Health
Last day and last chance to win this dream home! Support the 2025 Red Deer Hospital Lottery before midnight!

Deadline: June 16, 2025
Draw: June 26, 2025
|
|
|
The 2025 Red Deer Hospital Lottery Dream Home, designed by Sorento Custom Homes, continues Sorento’s tradition of award-winning designs. This gorgeous bungalow features 2,824 sq ft of developed living space and showcases a tall, vaulted ceiling.
Located at 128 Emmett Crescent in the neighbourhood of Evergreen, this outstanding home features a screened deck off the dining room, a large family room on the lower level, and of course, a beautiful primary suite. Sorento’s ensuites are always something to behold, and this one features a claw foot tub. There’s an office on the main level, two bedrooms below, and a large fitness room that includes a two-person infrared sauna. Enjoy the convenience of a walk-in pantry, main floor laundry, and chef quality appliances. The design of this unique home is complemented by gorgeous furnishings by Urban Barn.
Our Grand Prize Dream Home package is valued at $1,074,472! You won’t want to miss seeing this outstanding home or your chance to live in it.
Aristotle Foundation
The Canadian Medical Association’s inexplicable stance on pediatric gender medicine

By Dr. J. Edward Les
The thalidomide saga is particularly instructive: Canada was the last developed country to pull thalidomide from its shelves — three months during which babies continued to be born in this country with absent or deformed limbs
Physicians have a duty to put forward the best possible evidence, not ideology, based treatments
Late last month, the Canadian Medical Association (CMA) announced that it, along with three Alberta doctors, had filed a constitutional challenge to Alberta’s Bill 26 “to protect the relationship between patients, their families and doctors when it comes to making treatment decisions.”
Bill 26, which became law last December, prohibits doctors in the province from prescribing puberty blockers and hormone therapies for those under 16; it also bans doctors from performing gender-reassignment surgeries on minors (those under 18).
The unprecedented CMA action follows its strongly worded response in February 2024 to Alberta’s (at the time) proposed legislation:
“The CMA is deeply concerned about any government proposal that restricts access to evidence-based medical care, including the Alberta government’s proposed restrictions on gender-affirming treatments for pediatric transgender patients.”
But here’s the problem with that statement, and with the CMA’s position: the evidence supporting the “gender affirmation” model of care — which propels minors onto puberty blockers, cross-gender hormones, and in some cases, surgery — is essentially non-existent. That’s why the United Kingdom’s Conservative government, in the aftermath of the exhaustive four-year-long Cass Review, which laid bare the lack of evidence for that model, and which shone a light on the deeply troubling potential for the model’s irreversible harm to youth, initiated a temporary ban on puberty blockers — a ban made permanent last December by the subsequent Labour government. And that’s why other European jurisdictions like Finland and Sweden, after reviews of gender affirming care practices in their countries, have similarly slammed the brakes on the administration of puberty blockers and cross-gender hormones to minors.
It’s not only the Europeans who have raised concerns. The alarm bells are ringing loudly within our own borders: earlier this year, a group at McMaster University, headed by none other than Dr. Gordon Guyatt, one of the founding gurus of the “evidence-based care” construct that rightfully underpins modern medical practice, issued a pair of exhaustive systematic reviews and meta analyses that cast grave doubts on the wisdom of prescribing these drugs to youth.
And yet, the CMA purports to be “deeply concerned about any government proposal that restricts access to evidence-based medical care,” which begs the obvious question: Where, exactly, is the evidence for the benefits of the “gender affirming” model of care? The answer is that it’s scant at best. Worse, the evidence that does exist, points, on balance, to infliction of harm, rather than provision of benefit.
CMA President Joss Reimer, in the group’s announcement of the organization’s legal action, said:
“Medicine is a calling. Doctors pursue it because they are compelled to care for and promote the well-being of patients. When a government bans specific treatments, it interferes with a doctor’s ability to empower patients to choose the best care possible.”
Indeed, we physicians have a sacred duty to pursue the well-being of our patients. But that means that we should be putting forward the best possible treatments based on actual evidence.
When Dr. Reimer states that a government that bans specific treatments is interfering with medical care, she displays a woeful ignorance of medical history. Because doctors don’t always get things right: look to the sad narratives of frontal lobotomies, the oxycontin crisis, thalidomide, to name a few.
The thalidomide saga is particularly instructive: it illustrates what happens when a government drags its heels on necessary action. Canada was the last developed country to pull thalidomide, given to pregnant women for morning sickness, from its shelves, three months after it had been banned everywhere else — three months during which babies continued to be born in this country with absent or deformed limbs, along with other severe anomalies. It’s a shameful chapter in our medical past, but it pales in comparison to the astonishing intransigence our medical leaders have displayed — and continue to display — on the youth gender care file.
A final note (prompted by thalidomide’s history), to speak to a significant quibble I have with Alberta’s Bill 26 legislation: as much as I admire Premier Danielle Smith’s courage in bringing it forward, the law contains a loophole allowing minors already on puberty blockers and cross-gender hormones to continue to take them. Imagine if, after it was removed from the shelves in 1962, government had allowed pregnant women already on the drug to continue to take thalidomide. Would that have made any sense? Of course not. And the same applies to puberty blockers and cross-gender hormones: they should be banned outright for all youth.
That argument is the kind our medical associations should be making — and would be making, if they weren’t so firmly in the grasp, seemingly, of ideologues who have abandoned evidence-based medical care for our youth.
J. Edward Les is a Calgary pediatrician, a senior fellow with the Aristotle Foundation for Public Policy, and co-author of “Teenagers, Children, and Gender Transition Policy: A Comparison of Transgender Medical Policy for Minors in Canada, the United States, and Europe.”
Fraser Institute
Long waits for health care hit Canadians in their pocketbooks

