Fraser Institute
Yes, B.C.’s Land Act changes give First Nations veto over use of Crown Land

From the Fraser Institute
By Bruce Pardy
Nathan Cullen says there’s no veto. Cullen, British Columbia’s Minister of Water, Land, and Resource Stewardship, plans to give First Nations joint decision-making authority over Crown land. His NDP government recently opened consultations on its proposal to amend the B.C. Land Act, under which the minister grants leases, licences, permits, rights-of-way and land sales. The amendments will give legal effect to agreements with Indigenous governing bodies. Those agreements will share decision-making power “through joint or consent models” with some or all of B.C.’s more than 200 First Nations.
Yes, First Nations will have a veto.
Cullen denies it. “There is no veto in these amendments,” he told the Nanaimo News Bulletin last week. He accused critics of fearmongering and misinformation. “My worry is that for some of the political actors here on the right, this is an element of dog-whistle politics.”
But Cullen has a problem. Any activity that requires your consent is an activity over which you have a veto. If a contract requires approval of both parties before something can happen, “no” by one means “no” for both. The same is true in other areas of law such as sexual conduct, which requires consent. If you withhold your consent, you have vetoed the activity. “Joint decision-making,” “consent,” and “veto” come out to the same thing.
Land use decisions are subject to the same logic. The B.C. government will give First Nations joint decision-making power, when and where agreements are entered into. Its own consultation materials say so. This issue has blown up in the media, and the government has hastily amended its consultation webpage to soothe discontent (“The proposed amendments to the Land Act will not lead to broad, sweeping, or automatic changes (or) provide a ‘veto.’”) Nothing to see here folks. But its documentation continues to describe “shared decision-making through joint or consent models.”
These proposals should not surprise anyone. In 2019, the B.C. legislature passed Bill 41, the Declaration of the Rights of Indigenous Peoples Act (DRIPA). It requires the government to take “all measures necessary” to make the laws of British Columbia consistent with the United Nations Declaration on the Rights of Indigenous People (UNDRIP).
UNDRIP is a declaration of the U.N. General Assembly passed in 2007. It says that Indigenous people have “the right to the lands, territories and resources which they have traditionally owned, occupied or otherwise used or acquired… to own, use, develop and control.”
On its own, UNDRIP is non-binding and unenforceable. But DRIPA seeks to incorporate UNDRIP into B.C. law, obligating the government to achieve its aspirations. Mere consultation with First Nations, which Section 35 of the Constitution requires, won’t cut it under UNDRIP. Under Section 7 of DRIPA, agreements to be made with indigenous groups are to establish joint decision-making or to require consent of the Indigenous group. Either Cullen creates a First Nations veto or falls short of the goalposts in DRIPA. He is talking out of both sides of his mouth.
Some commentators warned against these dangers long ago. For example, shortly after DRIPA was passed in 2019, Vancouver lawyer Robin Junger wrote in the Vancouver Sun, “It will likely be impossible for government to live up to the expectations that Indigenous groups will now reasonably hold, without fundamentally affecting the rights and interests of third parties.” Unfortunately, few wanted to tackle that thorny question head on at the time. All three political parties in B.C. voted in favour of DRIPA, which passed unanimously.
For a taste of how Land Act changes could work, ask some B.C. residents who have private docks. In Pender Harbour, for instance, the shishalh Nation and the province have jointly developed a “Dock Management Plan” to try and impose various new and onerous rules on private property owners (including red “no go” zones and rules that will make many existing docks and boat houses non-compliant). Property owners with long-standing docks in full legal compliance will have no right to negotiate, to be consulted, or to be grandfathered. Land Act amendments may hardwire this plan into B.C. law.
Yet Cullen insists that no veto will exist since aggrieved parties can apply to a court for judicial review. “[An agreement] holds both parties—B.C. and whichever nation we enter into an agreement (with)—to the same standard of judicial review, administrative fairness, all the things that courts protect when someone is going through an application or a tendering process,” he told Business in Vancouver.
