Community
LOCAL AUTHOR ASKS; DOES ANYONE EVER REALLY DIE FROM SUICIDE?
Celebrity Ricki Lake posted on her Instagram on February 14th.
“It is with a heavy heart that I share that my beloved soulmate, Christian Evans has passed. He succumbed to his life long struggle with bipolar disorder.”
Instantly I knew what she meant. And how she felt.
And then the flood of comments, mostly support; love, best wishes, sorry for your loss. But as all of us entangled in this complicated world of mental illness and/or addiction know the lack of understanding or compassion towards our loved one will rear its ugly head.
Instantly I began reading, “Selfish” and “No one dies from bipolar.” I stopped reading, after all I know how it goes.
I disagree. People do die every day from bipolar disorder and other illnesses. Personally, I don’t think anyone dies from suicide.
I have spent my entire life surrounded by alcohol addiction, it is on many branches of my family tree. Just like Ricki Lake, I loved someone very much that struggled in this life but lost his brave battle in March of 2012.
I spent over six years, six long painful years obsessed and determined to save my younger brother from addiction, he and I both making many mistakes along the way. In 2005, this had become such a crazy, out of control story, that I started keeping notes, I didn’t think anyone would believe this could happen from “just alcohol.”
While most stories of it’s kind give you just a partial glimpse, it has always been my intent to tell the WHOLE story, without shame, beginning at childhood. We know now, and what I didn’t know then, is that childhood trauma and/or sexual abuse can cause anxiety, depression, more severe mental health issues, alcohol, drug addiction and yes, even suicidal ideation. Proudly my memoir, The Sun is Gone, was just released and instantly hit #1 on Amazon.
For a small town girl, having grown up in Red Deer and now living just minutes away in Sylvan Lake I am blissfully proud. Within a couple days I got my first newspaper interview, after all I can’t do this without the support of the media, and I am on my way! Yippee! My brother Brett and I together are going to save lives. Create a conversation. Eliminate the shame and stigma. And help families. The article was published the very next day.
I got to the second sentence and lost my breath…ENDED WITH HIS SUICIDE. What? His suicide?!
Those simple words threw me off. And I started to cry. I spent over three years writing, a girl on a mission; calculated and precise. I knew exactly how I wanted to tell this story. It was always my intent that no one know the ending in advance. Not because I am hiding or ashamed or trying to pull a fast one, but rather allowing everyone to experience our journey, just as we did. What it really “feels” like while also giving knowledge, courage, encouraging compassion, empathy and most importantly, hope.
The world health organization estimates that over a million people die from suicide each year. 30,000 in the USA and 3800 in Canada. As long as we continue to zoom in on just that “one word” we will not be looking in the right direction, losing sight of the issue at hand; the causes and help for depression, anxiety, bipolar, borderline personality disorder, addiction and all the other things that lead to someone taking their own life.
I have watched a loved one pass away from Cancer. Taking what was once a strong, energetic, virile man that would eventually be confined to a hospital bed, unable to speak, with feeding tubes, weight loss and he became a shell of what was once a man. When his heart finally could not take it anymore, no one would ever say that he died from heart failure.
My brother did not die from Suicide.
My brother died a slow, painful, agonizing death from Alcoholism. Did he take his own life? Yes. But that does not change that fact. Had my brother found sobriety, and help for mental health issues, he would still be anxious, uncomfortable and have to find the strength within himself to work through his pain. He would have had complicated struggles with family and all of life’s difficulties that we all have. But he would be alive.
And had Ricki Lake’s beloved ex-husband, not struggled with bipolar, he would be alive too.
Jodee Prouse is a Speaker and outspoken advocate to eliminating the shame and stigma surrounding Addiction and Mental Illness. She is the author of the Amazon best seller, The Sun is Gone: A Sister Lost in Secrets, Shame, and Addiction, and How I Broke Free. Visit jodeeprouse.com to learn more.
Community
SPARC Red Deer – Caring Adult Nominations open now!

