Health
WHO’s Global Digital Health Certification Network

With notes from the World Health Organization website, Dr. John Campbell explains the WHO’s Global Digital Health Certification Network. To see the WHO’s press release click here or scroll below the video where it is attached.
From the youtube channel of  Dr. John Campbell
Dr. John Campbell
Press release from the World Health Organization
The European Commission and WHO launch landmark digital health initiative to strengthen global health security
The World Health Organization (WHO) and European Commission have announced today the launch of a landmark digital health partnership.
In June 2023, WHO will take up the European Union (EU) system of digital COVID-19 certification to establish a global system that will help facilitate global mobility and protect citizens across the world from on-going and future health threats, including pandemics. This is the first building block of the WHO Global Digital Health Certification Network (GDHCN) that will develop a wide range of digital products to deliver better health for all.
“Building on the EU’s highly successful digital certification network, WHO aims to offer all WHO Member States access to an open-source digital health tool, which is based on the principles of equity, innovation, transparency and data protection and privacy,” said Dr Tedros Adhanom Ghebreyesus, WHO Director-General. “New digital health products in development aim to help people everywhere receive quality health services quickly and more effectively”.
Based on the EU Global Health Strategy and WHO Global strategy on digital health, the initiative follows the 30 November 2022 agreement between Commissioner Kyriakides and Dr Tedros to enhance strategic cooperation on global health issues. This further bolsters a robust multilateral system with WHO at its core, powered by a strong EU.
“This partnership is an important step for the digital action plan of the EU Global Health Strategy. By using European best practices we contribute to digital health standards and interoperability globally—to the benefit of those most in need. It is also a powerful example of how alignment between the EU and the WHO can deliver better health for all, in the EU and across the world. As the directing and coordinating authority on international health work, there is no better partner than the WHO to advance the work we started at the EU and further develop global digital health solutions,” said Stella Kyriakides, Commissioner for Health and Food Safety.
This partnership will include close collaboration in the development, management and implementation of the WHO GDHCN system, benefitting from the European Commission’s ample technical expertise in the field. A first step is to ensure that the current EU digital certificates continue to function effectively.
“With 80 countries and territories connected to the EU Digital COVID-19 Certificate, the EU has set a global standard. The EU certificate has not only been an important tool in our fight against the pandemic, but has also facilitated international travel and tourism. I am pleased that the WHO will build on the privacy-preserving principles and cutting-edge technology of the EU certificate to create a global tool against future pandemics,” added Thierry Breton, Commissioner for Internal Market.
A global WHO system building on EU legacy
One of the key elements in the European Union’s work against the COVID-19 pandemic has been digital COVID-19 certificates. To facilitate free movement within its borders, the EU swiftly established interoperable COVID-19 certificates (entitled ‘EU Digital COVID-19 Certificate’ or ‘EU DCC’). Based on open-source technologies and standards it allowed also for the connection of non-EU countries that issue certificates according to EU DCC specifications, becoming the most widely used solution around the world.
From the onset of the pandemic, WHO engaged with all WHO Regions to define overall guidelines for such certificates. To help strengthen global health preparedness in the face of growing health threats, WHO is establishing a global digital health certification network which builds upon the solid foundations of the EU DCC framework, principles and open technologies. With this collaboration, WHO will facilitate this process globally under its own structure with the aim to allow the world to benefit from convergence of digital certificates. This includes standard-setting and validation of digital signatures to prevent fraud. In doing so, WHO will not have access to any underlying personal data, which would continue to be the exclusive domain of governments.
The first building block of the global WHO system becomes operational in June 2023 and aims to be progressively developed in the coming months.
A long-term digital partnership to deliver better health for all
To facilitate the uptake of the EU DCC by WHO and contribute to its operation and further development, WHO and the European Commission have agreed to partner in digital health.
This partnership will work to technically develop the WHO system with a staged approach to cover additional use cases, which may include, for example, the digitisation of the International Certificate of Vaccination or Prophylaxis. Expanding such digital solutions will be essential to deliver better health for citizens across the globe.
This cooperation is based on the shared values and principles of transparency and openness, inclusiveness, accountability, data protection and privacy, security, scalability at a global level, and equity. The WHO and the European Commission will work together to encourage maximum global uptake and participation. Particular attention will be paid to equitable opportunities for the participation by those most in need: low and middle-income countries.
Dr. John Campbell’s Presentation notes:
WHO’s Global Digital Health Certification Network https://www.who.int/initiatives/globa…
WHO has established the Global Digital Health Certification Network (GDHCN). Open-source platform, built on robust & transparent standards, that establishes the first building block of digital public health infrastructure, for developing a wide range of digital products, for strengthening pandemic preparedness
Background Member States used digital COVID-19 test and vaccine certificates As the directing and coordinating authority on international health work, at the onset of the pandemic, WHO engaged with all WHO Regions to define overall guidance for such certificates and published the Digital Documentation of COVID-19 Certificates
https://www.who.int/publications/i/it… https://www.who.int/publications/i/it… there is a recognition of an existing gap, and continued need for a global mechanism, that can support bilateral verification of the provenance of health documents
The GDHCN may include Digitisation of the International Certificate of Vaccination or Prophylaxis, verification of prescriptions across borders
International Patient Summary Verification of vaccination certificates within and across borders Certification of public health professionals (through WHO Academy) Expanding such digital solutions will be essential to deliver better health for people across the globe.
The GDHCN has been designed to be interoperable with other existing regional networks EU-WHO digital partnership https://www.who.int/news/item/05-06-2… ![]() • LIVE: WHO and @EU… https://commission.europa.eu/strategy… WHO and the European Commission have agreed to partner in digital health.
• LIVE: WHO and @EU… https://commission.europa.eu/strategy… WHO and the European Commission have agreed to partner in digital health.
This partnership will work to technically develop the WHO system with a staged approach to cover additional use cases, In June 2023, WHO will take up the European Union (EU) system of digital COVID-19 certification to establish a global system, that will help facilitate global mobility
This is the first building block of the WHO Global Digital Health Certification Network (GDHCN)
Dr Tedros Adhanom Ghebreyesus WHO aims to offer all WHO Member States access, On the principles of equity, innovation, transparency and data protection and privacy Stella Kyriakides, Commissioner for Health and Food Safety
This partnership is an important step for the digital action plan of the EU Global Health Strategy, we contribute to digital health standards and interoperability globally
Thierry Breton, Commissioner for Internal Market The EU certificate … has also facilitated international travel and tourism I am pleased that the WHO will build on …. cutting-edge technology … to create a global tool against future pandemics
One of the key elements in the European Union’s work against the COVID-19 pandemic has been digital COVID-19 certificates. WHO will facilitate this process globally under its own structure … allow the world to benefit from convergence of digital certificates. Expanding such digital solutions will be essential to deliver better health for citizens across the globe.
The WHO and the European Commission will work together to encourage maximum global uptake and participation.
Addictions
‘Over and over until they die’: Drug crisis pushes first responders to the brink

