting the other. One child of one of these couples became infected, providing further evidence of community spread.
According to the story, none of the individuals experienced close contacts with other non-family residents of the same neighborhood. That is, there seems to be no evidence of neighbor-to-neighbor transmission.
According to the story, “all (11 individuals) recovered and haven’t been sick since.” None of the 11 had travelled to China.
Like Michael Melham, none of these 11 people tested positive for the ‘short’ (IgM) antibodies – thus none had been recently infected.
The Post article also includes this eye-opening information: “Since March (2020) about two-fifths (approximately 200, 40%) of the 500 antibody tests taken by Xera Med (a DelRay Beach private testing lab/medical clinic) have been positive, said CEO Emily Rentz.” The first two confirmed cases in Florida were recorded March 1st.
The following sentence from this article might be even more significant: “The lab shares its data on positive tests with the state health department, (Rentz) added.”
And from the same article: “The state wouldn’t say whether it is collecting antibody data from hospitals or private laboratories.”
The Post article referenced a May 5th article by the same newspaper:
“In Florida, health department reports show patients who eventually tested positive for the virus experienced symptoms as early as January. The Florida Department of Health hasn’t explained those potential fault lines in the state’s assertion that the first cases didn’t appear in Florida until March.”
The fact 40% of 500 antibody tests administered by the clinic between March and early May 2020 tested positive for Covid antibodies suggests infections were widespread in this community. And according to the CEO of this lab, these antibody results were being shared with Florida State Department of Health officials.
And apparently these weren’t the only positive antibody results that were being reported by testing labs. As reported in the same article:
The University of Miami, in randomly testing Miami-Dade County residents for antibodies, has found that the rate of infection could be 16 times higher than state data suggests, said Dr. Erin Kobetz, a professor and lead researcher on the project …
“Since first publishing her findings, Kobetz has heard from several people who shared experiences similar to the Tropic Isle neighbors… They described being sick in December and later testing positive for antibodies. They asked if what they’d experienced was COVID-19.”
Significantly, if we count possible December 2019 cases, Americans from five geographically-dispersed US states were featured in published articles. An unknown number of Americans who’ve never been featured in a newspaper article undoubtedly fit the same profile. If one adds this unknown number of never-identified people to the list of known individuals, evidence the novel coronavirus was spreading widely across America in November and December 2019 becomes even more compelling.
Not every infectious disease expert agrees with the CDC’s assessment that widespread transmission did not begin until January 20th, 2020.
“It’s possible that the disease spread as early as November,” Dr. Kobetz said.
As in New Jersey, apparently no official with the Florida Department of Health contacted any of the 11 people referenced in the Post’s article. Nor have public health officials apparently followed up with Emily Renz, CEO of Xera Med, who stated approximately 200 other local residents received positive Covid antibody tests at the clinic between March and the end of April.
Ms. Renz noted that information on all of these positive test results had been forwarded to officials at the state’s health agency. Which prompts this question: How many clinics and testing labs in America also forwarded positive antibody test results to state health agencies, agencies which presumably could and would pass this information along to their colleagues at the CDC or NIH?
What the public doesn’t know but should is how many other Americans – those with lab results not reported in the press – also tested positive for antibodies between March and early May 2020. Presumably, the CDC and state and local health agencies have these data, which have never been released to the public.
Indeed, I’ve come to believe it’s possible at least some high-ranking officials may have conspired to suppress antibody results which, if published, might have led the public to conclude this virus was spreading widely months before officials said it had been introduced in this country. Such knowledge might have changed the way tens of millions of Americans evaluated their personal Covid risk as well as their support for lockdowns.
Case 3: Shane from Marin County, California
Perhaps the first early case in America (with antibody evidence that would confirm infection) is Shane of Marin County, California. Shane’s possible early case was not featured in a newspaper article, but by Shane himself in the reader comments section that followed a May 7th 2020 New York Times story (the story describes symptoms experienced by Covid patients).
Writes Shane: “I had COVID-19 last fall, far earlier than anyone else I’ve heard of. I suspect I caught it while on an overseas trip to Italy and the Middle East – I’ve taken two antibody tests in the past month, both of which confirmed I was infected.”
As Shane recounts, he was extremely sick with signature Covid symptoms.
“For me the worst symptom by far was the dry, unproductive cough. The cough was so intense, so relentless, it left me with bruised ribs and a horrible searing pain in my chest, which also felt as if someone were sitting on it. The fever at one point reached 104.9 upon which I began hallucinating – seeing my dogs talking to me and forgetting how to open a sliding glass door. Horrible chills which led to my teeth chattering so hard my jaw ached were also another noxious gift of Covid.