Red Deer community let’s give a round of applause to the incredible adults shaping the future of our kids. Whether they’re a coach, neighbour, teacher, mentor, instructor, or someone special, we want to know about them!
Tell us the inspiring story of how your nominee is helping kids grow up great. We will honour the first 100 local nominees for their outstanding contributions to youth development. It’s time to highlight those who consistently go above and beyond!
To nominate, visit Events (sparcreddeer.ca)

Addictions
‘Harm Reduction’ is killing B.C.’s addicts. There’s got to be a better way

From the Frontier Centre for Public Policy
B.C. recently decriminalized the possession of small amounts of illicit drugs. The resulting explosion of addicts using drugs in public spaces, including parks and playgrounds, recently led the province’s NDP government to attempt to backtrack on this policy
Fuelled by the deadly manufactured opioid fentanyl, Canada’s national drug overdose rate stood at 19.3 people per 100,000 in 2022, a shockingly high number when compared to the European Union’s rate of just 1.8. But national statistics hide considerable geographic variation. British Columbia and Alberta together account for only a quarter of Canada’s population yet nearly half of all opioid deaths. B.C.’s 2022 death rate of 45.2/100,000 is more than double the national average, with Alberta close behind at 33.3/100,00.
In response to the drug crisis, Canada’s two western-most provinces have taken markedly divergent approaches, and in doing so have created a natural experiment with national implications.
B.C. has emphasized harm reduction, which seeks to eliminate the damaging effects of illicit drugs without actually removing them from the equation. The strategy focuses on creating access to clean drugs and includes such measures as “safe” injection sites, needle exchange programs, crack-pipe giveaways and even drug-dispensing vending machines. The approach goes so far as to distribute drugs like heroin and cocaine free of charge in the hope addicts will no longer be tempted by potentially tainted street drugs and may eventually seek help.
But safe-supply policies create many unexpected consequences. A National Post investigation found, for example, that government-supplied hydromorphone pills handed out to addicts in Vancouver are often re-sold on the street to other addicts. The sellers then use the money to purchase a street drug that provides a better high — namely, fentanyl.
Doubling down on safe supply, B.C. recently decriminalized the possession of small amounts of illicit drugs. The resulting explosion of addicts using drugs in public spaces, including parks and playgrounds, recently led the province’s NDP government to attempt to backtrack on this policy — though for now that effort has been stymied by the courts.
According to Vancouver city councillor Brian Montague, “The stats tell us that harm reduction isn’t working.” In an interview, he calls decriminalization “a disaster” and proposes a policy shift that recognizes the connection between mental illness and addiction. The province, he says, needs “massive numbers of beds in treatment facilities that deal with both addictions and long-term mental health problems (plus) access to free counselling and housing.”
In fact, Montague’s wish is coming true — one province east, in Alberta. Since the United Conservative Party was elected in 2019, Alberta has been transforming its drug addiction policy away from harm reduction and towards publicly-funded treatment and recovery efforts.
Instead of offering safe-injection sites and free drugs, Alberta is building a network of 10 therapeutic communities across the province where patients can stay for up to a year, receiving therapy and medical treatment and developing skills that will enable them to build a life outside the drug culture. All for free. The province’s first two new recovery centres opened last year in Lethbridge and Red Deer. There are currently over 29,000 addiction treatment spaces in the province.
This treatment-based strategy is in large part the work of Marshall Smith, current chief of staff to Alberta’s premier and a former addict himself, whose life story is a testament to the importance of treatment and recovery.
The sharply contrasting policies of B.C. and Alberta allow a comparison of what works and what doesn’t. A first, tentative report card on this natural experiment was produced last year in a study from Stanford University’s network on addiction policy (SNAP). Noting “a lack of policy innovation in B.C.,” where harm reduction has become the dominant policy approach, the report argues that in fact “Alberta is currently experiencing a reduction in key addiction-related harms.” But it concludes that “Canada overall, and B.C. in particular, is not yet showing the progress that the public and those impacted by drug addiction deserve.”
The report is admittedly an early analysis of these two contrasting approaches. Most of Alberta’s recovery homes are still under construction, and B.C.’s decriminalization policy is only a year old. And since the report was published, opioid death rates have inched higher in both provinces.
Still, the early returns do seem to favour Alberta’s approach. That should be regarded as good news. Society certainly has an obligation to try to help drug users. But that duty must involve more than offering addicts free drugs. Addicted people need treatment so they can kick their potentially deadly habit and go on to live healthy, meaningful lives. Dignity comes from a life of purpose and self-control, not a government-funded fix.
Susan Martinuk is a senior fellow at the Frontier Centre for Public Policy and author of the 2021 book Patients at Risk: Exposing Canada’s Health Care Crisis. A longer version of this article recently appeared at C2CJournal.ca.
-

