COVID-19
We all want this crisis to end. Read this. Then find a mask and put it on when you go out in public

This is article is abridged for your convenience.
Public use of masks to control the coronavirus pandemic
(Originally published March 29 by Longrich Paleo Lab)
Nicholas R. Longrich, PhD
Department of Biology and Biochemistry, University of Bath, Bath, United Kingdom
The Longrich Paleontology Lab is part of the Milner Centre for Evolution at the University of Bath. We use fossils to understand large-scale evolutionary change in organisms and ecosystems.
The US and UK governments, as well as the World Health Organization, currently advise against the use of masks by the public to fight the ongoing Coronavirus Disease 19 (COVID-19) pandemic (1). But could they be wrong?
The governments of China, South Korea, Hong Kong, Viet Nam, Czechia, Slovakia, Bosnia and Taiwan all recommend that the public wear masks to slow the spread of the coronavirus. In some countries, like Japan, masks aren’t officially recommended, but are still widely used by the public. Many countries treat masks as a strategic resource. China has ramped up production of facemasks, converting Foxconn factories that once made iPhones to make face masks. Taiwan has also ramped up the production of facemasks, prohibited their export, and implemented price controls and rationing. It’s hard to see how both approaches could be right. Increasingly, advice against the use of face masks has been questioned (1) (2) (3), including by the head of China’s CDC (4). Austria has recently moved to make mask wearing in public obligatory, and in the United States, the CDC is now debating their use.
Common sense, scientific studies, but perhaps most of all the success of countries using masks to fight the coronavirus suggest that masks may make a difference. There are fewer scientific studies available to guide decision making than we might like, and the evidence is not always clear-cut. However, decision-making in a crisis requires that decisions be made in the absence of perfect clarity. What is clear is that the exponential mathematics of pandemics mean that even if masks are of limited benefit in reducing infection rates, masks could make a large difference over time, potentially slowing the pace of the pandemic, limiting its spread, saving lives, and finally, letting countries to restart the economies that their people depend on for their livelihoods.

Figure produced by Johns Hopkins University using data from Worldometers on March 29.
Masks protect you from others, others from you
It seems sensible to assume that any barrier between two people’s airways reduces the chance of an air-borne virus being transmitted between them. Masks worn by infected people catch some fraction of virus-laden respiratory droplets that are released by breathing and coughing. Perhaps just as important, breathing through a mask slows and deflects air as it is exhaled, potentially reducing the distance that viral droplets travel as aerosols.
Meanwhile, masks worn by uninfected people catch a fraction of the virus they’d otherwise inhale. If both infected and uninfected people wear masks, then these effects multiply. For example, hypothetically, if an infected person’s mask reduces the amount of virus spread by 75%, and the uninfected person’s mask reduces it by another 75%, then the total reduction of the virus spread is 94%.
It’s still possible that this reduction isn’t enough to prevent infection. However, masks could still protect people— because dosage matters. Lower dosing of virus means infection takes longer to build up, giving the immune system time to mount a response.
The immune system fights viruses, like a farmer trying to remove weeds from his field. How difficult those weeds will be to control depends on how many seeds there are. 1000 seeds in a field might not be a challenge, but 1,000,000 or 100 million make weeding far more difficult. In the same way, even when masks fail to prevent infection, by lowering the initial dose of virus they could conceivably make the difference between mild symptoms and a severe illness requiring hospitalization, or even leading to death.