“What I most remember about my experience with Covid is pain, pain from coughing, pain in my body and head, pain everywhere around me, like a smothering red blanket. At times I felt I was going to die during that week and even today I must admit I am surprised I didn’t.”
Adding credibility to his claim, Shane’s post cited two labs where he claims to have received his positive antibody tests.
“The local health centre in West Marin is where I took the latest one. The other one I took directly at the manufacturer’s location – ARCpoint Labs in Richmond. That one is only 87% accurate and not FDA approved so that’s why I took the more recent one, which was done through Quest Labs I believe.”
In the comment thread, one poster suggests it’s unlikely Shane developed Covid as there had been no reported confirmed cases from that time. This poster opines that Shane was sick with some other nasty virus and later developed an asymptomatic case of Covid. However, Shane stuck to his theory and presented reasons for his opinion.
“I suppose it’s possible but I tend to think that since what I contracted had the exact same symptoms as COVID-19 – that COVID-19 is what I had. In addition, mid-February through mid-March I was in isolation, caring for my sister who died mid-March from metastatic cervical cancer. When COVID-19 made its first appearance in the U.S. in February we very quickly put in strict isolation protocols as my sister had a compromised immune system due to chemotherapy, further insulating myself from contact and infection as well.”
Shane does not report what month he thinks he had Covid – only that it was “last fall… and far earlier than anyone else I’ve heard.” He could have been sick in November or October (maybe even late September). Shane (if he really had Covid) contracted the virus from an unknown person who would have been infected earlier than him.
Shane shared his belief he might have contracted the virus in Italy or in the Middle East, which, if true, would provide more evidence of early global spread. However, it’s also possible he contracted the virus in California.
Shane’s claim was posted in the moderated New York Times’ comments section, meaning one or more Times employees were aware of Shane’s startling claim. I imagine any Covid article, including the popular reader comments, published by the New York Times was also read by at least some employees of the CDC, NIH etc.
As only paid subscribers can make comments in the New York Times comment section, the newspaper possesses Shane’s subscription information. That is, someone at the newspaper could have easily ascertained Shane’s full name and contact information, including his street and email address.
For what it’s worth, I contacted the NY Times via its news tip email address and suggested a reporter follow up on Shane’s eye-opening claim. I did not receive a reply. This leads me to believe the New York Times is not interested in pursuing evidence of early spread in America, even in the case of a person who very well could be the first known Covid case in the world.
Conclusion
At least three Americans (either known, or in Shane’s case, easily identifiable if effort was made) possessed antibody evidence of Covid in November 2019. The infection chain that ultimately produced these symptomatic individuals likely traces to October 2019. Of note, two of these individuals received two positive antibody tests, making a false positive explanation far less likely. These cases occurred not in one state, but three states (New Jersey, Florida and California). Americans from at least 12 US states had antibody evidence of infection prior to mid-January 2020.
As far as I know, none of these 123 Americans (17 Americans identified in press reports and 106 in the Red Cross antibody study) had travelled to China. All 123 are either known or could be identified. (For unstated reasons, the CDC did not interview any of the 106 Americans who provided positive blood samples to the Red Cross.) The figure 123 does not include the unknown individuals who infected these Americans, nor does it include the possible cases that never became known to reporters or the public.
This antibody evidence strongly suggests the novel coronavirus was being transmitted person-to-person throughout the United States well before January 1st, 2020, and was probably occurring by October 2019.
If certain officials concealed this truth or were simply too incompetent to figure it out, any trust placed in such authorities is undermined. The above information also suggests that officials are not interested in conducting serious investigations into early spread of the virus, prompting a skeptic to wonder why this might be the case.
My hope is that journalists with more resources than myself, as well as officials and scientists, will belatedly and seriously investigate the strangely-ignored evidence of early spread.
This story also appeared in The Daily Skeptic.
Brownstone Institute
The Unmasking of Vaccine Science

From the Brownstone Institute
By
I recently purchased Aaron Siri’s new book Vaccines, Amen. As I flipped though the pages, I noticed a section devoted to his now-famous deposition of Dr Stanley Plotkin, the “godfather” of vaccines.
I’d seen viral clips circulating on social media, but I had never taken the time to read the full transcript — until now.
Siri’s interrogation was methodical and unflinching…a masterclass in extracting uncomfortable truths.