This is nonsense on stilts. By that standard, no government official has final authority under any statute. All statutory decisions are potentially subject to judicial review, including decisions of Cullen himself as the minister responsible for the Land Act. He doesn’t have a veto? Of course he does. Moreover, courts on judicial review generally defer to statutory decision-makers. And they don’t change decisions but merely send them back to be made again. The argument that First Nations won’t have a veto because their decisions can be challenged on judicial review is legal jibber jabber.
When the U.N. passed UNDRIP in 2007, people said they can’t be serious. When the B.C. legislature passed DRIPA in 2019, people said they can’t be serious. The B.C. government now proposes to give First Nations a veto over the use of Crown land. Don’t worry, they can’t be serious.
Author:
Fraser Institute
Long waits for health care hit Canadians in their pocketbooks

From the Fraser Institute
Canadians continue to endure long wait times for health care. And while waiting for care can obviously be detrimental to your health and wellbeing, it can also hurt your pocketbook.
In 2024, the latest year of available data, the median wait—from referral by a family doctor to treatment by a specialist—was 30 weeks (including 15 weeks waiting for treatment after seeing a specialist). And last year, an estimated 1.5 million Canadians were waiting for care.
It’s no wonder Canadians are frustrated with the current state of health care.
Again, long waits for care adversely impact patients in many different ways including physical pain, psychological distress and worsened treatment outcomes as lengthy waits can make the treatment of some problems more difficult. There’s also a less-talked about consequence—the impact of health-care waits on the ability of patients to participate in day-to-day life, work and earn a living.
According to a recent study published by the Fraser Institute, wait times for non-emergency surgery cost Canadian patients $5.2 billion in lost wages in 2024. That’s about $3,300 for each of the 1.5 million patients waiting for care. Crucially, this estimate only considers time at work. After also accounting for free time outside of work, the cost increases to $15.9 billion or more than $10,200 per person.
Of course, some advocates of the health-care status quo argue that long waits for care remain a necessary trade-off to ensure all Canadians receive universal health-care coverage. But the experience of many high-income countries with universal health care shows the opposite.
Despite Canada ranking among the highest spenders (4th of 31 countries) on health care (as a percentage of its economy) among other developed countries with universal health care, we consistently rank among the bottom for the number of doctors, hospital beds, MRIs and CT scanners. Canada also has one of the worst records on access to timely health care.
So what do these other countries do differently than Canada? In short, they embrace the private sector as a partner in providing universal care.
Australia, for instance, spends less on health care (again, as a percentage of its economy) than Canada, yet the percentage of patients in Australia (33.1 per cent) who report waiting more than two months for non-emergency surgery was much higher in Canada (58.3 per cent). Unlike in Canada, Australian patients can choose to receive non-emergency surgery in either a private or public hospital. In 2021/22, 58.6 per cent of non-emergency surgeries in Australia were performed in private hospitals.
But we don’t need to look abroad for evidence that the private sector can help reduce wait times by delivering publicly-funded care. From 2010 to 2014, the Saskatchewan government, among other policies, contracted out publicly-funded surgeries to private clinics and lowered the province’s median wait time from one of the longest in the country (26.5 weeks in 2010) to one of the shortest (14.2 weeks in 2014). The initiative also reduced the average cost of procedures by 26 per cent.
Canadians are waiting longer than ever for health care, and the economic costs of these waits have never been higher. Until policymakers have the courage to enact genuine reform, based in part on more successful universal health-care systems, this status quo will continue to cost Canadian patients.