 COVID-1911 hours ago
COVID-1911 hours agoCDC Quietly Admits to Covid Policy Failures
-
 Brownstone Institute59 mins ago
Brownstone Institute59 mins agoDeborah Birx Gets Her Close-Up
-
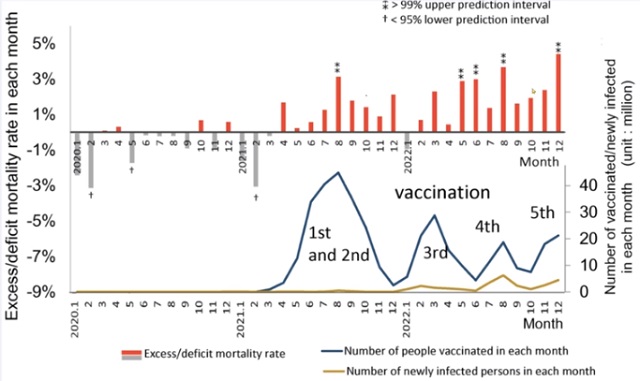
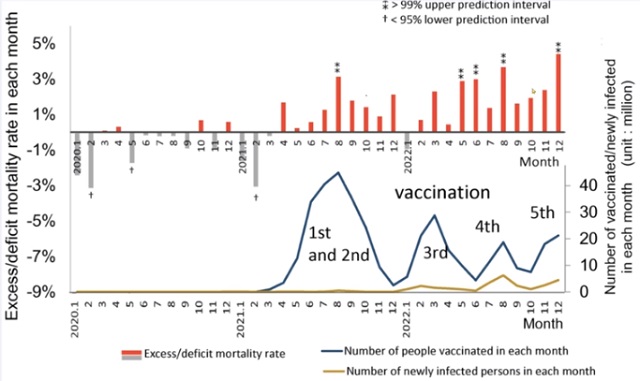 COVID-1914 hours ago
COVID-1914 hours agoJapanese study shows disturbing increase in cancer related deaths during the Covid pandemic
-

 Great Reset9 hours ago
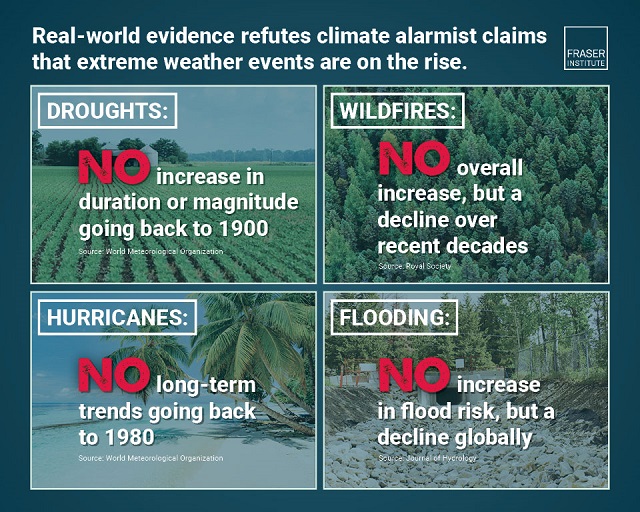
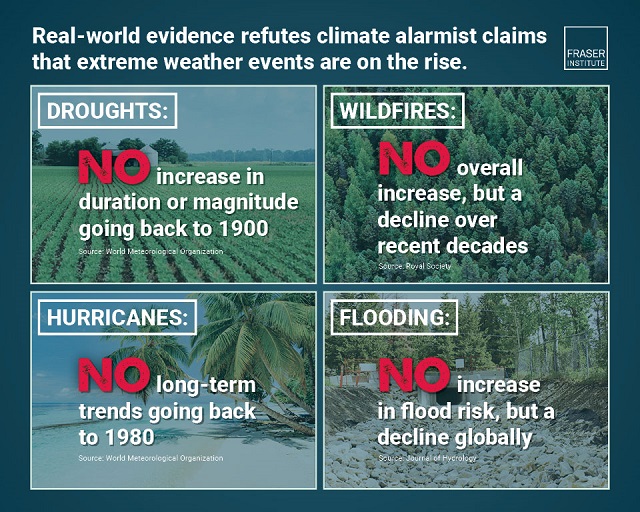
Great Reset9 hours agoClimate expert warns against extreme ‘weather porn’ from alarmists pushing ‘draconian’ policies
-

 Alberta2 days ago
Alberta2 days agoDanielle Smith warns arsonists who start wildfires in Alberta that they will be held accountable
-

 National2 days ago
National2 days agoCanada’s Governor General slammed for hosting partisan event promoting Trudeau’s ‘hate speech’ bill
-
 Economy2 days ago
Economy2 days agoExtreme Weather and Climate Change
-

 Bruce Dowbiggin1 day ago
Bruce Dowbiggin1 day agoWhy Are Canadian Mayors So Far Left And Out Of Touch?