Models suggest masks could work to control pandemics
Of course, it’s possible that masks might have only limited benefit in stopping the spread of COVID-19— for any number of reasons. Masks might provide limited protection, because they are less effective than suggested by some studies, because people misuse them, because of shortages of effective masks like surgical masks and N-95s— or all of these.
But to understand how they could still make a difference, we have to consider masks in the context of small reductions in viral transmission rates. Consider how epidemics grow— exponentially. Allowed to spread unchecked, one case of Covid-19 becomes 2.5 (assuming for this model an R0 of 2.5), each case causing 2.5 more, and so on. Over the course of 15 reproductive cycles, each taking 7 days, or about 3 months in total, one case becomes 2.5 x 2.5 x 25… or 2.5^15 = 931,323 cases (Fig. 1).
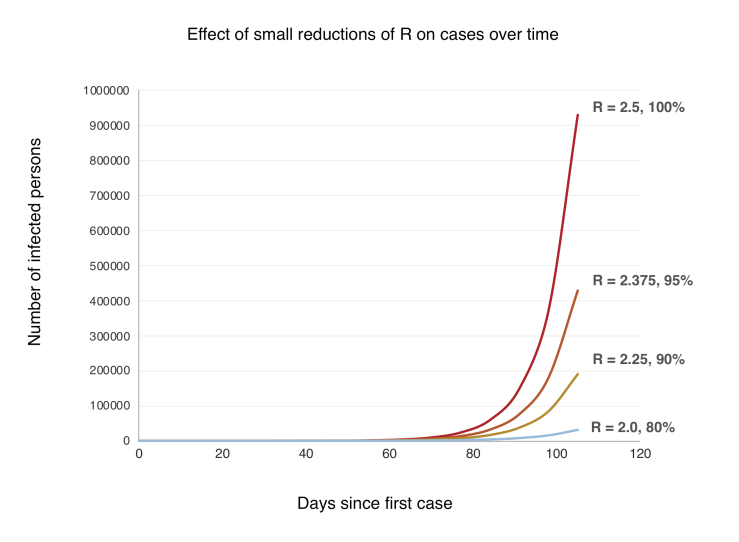
Figure 1. A simple model showing exponential growth in an uncontained outbreak over time (generation time = 7 days, R0 = 2.5) and with small reductions in the reproductive rate R.
Now, let’s suppose widespread use of masks cuts the growth rate by just 10%. Each person now infects 2.25 others, who infect 2.25 others, and so on. Over 15 cycles, 2.25^15 = 191,751 cases. An 80% reduction. Understanding this exponential growth explains how the virus caught the world by surprise even as the pandemic was monitored in real time. Exponential growth just doesn’t make sense, until you do the numbers, and even, they’re still hard to believe. But another counterintuitive aspect of exponential growth is that small decreases in the exponent greatly slow growth. A 10% increase in the exponent can have a massive effect, but even a limited intervention, with a 10% decrease over time, pays large dividends (Fig. 1).
These are very, very simple models. But sophisticated modeling also shows large scale use of masks could slow, even stop pandemics. A 2010 study found that above a certain threshold, widespread use of effective masks can reduce the reproductive number (R) of an influenza virus below 1, and the pandemic stops (25). If face masks were highly effective (well-designed, used properly and consistently), then public use of masks could stop a flu pandemic if used by just 50% of people. If masks were less effective, more than half the population would have to wear them to stop the pandemic. If masks were highly ineffective, they could flatten the curve of the epidemic, but wouldn’t stop it (25). We don’t know which model is most accurate. But does it even matter? In the context of the current pandemic, any of these scenarios would be a huge win.