A Legal Showdown
In January 2018, Dr Stanley Plotkin, a towering figure in immunology and co-developer of the rubella vaccine, was deposed under oath in Pennsylvania by attorney Aaron Siri.
The case stemmed from a custody dispute in Michigan, where divorced parents disagreed over whether their daughter should be vaccinated. Plotkin had agreed to testify in support of vaccination on behalf of the father.
What followed over the next nine hours, captured in a 400-page transcript, was extraordinary.
Plotkin’s testimony revealed ethical blind spots, scientific hubris, and a troubling indifference to vaccine safety data.
He mocked religious objectors, defended experiments on mentally disabled children, and dismissed glaring weaknesses in vaccine surveillance systems.
A System Built on Conflicts
From the outset, Plotkin admitted to a web of industry entanglements.
He confirmed receiving payments from Merck, Sanofi, GSK, Pfizer, and several biotech firms. These were not occasional consultancies but long-standing financial relationships with the very manufacturers of the vaccines he promoted.
Plotkin appeared taken aback when Siri questioned his financial windfall from royalties on products like RotaTeq, and expressed surprise at the “tone” of the deposition.
Siri pressed on: “You didn’t anticipate that your financial dealings with those companies would be relevant?”
Plotkin replied: “I guess, no, I did not perceive that that was relevant to my opinion as to whether a child should receive vaccines.”
The man entrusted with shaping national vaccine policy had a direct financial stake in its expansion, yet he brushed it aside as irrelevant.
Contempt for Religious Dissent
Siri questioned Plotkin on his past statements, including one in which he described vaccine critics as “religious zealots who believe that the will of God includes death and disease.”
Siri asked whether he stood by that statement. Plotkin replied emphatically, “I absolutely do.”
Plotkin was not interested in ethical pluralism or accommodating divergent moral frameworks. For him, public health was a war, and religious objectors were the enemy.
He also admitted to using human foetal cells in vaccine production — specifically WI-38, a cell line derived from an aborted foetus at three months’ gestation.
Siri asked if Plotkin had authored papers involving dozens of abortions for tissue collection. Plotkin shrugged: “I don’t remember the exact number…but quite a few.”
Plotkin regarded this as a scientific necessity, though for many people — including Catholics and Orthodox Jews — it remains a profound moral concern.
Rather than acknowledging such sensitivities, Plotkin dismissed them outright, rejecting the idea that faith-based values should influence public health policy.
That kind of absolutism, where scientific aims override moral boundaries, has since drawn criticism from ethicists and public health leaders alike.
As NIH director Jay Bhattacharya later observed during his 2025 Senate confirmation hearing, such absolutism erodes trust.
“In public health, we need to make sure the products of science are ethically acceptable to everybody,” he said. “Having alternatives that are not ethically conflicted with foetal cell lines is not just an ethical issue — it’s a public health issue.”
Safety Assumed, Not Proven
When the discussion turned to safety, Siri asked, “Are you aware of any study that compares vaccinated children to completely unvaccinated children?”
Plotkin replied that he was “not aware of well-controlled studies.”
Asked why no placebo-controlled trials had been conducted on routine childhood vaccines such as hepatitis B, Plotkin said such trials would be “ethically difficult.”
That rationale, Siri noted, creates a scientific blind spot. If trials are deemed too unethical to conduct, then gold-standard safety data — the kind required for other pharmaceuticals — simply do not exist for the full childhood vaccine schedule.
Siri pointed to one example: Merck’s hepatitis B vaccine, administered to newborns. The company had only monitored participants for adverse events for five days after injection.
Plotkin didn’t dispute it. “Five days is certainly short for follow-up,” he admitted, but claimed that “most serious events” would occur within that time frame.
Siri challenged the idea that such a narrow window could capture meaningful safety data — especially when autoimmune or neurodevelopmental effects could take weeks or months to emerge.
Siri pushed on. He asked Plotkin if the DTaP and Tdap vaccines — for diphtheria, tetanus and pertussis — could cause autism.
“I feel confident they do not,” Plotkin replied.
But when shown the Institute of Medicine’s 2011 report, which found the evidence “inadequate to accept or reject” a causal link between DTaP and autism, Plotkin countered, “Yes, but the point is that there were no studies showing that it does cause autism.”
In that moment, Plotkin embraced a fallacy: treating the absence of evidence as evidence of absence.
“You’re making assumptions, Dr Plotkin,” Siri challenged. “It would be a bit premature to make the unequivocal, sweeping statement that vaccines do not cause autism, correct?”