First responders say it is not overdoses that leave them feeling burned out—it is the endless cycle of calls they cannot meaningfully resolve
The soap bottle just missed his head.
Standing in the doorway of a cluttered Halifax apartment, Derek, a primary care paramedic, watched it smash against the wall.
Derek was there because the woman who threw it had called 911 again — she did so nearly every day. She said she had chest pain. But when she saw the green patch on his uniform, she erupted. Green meant he could not give her what she wanted: fentanyl.
She screamed at him to call “the red tags” — advanced care paramedics authorized to administer opioids. With none available, Derek declared the scene unsafe and left. Later that night, she called again. This time, a red-patched unit was available. She got her dose.
Derek says he was not angry at the woman, but at the system that left her trapped in addiction — and him powerless to help.
First responders across Canada say it is not overdoses that leave them feeling burned out — it is the endless cycle of calls they cannot meaningfully resolve. Understaffed, overburdened and dispatched into crises they are not equipped to fix, many feel morally and emotionally drained.
“We’re sending our first responders to try and manage what should otherwise be dealt with at structural and systemic levels,” said Nicholas Carleton, a University of Regina researcher who studies the mental health of public safety personnel.
Canadian Affairs agreed to use pseudonyms for the two frontline workers referenced in this story. Canadian Affairs also spoke with nine other first responders who agreed to speak only on background. All of these sources cited concerns about workplace retaliation for speaking out.
Moral injury
Canada’s opioid crisis is pushing frontline workers such as paramedics to the brink.
A 2024 study of 350 Quebec paramedics shows one in three have seriously considered suicide. Globally, ambulance workers have among the highest suicide rates of public service personnel.
Between 2017 and 2024, Canadian paramedics responded to nearly 240,000 suspected opioid overdoses. More than 50,000 of those were fatal.
Yet many paramedics say overdose calls are not the hardest part of the job.
“When they do come up, they’re pretty easy calls,” said Derek. Naloxone, a drug that reverses overdoses, is readily available. “I can actually fix the problem,” he said. “[It’s a] bit of instant gratification, honestly.”
What drains him are the calls they cannot fix: mental health crises, child neglect and abuse, homelessness.
“The ER has a [cardiac catheterization] lab that can do surgery in minutes to fix a heart attack. But there’s nowhere I can bring the mental health patients.
“So they call. And they call. And they call.”
Thomas, a primary care paramedic in Eastern Ontario, echoes that frustration.
“The ER isn’t a good place to treat addiction,” he said. “They need intensive, long-term psychological inpatient treatment and a healthy environment and support system — first responders cannot offer that.”
That powerlessness erodes trust. Paramedics say patients with addictions often become aggressive, or stop seeking help altogether.
“We have a terrible relationship with the people in our community struggling with addiction,” Thomas said. “They know they will sit in an ER bed for a few hours while being in withdrawals and then be discharged with a waitlist or no follow-up.”
Carleton, of the University of Regina, says that reviving people repeatedly without improvement decreases morale.
“You’re resuscitating someone time and time again,” said Carleton, who is also director of the Psychological Trauma and Stress Systems Lab, a federal unit dedicated to mental health research for public safety personnel. “That can lead to compassion fatigue … and moral injury.”
Katy Kamkar, a clinical psychologist focused on first responder mental health, says moral injury arises when workers are trapped in ethically impossible situations — saving a life while knowing that person will be back in the same state tomorrow.
“Burnout is … emotional exhaustion, depersonalization, and reduced personal accomplishment,” she said in an emailed statement. “High call volumes, lack of support or follow-up care for patients, and/or bureaucratic constraints … can increase the risk of reduced empathy, absenteeism and increased turnover.”
Kamkar says moral injury affects all branches of public safety, not just paramedics. Firefighters, who are often the first to arrive on the scene, face trauma from overdose deaths. Police report distress enforcing laws that criminalize suffering.
Understaffed and overburdened
Staffing shortages are another major stressor.
“First responders were amazing during the pandemic, but it also caused a lot of fatigue, and a lot of people left our business because of stress and violence,” said Marc-André Périard, vice president of the Paramedic Chiefs of Canada.
Nearly half of emergency medical services workers experience daily “Code Blacks,” where there are no ambulances available. Vacancy rates are climbing across emergency services. The federal government predicts paramedic shortages will persist over the coming decade, alongside moderate shortages of police and firefighters.
Unsafe work conditions are another concern. Responders enter chaotic scenes where bystanders — often fellow drug users — mistake them for police. Paramedics can face hostility from patients they just saved, says Périard.
“People are upset that they’ve been taken out of their high [when Naloxone is administered] and not realizing how close to dying they were,” he said.
Thomas says safety is undermined by vague, inconsistently enforced policies. And efforts to collect meaningful data can be hampered by a work culture that punishes reporting workplace dangers.
“If you report violence, it can come back to haunt you in performance reviews” he said.
Some hesitate to wait for police before entering volatile scenes, fearing delayed response times.
“[What] would help mitigate violence is to have management support their staff directly in … waiting for police before arriving at the scene, support paramedics in leaving an unsafe scene … and for police and the Crown to pursue cases of violence against health-care workers,” Thomas said.
“Right now, the onus is on us … [but once you enter], leaving a scene is considered patient abandonment,” he said.
Upstream solutions
Carleton says paramedics’ ability to refer patients to addiction and mental health referral networks varies widely based on their location. These networks rely on inconsistent local staffing, creating a patchwork system where people easily fall through the cracks.
“[Any] referral system butts up really quickly against the challenges our health-care system is facing,” he said. “Those infrastructures simply don’t exist at the size and scale that we need.”
Périard agrees. “There’s a lot of investment in safe injection sites, but not as much [resources] put into help[ing] these people deal with their addictions,” he said.
Until that changes, the cycle will continue.
On May 8, Alberta renewed a $1.5 million grant to support first responders’ mental health. Carleton welcomes the funding, but says it risks being futile without also addressing understaffing, excessive workloads and unsafe conditions.
“I applaud Alberta’s investment. But there need to be guardrails and protections in place, because some programs should be quickly dismissed as ineffective — but they aren’t always,” he said.
Carleton’s research found that fewer than 10 mental health programs marketed to Canadian governments — out of 300 in total — are backed up by evidence showing their effectiveness.
In his view, the answer is not complicated — but enormous.
“We’ve got to get way further upstream,” he said.
“We’re rapidly approaching more and more crisis-level challenges… with fewer and fewer [first responders], and we’re asking them to do more and more.”
This article was produced through the Breaking Needles Fellowship Program, which provided a grant to Canadian Affairs, a digital media outlet, to fund journalism exploring addiction and crime in Canada. Articles produced through the Fellowship are co-published by Break The Needle and Canadian Affairs.
Business
Prime minister can make good on campaign promise by reforming Canada Health Act