Real world experience suggests masks work in pandemics
The most compelling evidence of the potential effectiveness of masks in the fight against COVID-19 comes from their use in the real world. Places that have controlled their coronavirus epidemics most effectively – China, South Korea, Hong Kong, Taiwan, Vietnam, Singapore, Kuwait, Czechia, Slovakia, Japan- use masks (Fig. 2). Aside from China, which was the epicenter of the pandemic and so played catchup in developing and implementing its strategy, virtually all of the worst outbreaks are in Western countries that officially advise against mask use, and where there is little culture or practice of mask wearing.
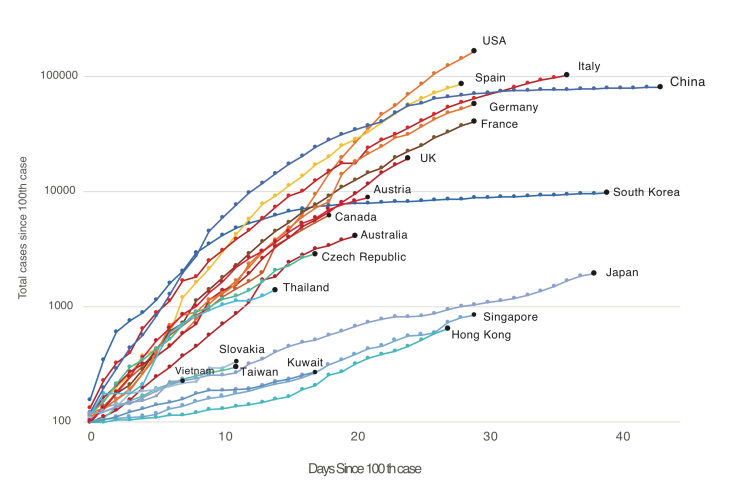
Figure 2. Western countries (US, Canada, Australia, UK, Western Europe) versus countries and territories using masks as part of official government or in practice policy (China, South Korea, Japan, Hong Kong, Taiwan, Vietnam, Thailand, Kuwait, Slovakia, Czech Republic, in blues and greens). Countries with official or unofficial policies of mask usage have controlled the outbreak far better than those without. Note that Austria currently uses masks but has only revised its official policy recently.
Places like China, South Korea, Taiwan, Vietnam, Kuwait, Czechia and Singapore differ greatly in political organization, ranging from communism to democracies, and also in their level of economic development and population density. And strikingly, these countries also differ in their suppression strategies. China implemented a lockdown of Wuhan, shut down industry nationwide, implemented temperature checks and social distancing, tested extensively— and employed masks. Korea responded with an aggressive testing and contact tracing—and masks. Japan has done far less extensive testing than Korea, but shut down schools and large gatherings— and used masks. The pandemic management strategies used by these countries far more diverse than has been appreciated. Arguably one of the few things all these successes share is widespread wearing of masks. And on the other hand, one common factor shared by the pandemic suppression strategies of the US, Canada, the UK and Europe is the decision to discourage the use of masks by the public. This evidence doesn’t prove, but it does very strongly hint that masks are a critical part of these country’s suppression strategies. And by watching countries like Austria that have recently revised their policies, we can test this idea.

What kind of mask? Surgical masks as good as N95s; are improvised masks better than nothing?
Would cloth masks work? Research into the effectiveness of cloth masks is limited (34). Existing research shows homemade masks are- unsurprisingly- inferior to surgical masks. However, they appear to be better than nothing. One laboratory study found homemade masks were half as effective as surgical masks in filtering particles (35). Another study found homemade masks made from various materials stopped virus aerosols, but less well than surgical masks (36). A surgical mask stopped 90% of viral aerosol particles, a dish towel, 72%, linen, 62%, and a cotton T-shirt, 51% (36).
Conclusions
Strong scientific evidence and rational arguments exist for the widespread, public use of facemasks. The principle behind facemasks- they reduce the amount of virus exhaled by infected people, and inhaled by uninfected- suggest they should be a primary tool in combating any respiratory virus. Scientific research, including experimental studies, retrospective studies of the SARS epidemic, hospital studies of COVID-19, and modeling studies, all suggests masks are likely to be effective in controlling the pandemic. Most importantly, the experience of countries using masks against SARS and the current coronavirus pandemic imply that they are effective when used by the public. However, modeling studies and the real-world experience of countries like China and South Korea suggests that neither masks, nor anything else, provides a magic bullet against a pandemic. So strategies should not rely on any single intervention, but rather a wide range of interventions, potentially including masks. Further research and open debate on the effectiveness of masks and other strategies are urgently needed.
Flames GM Brad Treliving does what he can to be ready for NHL reboot
Business
Conservatives demand probe into Liberal vaccine injury program’s $50m mismanagement