Plotkin relented. “As a scientist, I would say that I do not have evidence one way or the other.”
The MMR
The deposition also exposed the fragile foundations of the measles, mumps, and rubella (MMR) vaccine.
When Siri asked for evidence of randomised, placebo-controlled trials conducted before MMR’s licensing, Plotkin pushed back: “To say that it hasn’t been tested is absolute nonsense,” he said, claiming it had been studied “extensively.”
Pressed to cite a specific trial, Plotkin couldn’t name one. Instead, he gestured to his own 1,800-page textbook: “You can find them in this book, if you wish.”
Siri replied that he wanted an actual peer-reviewed study, not a reference to Plotkin’s own book. “So you’re not willing to provide them?” he asked. “You want us to just take your word for it?”
Plotkin became visibly frustrated.
Eventually, he conceded there wasn’t a single randomised, placebo-controlled trial. “I don’t remember there being a control group for the studies, I’m recalling,” he said.
The exchange foreshadowed a broader shift in public discourse, highlighting long-standing concerns that some combination vaccines were effectively grandfathered into the schedule without adequate safety testing.
In September this year, President Trump called for the MMR vaccine to be broken up into three separate injections.
The proposal echoed a view that Andrew Wakefield had voiced decades earlier — namely, that combining all three viruses into a single shot might pose greater risk than spacing them out.
Wakefield was vilified and struck from the medical register. But now, that same question — once branded as dangerous misinformation — is set to be re-examined by the CDC’s new vaccine advisory committee, chaired by Martin Kulldorff.
The Aluminium Adjuvant Blind Spot
Siri next turned to aluminium adjuvants — the immune-activating agents used in many childhood vaccines.
When asked whether studies had compared animals injected with aluminium to those given saline, Plotkin conceded that research on their safety was limited.
Siri pressed further, asking if aluminium injected into the body could travel to the brain. Plotkin replied, “I have not seen such studies, no, or not read such studies.”
When presented with a series of papers showing that aluminium can migrate to the brain, Plotkin admitted he had not studied the issue himself, acknowledging that there were experiments “suggesting that that is possible.”
Asked whether aluminium might disrupt neurological development in children, Plotkin stated, “I’m not aware that there is evidence that aluminum disrupts the developmental processes in susceptible children.”
Taken together, these exchanges revealed a striking gap in the evidence base.
Compounds such as aluminium hydroxide and aluminium phosphate have been injected into babies for decades, yet no rigorous studies have ever evaluated their neurotoxicity against an inert placebo.
This issue returned to the spotlight in September 2025, when President Trump pledged to remove aluminium from vaccines, and world-leading researcher Dr Christopher Exley renewed calls for its complete reassessment.
A Broken Safety Net
Siri then turned to the reliability of the Vaccine Adverse Event Reporting System (VAERS) — the primary mechanism for collecting reports of vaccine-related injuries in the United States.
Did Plotkin believe most adverse events were captured in this database?
“I think…probably most are reported,” he replied.
But Siri showed him a government-commissioned study by Harvard Pilgrim, which found that fewer than 1% of vaccine adverse events are reported to VAERS.
“Yes,” Plotkin said, backtracking. “I don’t really put much faith into the VAERS system…”
Yet this is the same database officials routinely cite to claim that “vaccines are safe.”
Ironically, Plotkin himself recently co-authored a provocative editorial in the New England Journal of Medicine, conceding that vaccine safety monitoring remains grossly “inadequate.”
Experimenting on the Vulnerable
Perhaps the most chilling part of the deposition concerned Plotkin’s history of human experimentation.
“Have you ever used orphans to study an experimental vaccine?” Siri asked.
“Yes,” Plotkin replied.
“Have you ever used the mentally handicapped to study an experimental vaccine?” Siri asked.
“I don’t recollect…I wouldn’t deny that I may have done so,” Plotkin replied.
Siri cited a study conducted by Plotkin in which he had administered experimental rubella vaccines to institutionalised children who were “mentally retarded.”
Plotkin stated flippantly, “Okay well, in that case…that’s what I did.”
There was no apology, no sign of ethical reflection — just matter-of-fact acceptance.
Siri wasn’t done.
He asked if Plotkin had argued that it was better to test on those “who are human in form but not in social potential” rather than on healthy children.
Plotkin admitted to writing it.
Siri established that Plotkin had also conducted vaccine research on the babies of imprisoned mothers, and on colonised African populations.
Plotkin appeared to suggest that the scientific value of such studies outweighed the ethical lapses—an attitude that many would interpret as the classic ‘ends justify the means’ rationale.