From the Fraser Institute
While running for the job of leading the country, Prime Minister Carney promised to defend the Canada Health Act (CHA) and build a health-care system Canadians can be proud of. Unfortunately, to have any hope of accomplishing the latter promise, he must break the former and reform the CHA.
As long as Ottawa upholds and maintains the CHA in its current form, Canadians will not have a timely, accessible and high-quality universal health-care system they can be proud of.
Consider for a moment the remarkably poor state of health care in Canada today. According to international comparisons of universal health-care systems, Canadians endure some of the lowest access to physicians, medical technologies and hospital beds in the developed world, and wait in queues for health care that routinely rank among the longest in the developed world. This is all happening despite Canadians paying for one of the developed world’s most expensive universal-access health-care systems.
None of this is new. Canada’s poor ranking in the availability of services—despite high spending—reaches back at least two decades. And wait times for health care have nearly tripled since the early 1990s. Back then, in 1993, Canadians could expect to wait 9.3 weeks for medical treatment after GP referral compared to 30 weeks in 2024.
But fortunately, we can find the solutions to our health-care woes in other countries such as Germany, Switzerland, the Netherlands and Australia, which all provide more timely access to quality universal care. Every one of these countries requires patient cost-sharing for physician and hospital services, and allows private competition in the delivery of universally accessible services with money following patients to hospitals and surgical clinics. And all these countries allow private purchases of health care, as this reduces the burden on the publicly-funded system and creates a valuable pressure valve for it.
And this brings us back to the CHA, which contains the federal government’s requirements for provincial policymaking. To receive their full federal cash transfers for health care from Ottawa (totalling nearly $55 billion in 2025/26) provinces must abide by CHA rules and regulations.
And therein lies the rub—the CHA expressly disallows requiring patients to share the cost of treatment while the CHA’s often vaguely defined terms and conditions have been used by federal governments to discourage a larger role for the private sector in the delivery of health-care services.
Clearly, it’s time for Ottawa’s approach to reflect a more contemporary understanding of how to structure a truly world-class universal health-care system.
Prime Minister Carney can begin by learning from the federal government’s own welfare reforms in the 1990s, which reduced federal transfers and allowed provinces more flexibility with policymaking. The resulting period of provincial policy innovation reduced welfare dependency and government spending on social assistance (i.e. savings for taxpayers). When Ottawa stepped back and allowed the provinces to vary policy to their unique circumstances, Canadians got improved outcomes for fewer dollars.
We need that same approach for health care today, and it begins with the federal government reforming the CHA to expressly allow provinces the ability to explore alternate policy approaches, while maintaining the foundational principles of universality.
Next, the Carney government should either hold cash transfers for health care constant (in nominal terms), reduce them or eliminate them entirely with a concordant reduction in federal taxes. By reducing (or eliminating) the pool of cash tied to the strings of the CHA, provinces would have greater freedom to pursue reform policies they consider to be in the best interests of their residents without federal intervention.
After more than four decades of effectively mandating failing health policy, it’s high time to remove ambiguity and minimize uncertainty—and the potential for politically motivated interpretations—in the CHA. If Prime Minister Carney wants Canadians to finally have a world-class health-care system then can be proud of, he should allow the provinces to choose their own set of universal health-care policies. The first step is to fix, rather than defend, the 40-year-old legislation holding the provinces back.
-