From LifeSiteNews
The Liberals’ Vaccine Injury Support Program is accused of mismanaging a $50-million contract with Oxaro Inc. and failing to resolve claims for thousands of vaccine-injured Canadians.
Conservatives are calling for an official investigation into the Liberal-run vaccine injury program, which has cost Canadians millions but has little to show for it.
On July 14th, four Conservative Members of Parliament (MPs) signed a letter demanding answers after an explosive Global News report found the Liberals’ Vaccine Injury Support Program (VISP) misallocated taxpayer funds and disregarded many vaccine-injured Canadians.
“The federal government awarded a $50 million taxpayer-funded contract to Oxaro Inc. (formerly Raymond Chabot Grant Thornton Consulting Inc.). The purpose of this contract was to administer the VISP,” the letter wrote.
“However, there was no clear indication that Oxaro had credible experience in healthcare or in the administration of health-related claims raising valid questions about how and why this firm was selected,” it continued.
Canada’s VISP was launched in December 2020 after the Canadian government gave vaccine makers a shield from liability regarding COVID-19 jab-related injuries.
However, mismanagement within the program has led to many injured Canadians still waiting to receive compensation, while government contractors grow richer.
“Despite the $50 million contract, over 1,700 of the 3,100 claims remain unresolved,” the Conservatives continued. “Families dealing with life-altering injuries have been left waiting years for answers and support they were promised.”
Furthermore, the claims do not represent the total number of Canadians injured by the allegedly “safe and effective” COVID shots, as inside memos have revealed that the Public Health Agency of Canada (PHAC) officials neglected to report all adverse effects from COVID shots and even went as far as telling staff not to report all events.
The PHAC’s downplaying of vaccine injuries is of little surprise to Canadians, as a 2023 secret memo revealed that the federal government purposefully hid adverse effect so as not to alarm Canadians.
Of the $50.6 million that Oxaro Inc., has received, $33.7 million has been spent on administrative costs, compared to only $16.9 million going to vaccine-injured Canadians.
The letter further revealed that former VISP employees have revealed that the program lacked professionalism, describing what Conservatives described as “a fraternity house rather than a professional organization responsible for administering health-related claims.”
“Reports of constant workplace drinking, ping pong, and Netflix are a slap in the face to taxpayers and the thousands of Canadians waiting for support for life altering injuries,” the letter continued.
Regardless of this, the Liberal government, under Prime Minister Mark Carney, is considering renewing its contract with Oxaro Inc.
Indeed, this would hardly be the first time that Liberals throw taxpayer dollars at a COVID program that is later exposed as ineffective and mismanaged.
Canada’s infamous ArriveCan app, which was mandated for all travelers in and out of Canada in 2020, has cost Canadians $54 million, despite the Public Health Agency of Canada admitting that they have no evidence that the program saved lives.
Details regarding the app and the government contracts surrounding it have been hidden from Canadians, as Liberals were exposed in 2023 for hiding a RCMP investigation into the app from auditors.
An investigation of the ArriveCan app began in 2022 after the House of Commons voted 173-149 for a full audit of the controversial app.
COVID-19
Trump DOJ dismisses charges against doctor who issued fake COVID passports