But that logic fails the most basic test of informed consent. Siri asked whether consent had been obtained in these cases.
“I don’t remember…but I assume it was,” Plotkin said.
Assume?
This was post-Nuremberg research. And the leading vaccine developer in America couldn’t say for sure whether he had properly informed the people he experimented on.
In any other field of medicine, such lapses would be disqualifying.
A Casual Dismissal of Parental Rights
Plotkin’s indifference to experimenting on disabled children didn’t stop there.
Siri asked whether someone who declined a vaccine due to concerns about missing safety data should be labelled “anti-vax.”
Plotkin replied, “If they refused to be vaccinated themselves or refused to have their children vaccinated, I would call them an anti-vaccination person, yes.”
Plotkin was less concerned about adults making that choice for themselves, but he had no tolerance for parents making those choices for their own children.
“The situation for children is quite different,” said Plotkin, “because one is making a decision for somebody else and also making a decision that has important implications for public health.”
In Plotkin’s view, the state held greater authority than parents over a child’s medical decisions — even when the science was uncertain.
The Enabling of Figures Like Plotkin
The Plotkin deposition stands as a case study in how conflicts of interest, ideology, and deference to authority have corroded the scientific foundations of public health.
Plotkin is no fringe figure. He is celebrated, honoured, and revered. Yet he promotes vaccines that have never undergone true placebo-controlled testing, shrugs off the failures of post-market surveillance, and admits to experimenting on vulnerable populations.
This is not conjecture or conspiracy — it is sworn testimony from the man who helped build the modern vaccine program.
Now, as Health Secretary Robert F. Kennedy, Jr. reopens long-dismissed questions about aluminium adjuvants and the absence of long-term safety studies, Plotkin’s once-untouchable legacy is beginning to fray.
Republished from the author’s Substack
Brownstone Institute
Bizarre Decisions about Nicotine Pouches Lead to the Wrong Products on Shelves

From the Brownstone Institute
A walk through a dozen convenience stores in Montgomery County, Pennsylvania, says a lot about how US nicotine policy actually works. Only about one in eight nicotine-pouch products for sale is legal. The rest are unauthorized—but they’re not all the same. Some are brightly branded, with uncertain ingredients, not approved by any Western regulator, and clearly aimed at impulse buyers. Others—like Sweden’s NOAT—are the opposite: muted, well-made, adult-oriented, and already approved for sale in Europe.
Yet in the United States, NOAT has been told to stop selling. In September 2025, the Food and Drug Administration (FDA) issued the company a warning letter for offering nicotine pouches without marketing authorization. That might make sense if the products were dangerous, but they appear to be among the safest on the market: mild flavors, low nicotine levels, and recyclable paper packaging. In Europe, regulators consider them acceptable. In America, they’re banned. The decision looks, at best, strange—and possibly arbitrary.
What the Market Shows
My October 2025 audit was straightforward. I visited twelve stores and recorded every distinct pouch product visible for sale at the counter. If the item matched one of the twenty ZYN products that the FDA authorized in January, it was counted as legal. Everything else was counted as illegal.
Two of the stores told me they had recently received FDA letters and had already removed most illegal stock. The other ten stores were still dominated by unauthorized products—more than 93 percent of what was on display. Across all twelve locations, about 12 percent of products were legal ZYN, and about 88 percent were not.
The illegal share wasn’t uniform. Many of the unauthorized products were clearly high-nicotine imports with flashy names like Loop, Velo, and Zimo. These products may be fine, but some are probably high in contaminants, and a few often with very high nicotine levels. Others were subdued, plainly meant for adult users. NOAT was a good example of that second group: simple packaging, oat-based filler, restrained flavoring, and branding that makes no effort to look “cool.” It’s the kind of product any regulator serious about harm reduction would welcome.
Enforcement Works
To the FDA’s credit, enforcement does make a difference. The two stores that received official letters quickly pulled their illegal stock. That mirrors the agency’s broader efforts this year: new import alerts to detain unauthorized tobacco products at the border (see also Import Alert 98-06), and hundreds of warning letters to retailers, importers, and distributors.
But effective enforcement can’t solve a supply problem. The list of legal nicotine-pouch products is still extremely short—only a narrow range of ZYN items. Adults who want more variety, or stores that want to meet that demand, inevitably turn to gray-market suppliers. The more limited the legal catalog, the more the illegal market thrives.