 Alberta2 days ago
Alberta2 days agoCOWBOY UP! Pierre Poilievre Promises to Fight for Oil and Gas, a Stronger Military and the Interests of Western Canada
-

 MAiD1 day ago
MAiD1 day agoCanada’s euthanasia regime is already killing the disabled. It’s about to get worse
-

 Crime2 days ago
Crime2 days agoEyebrows Raise as Karoline Leavitt Answers Tough Questions About Epstein
-
 Alberta2 days ago
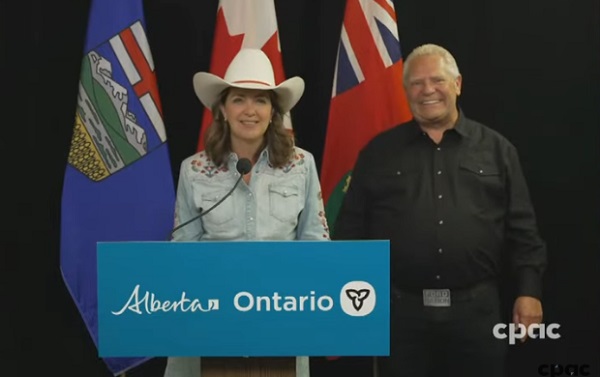
Alberta2 days agoAlberta and Ontario sign agreements to drive oil and gas pipelines, energy corridors, and repeal investment blocking federal policies
-

 Fraser Institute24 hours ago
Fraser Institute24 hours agoBefore Trudeau average annual immigration was 617,800. Under Trudeau number skyrocketted to 1.4 million from 2016 to 2024
-
 Daily Caller1 day ago
Daily Caller1 day ago‘I Know How These People Operate’: Fmr CIA Officer Calls BS On FBI’s New Epstein Intel
-
 Censorship Industrial Complex13 hours ago
Censorship Industrial Complex13 hours agoCanadian pro-freedom group sounds alarm over Liberal plans to revive internet censorship bill
-

 International2 days ago
International2 days agoChicago suburb purchases childhood home of Pope Leo XIV