From LifeSiteNews
Attorney General Pam Bondi has ended the federal prosecution of Dr. Michael Kirk Moore for giving ‘patients a choice when the federal government refused to do so.’
The Utah plastic surgeon who issued fake COVID-19 vaccine passports to help patients get around COVID vaccine mandates will no longer be prosecuted, U.S. Attorney General Pam Bondi announced Saturday.
During the COVID pandemic, Dr. Michael Kirk Moore Jr. and employees at his Salt Lake private practice developed a plan to provide patients who objected to being forced to take the vaccine with ineffectual, harmless saline injections instead and give them COVID vaccination cards that would satisfy (since rescinded) mandates to take the shot as a condition of employment, public facilities, mass gatherings, and more.
For his efforts, he was indicted for allegedly “endanger[ing] the health and well-being of a vulnerable population” and “undermin[ing] public trust and the integrity of federal health care programs.” The government also accused him of doing so for profit, but several sources attested off the record that Moore not only issued the cards for free but actually refused offers of compensation.
“They broke no laws and harmed no person,” the defendants’ legal team said in 2023. “Dr. Moore, specifically, abided by his long held Hippocratic oath to First Do No Harm. We believe he and his co-defendants will be found innocent of all charges.”
Last month, LifeSiteNews reported that Moore’s trial was set to begin on July 7, which could have potentially ended with him facing 35 years in jail and a $125,000 penalty. Supporters of the doctor had expressed worry that the change in presidential administration had not yet halted the prosecution.
Over the weekend, however, Bondi announced that at her direction it has now done exactly that.
“Dr. Moore gave his patients a choice when the federal government refused to do so,” she said. “He did not deserve the years in prison he was facing. It ends today.”
There is a large body of warning signs against the shots, which were developed in record time by the first Trump administration’s Operation Warp Speed initiative.
The federal Vaccine Adverse Event Reporting System (VAERS) reports 38,709 deaths, 221,030 hospitalizations, 22,331 heart attacks, and 28,966 myocarditis and pericarditis cases as of June 27, among other ailments. U.S. Centers for Disease Control & Prevention (CDC) researchers have recognized a “high verification rate of reports of myocarditis to VAERS after mRNA-based COVID-19 vaccination,” leading to the conclusion that “under-reporting is more likely” than over-reporting.
An analysis of 99 million people across eight countries published in the journal Vaccine “observed significantly higher risks of myocarditis following the first, second and third doses” of mRNA-based COVID vaccines, as well as signs of increased risk of “pericarditis, Guillain-Barré syndrome, and cerebral venous sinus thrombosis,” and other “potential safety signals that require further investigation.”
In April 2024, the U.S. Centers for Disease Control & Prevention (CDC) was forced to release by court order 780,000 previously undisclosed reports of serious adverse reactions, and a study out of Japan found “statistically significant increases” in cancer deaths after third doses of mRNA-based COVID-19 vaccines, and offered several theories for a causal link.
In January, a long-awaited Florida grand jury report on the COVID vaccine manufacturers found that while only a miniscule percentage of the millions of vaccinations resulted in serious harm based on the data it had access to, such events do occur, and there are “profound and serious issues” in pharmaceutical companies’ review process, including reluctance to share what evidence of adverse events they did find.
In May, Trump administration U.S. Food & Drug Administration (FDA) Commissioner Dr. Marty Makary and vaccine chief Dr. Vinay Prasad announced that there would no longer be blanket recommendations for all Americans to receive the shot, but the “risk factors” it would still be recommended for include asthma, cancer, cerebrovascular disease, chronic kidney diseases, a handful of chronic liver and lung diseases, diabetes, disabilities such as Down’s syndrome, heart conditions, HIV, dementia, Parkinson’s, obesity, smoking, tuberculosis, and more. Health & Human Services (HHS) Secretary Robert F. Kennedy Jr. subsequently announced COVID vaccines will not be recommended to healthy children or pregnant women.
The Trump administration has approved a new mRNA-based COVID-19 vaccine from Moderna, suggesting the federal government’s overall view of the shots will remain favorable, albeit without mandates of any kind. At the same time, it does require mRNA COVID shots to carry a new warning about the danger of heart damage in young men.
-

 Business1 day ago
Business1 day agoMark Carney’s Fiscal Fantasy Will Bankrupt Canada
-

 Opinion1 day ago
Opinion1 day agoCharity Campaigns vs. Charity Donations
-

 Alberta1 day ago
Alberta1 day agoTemporary Alberta grid limit unlikely to dampen data centre investment, analyst says
-

 Frontier Centre for Public Policy2 days ago
Frontier Centre for Public Policy2 days agoCanada’s New Border Bill Spies On You, Not The Bad Guys
-

 Daily Caller20 hours ago
Daily Caller20 hours ago‘Strange Confluence Of Variables’: Mike Benz Wants Transparency Task Force To Investigate What Happened in Butler, PA
-

 Uncategorized2 days ago
Uncategorized2 days agoCNN’s Shock Climate Polling Data Reinforces Trump’s Energy Agenda
-
 Opinion1 day ago
Opinion1 day agoPreston Manning: Three Wise Men from the East, Again
-

 COVID-191 day ago
COVID-191 day agoTrump DOJ dismisses charges against doctor who issued fake COVID passports