From the Fraser Institute
Canadians continue to endure long wait times for health care. And while waiting for care can obviously be detrimental to your health and wellbeing, it can also hurt your pocketbook.
In 2024, the latest year of available data, the median wait—from referral by a family doctor to treatment by a specialist—was 30 weeks (including 15 weeks waiting for treatment after seeing a specialist). And last year, an estimated 1.5 million Canadians were waiting for care.
It’s no wonder Canadians are frustrated with the current state of health care.
Again, long waits for care adversely impact patients in many different ways including physical pain, psychological distress and worsened treatment outcomes as lengthy waits can make the treatment of some problems more difficult. There’s also a less-talked about consequence—the impact of health-care waits on the ability of patients to participate in day-to-day life, work and earn a living.
According to a recent study published by the Fraser Institute, wait times for non-emergency surgery cost Canadian patients $5.2 billion in lost wages in 2024. That’s about $3,300 for each of the 1.5 million patients waiting for care. Crucially, this estimate only considers time at work. After also accounting for free time outside of work, the cost increases to $15.9 billion or more than $10,200 per person.
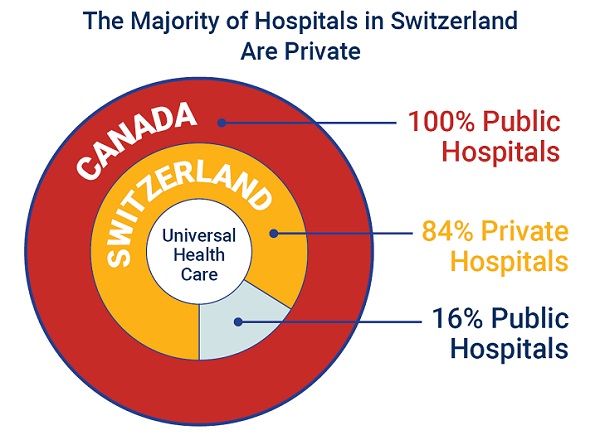
Of course, some advocates of the health-care status quo argue that long waits for care remain a necessary trade-off to ensure all Canadians receive universal health-care coverage. But the experience of many high-income countries with universal health care shows the opposite.
Despite Canada ranking among the highest spenders (4th of 31 countries) on health care (as a percentage of its economy) among other developed countries with universal health care, we consistently rank among the bottom for the number of doctors, hospital beds, MRIs and CT scanners. Canada also has one of the worst records on access to timely health care.
So what do these other countries do differently than Canada? In short, they embrace the private sector as a partner in providing universal care.
Australia, for instance, spends less on health care (again, as a percentage of its economy) than Canada, yet the percentage of patients in Australia (33.1 per cent) who report waiting more than two months for non-emergency surgery was much higher in Canada (58.3 per cent). Unlike in Canada, Australian patients can choose to receive non-emergency surgery in either a private or public hospital. In 2021/22, 58.6 per cent of non-emergency surgeries in Australia were performed in private hospitals.
But we don’t need to look abroad for evidence that the private sector can help reduce wait times by delivering publicly-funded care. From 2010 to 2014, the Saskatchewan government, among other policies, contracted out publicly-funded surgeries to private clinics and lowered the province’s median wait time from one of the longest in the country (26.5 weeks in 2010) to one of the shortest (14.2 weeks in 2014). The initiative also reduced the average cost of procedures by 26 per cent.
Canadians are waiting longer than ever for health care, and the economic costs of these waits have never been higher. Until policymakers have the courage to enact genuine reform, based in part on more successful universal health-care systems, this status quo will continue to cost Canadian patients.
-

 Alberta2 days ago
Alberta2 days agoAlberta’s grand bargain with Canada includes a new pipeline to Prince Rupert
-

 Bruce Dowbiggin1 day ago
Bruce Dowbiggin1 day agoWOKE NBA Stars Seems Natural For CDN Advertisers. Why Won’t They Bite?
-

 Business2 days ago
Business2 days agoCarney’s European pivot could quietly reshape Canada’s sovereignty
-

 Crime10 hours ago
Crime10 hours agoUK finally admits clear evidence linking Pakistanis and child grooming gangs
-

 Business14 hours ago
Business14 hours agoCarney praises Trump’s world ‘leadership’ at G7 meeting in Canada
-

 Energy1 day ago
Energy1 day agoCould the G7 Summit in Alberta be a historic moment for Canadian energy?
-

 conflict18 hours ago
conflict18 hours agoIsrael bombs Iranian state TV while live on air
-

 Crime1 day ago
Crime1 day agoMinnesota shooter arrested after 48-hour manhunt