Business
84% of Swiss hospitals and 60% of hospitalizations are in private facilities, and they face much lower wait times
From the Fraser Institute
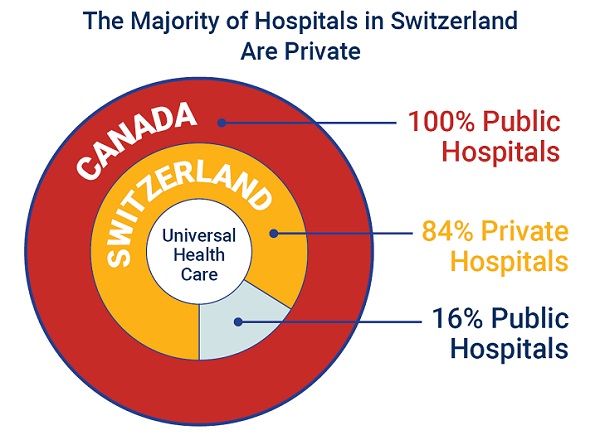
If Canada reformed to emulate Switzerland’s approach to universal health care, including its much greater use of private sector involvement, the country would deliver far better results to patients and reduce wait times, finds a new study published today by the Fraser Institute, an independent, non-partisan Canadian policy think-tank.
“The bane of Canadian health care is lack of access to timely care, so it’s critical to look to countries like Switzerland with more successful universal health care,” said Yanick Labrie, senior fellow at the Fraser Institute and author of Integrating Private Health Care Into Canada’s Public System: What We Can Learn from Switzerland. The study highlights how Switzerland successfully integrates the private sector into their universal health-care system, which consistently outperforms Canada on most health-care metrics, including wait times.
For example, in 2022, the percentage of patients who waited less than two months for a specialist appointment was 85.3 per cent in Switzerland compared to just 48.3 per cent in Canada.
In Switzerland, 84.2 per cent of all hospitals are private (either for-profit or not-for profit) institutions, and the country’s private hospitals provide 60.2 per cent of all hospitalizations, 60.9 per cent of all births, and 67.1 per cent of all operating rooms.
Crucially, Swiss patients can obtain treatment at the hospital of their choice, whether located inside or outside their geographic location, and hospitals cannot discriminate against patients, based on the care required.
“Switzerland shows that a universal health-care system can reconcile efficiency and equity–all while being more accessible and responsive to patients’ needs and preferences,” Labrie said.
“Based on the success of the Swiss model, provinces can make these reforms now and help improve Canadian health care.”

Integrating Private Health Care into Canada’s Public System: What We Can Learn from Switzerland
- Access to timely care remains the Achilles’ heel of Canada’s health systems. To reduce wait times, some provinces have partnered with private clinics for publicly funded surgeries—a strategy that has proven effective, but continues to spark debate in Canada.
- This study explores how Switzerland successfully integrates private health care into a universal public system and considers what Canada can learn from this model.
- In Switzerland, universal coverage is delivered through a system of managed competition among 44 non-profit private insurers, while decentralized governance allows each of the 26 cantons to coordinate and oversee hospital services in ways that reflect local needs and priorities.
- Nearly two-thirds of Swiss hospitals are for-profit institutions; they provide roughly half of all hospitalizations, births, and hospital beds across the country.
- All hospitals are treated equally—regardless of legal status—and funded through the same activity-based model, implemented nationwide in 2012.
- The reform led to a significant increase in the number of cases treated without a corresponding rise in expenditures per case, suggesting improved efficiency, better use of resources, and expanded access to hospital care.
- The average length of hospital stay steadily decreased over time and now stands at 4.87 days in for-profit hospitals versus 5.53 days in public ones, indicating faster patient turnover and more streamlined care pathways.
- Hospital-acquired infection rates are significantly lower in private hospitals (2.7%) than in public hospitals (6.2%), a key indicator of care quality.
- Case-mix severity is as high or higher in private hospitals, countering the notion that they only take on simpler or less risky cases.
- Patient satisfaction is slightly higher in private hospitals (4.28/5) than in public ones (4.17/5), reflecting strong user experience across multiple dimensions.
- Canada could benefit from regulated competition between public and private providers and activity-based funding, without breaching the Canada Health Act.