Why the NOAT Decision Appears Bizarre
The FDA’s own actions make the situation hard to explain. In January 2025, it authorized twenty ZYN products after finding that they contained far fewer harmful chemicals than cigarettes and could help adult smokers switch. That was progress. But nine months later, the FDA has approved nothing else—while sending a warning letter to NOAT, arguably the least youth-oriented pouch line in the world.
The outcome is bad for legal sellers and public health. ZYN is legal; a handful of clearly risky, high-nicotine imports continue to circulate; and a mild, adult-market brand that meets European safety and labeling rules is banned. Officially, NOAT’s problem is procedural—it lacks a marketing order. But in practical terms, the FDA is punishing the very design choices it claims to value: simplicity, low appeal to minors, and clean ingredients.
This approach also ignores the differences in actual risk. Studies consistently show that nicotine pouches have far fewer toxins than cigarettes and far less variability than many vapes. The biggest pouch concerns are uneven nicotine levels and occasional traces of tobacco-specific nitrosamines, depending on manufacturing quality. The serious contamination issues—heavy metals and inconsistent dosage—belong mostly to disposable vapes, particularly the flood of unregulated imports from China. Treating all “unauthorized” products as equally bad blurs those distinctions and undermines proportional enforcement.
A Better Balance: Enforce Upstream, Widen the Legal Path
My small Montgomery County survey suggests a simple formula for improvement.
First, keep enforcement targeted and focused on suppliers, not just clerks. Warning letters clearly change behavior at the store level, but the biggest impact will come from auditing distributors and importers, and stopping bad shipments before they reach retail shelves.
Second, make compliance easy. A single-page list of authorized nicotine-pouch products—currently the twenty approved ZYN items—should be posted in every store and attached to distributor invoices. Point-of-sale systems can block barcodes for anything not on the list, and retailers could affirm, once a year, that they stock only approved items.
Third, widen the legal lane. The FDA launched a pilot program in September 2025 to speed review of new pouch applications. That program should spell out exactly what evidence is needed—chemical data, toxicology, nicotine release rates, and behavioral studies—and make timely decisions. If products like NOAT meet those standards, they should be authorized quickly. Legal competition among adult-oriented brands will crowd out the sketchy imports far faster than enforcement alone.
The Bottom Line
Enforcement matters, and the data show it works—where it happens. But the legal market is too narrow to protect consumers or encourage innovation. The current regime leaves a few ZYN products as lonely legal islands in a sea of gray-market pouches that range from sensible to reckless.
The FDA’s treatment of NOAT stands out as a case study in inconsistency: a quiet, adult-focused brand approved in Europe yet effectively banned in the US, while flashier and riskier options continue to slip through. That’s not a public-health victory; it’s a missed opportunity.
If the goal is to help adult smokers move to lower-risk products while keeping youth use low, the path forward is clear: enforce smartly, make compliance easy, and give good products a fair shot. Right now, we’re doing the first part well—but failing at the second and third. It’s time to fix that.
-

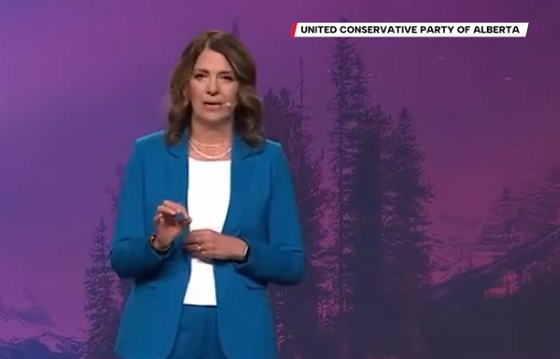
 Alberta2 days ago
Alberta2 days agoThis new Canada–Alberta pipeline agreement will cost you more than you think
-

 Energy2 days ago
Energy2 days agoUnceded is uncertain
-

 Automotive2 days ago
Automotive2 days agoPower Struggle: Governments start quietly backing away from EV mandates
-

 Business19 hours ago
Business19 hours agoCanada’s climate agenda hit business hard but barely cut emissions
-

 Energy1 day ago
Energy1 day agoCanada following Europe’s stumble by ignoring energy reality
-

 MAiD1 day ago
MAiD1 day agoFrom Exception to Routine. Why Canada’s State-Assisted Suicide Regime Demands a Human-Rights Review
-

 Great Reset2 days ago
Great Reset2 days agoCanada’s MAiD (State Sanctioned Murder) Report Just Dropped
-

 Business1 day ago
Business1 day agoCarney government should privatize airports—then open airline industry to competition