COVID-19
We all want this crisis to end. Read this. Then find a mask and put it on when you go out in public

This is article is abridged for your convenience.
Public use of masks to control the coronavirus pandemic
(Originally published March 29 by Longrich Paleo Lab)
Nicholas R. Longrich, PhD
Department of Biology and Biochemistry, University of Bath, Bath, United Kingdom
The Longrich Paleontology Lab is part of the Milner Centre for Evolution at the University of Bath. We use fossils to understand large-scale evolutionary change in organisms and ecosystems.
The US and UK governments, as well as the World Health Organization, currently advise against the use of masks by the public to fight the ongoing Coronavirus Disease 19 (COVID-19) pandemic (1). But could they be wrong?
The governments of China, South Korea, Hong Kong, Viet Nam, Czechia, Slovakia, Bosnia and Taiwan all recommend that the public wear masks to slow the spread of the coronavirus. In some countries, like Japan, masks aren’t officially recommended, but are still widely used by the public. Many countries treat masks as a strategic resource. China has ramped up production of facemasks, converting Foxconn factories that once made iPhones to make face masks. Taiwan has also ramped up the production of facemasks, prohibited their export, and implemented price controls and rationing. It’s hard to see how both approaches could be right. Increasingly, advice against the use of face masks has been questioned (1) (2) (3), including by the head of China’s CDC (4). Austria has recently moved to make mask wearing in public obligatory, and in the United States, the CDC is now debating their use.
Common sense, scientific studies, but perhaps most of all the success of countries using masks to fight the coronavirus suggest that masks may make a difference. There are fewer scientific studies available to guide decision making than we might like, and the evidence is not always clear-cut. However, decision-making in a crisis requires that decisions be made in the absence of perfect clarity. What is clear is that the exponential mathematics of pandemics mean that even if masks are of limited benefit in reducing infection rates, masks could make a large difference over time, potentially slowing the pace of the pandemic, limiting its spread, saving lives, and finally, letting countries to restart the economies that their people depend on for their livelihoods.

Figure produced by Johns Hopkins University using data from Worldometers on March 29.
Masks protect you from others, others from you
It seems sensible to assume that any barrier between two people’s airways reduces the chance of an air-borne virus being transmitted between them. Masks worn by infected people catch some fraction of virus-laden respiratory droplets that are released by breathing and coughing. Perhaps just as important, breathing through a mask slows and deflects air as it is exhaled, potentially reducing the distance that viral droplets travel as aerosols.
Meanwhile, masks worn by uninfected people catch a fraction of the virus they’d otherwise inhale. If both infected and uninfected people wear masks, then these effects multiply. For example, hypothetically, if an infected person’s mask reduces the amount of virus spread by 75%, and the uninfected person’s mask reduces it by another 75%, then the total reduction of the virus spread is 94%.
It’s still possible that this reduction isn’t enough to prevent infection. However, masks could still protect people— because dosage matters. Lower dosing of virus means infection takes longer to build up, giving the immune system time to mount a response.
The immune system fights viruses, like a farmer trying to remove weeds from his field. How difficult those weeds will be to control depends on how many seeds there are. 1000 seeds in a field might not be a challenge, but 1,000,000 or 100 million make weeding far more difficult. In the same way, even when masks fail to prevent infection, by lowering the initial dose of virus they could conceivably make the difference between mild symptoms and a severe illness requiring hospitalization, or even leading to death.

Models suggest masks could work to control pandemics
Of course, it’s possible that masks might have only limited benefit in stopping the spread of COVID-19— for any number of reasons. Masks might provide limited protection, because they are less effective than suggested by some studies, because people misuse them, because of shortages of effective masks like surgical masks and N-95s— or all of these.
But to understand how they could still make a difference, we have to consider masks in the context of small reductions in viral transmission rates. Consider how epidemics grow— exponentially. Allowed to spread unchecked, one case of Covid-19 becomes 2.5 (assuming for this model an R0 of 2.5), each case causing 2.5 more, and so on. Over the course of 15 reproductive cycles, each taking 7 days, or about 3 months in total, one case becomes 2.5 x 2.5 x 25… or 2.5^15 = 931,323 cases (Fig. 1).
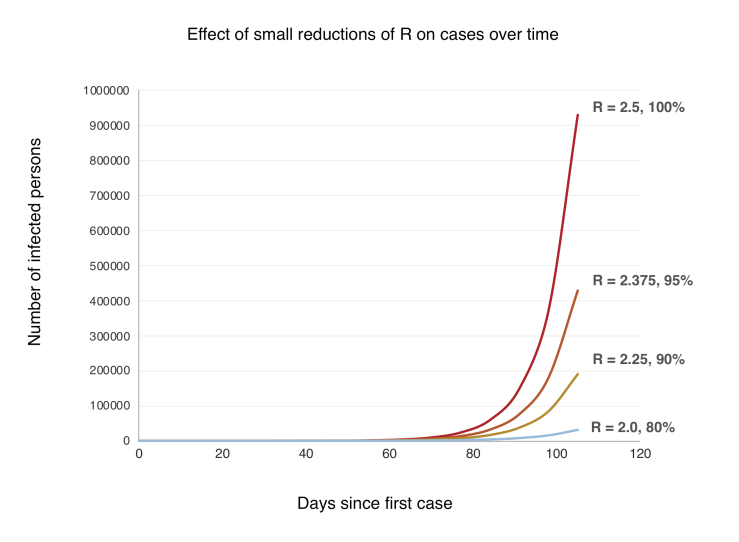
Figure 1. A simple model showing exponential growth in an uncontained outbreak over time (generation time = 7 days, R0 = 2.5) and with small reductions in the reproductive rate R.
Now, let’s suppose widespread use of masks cuts the growth rate by just 10%. Each person now infects 2.25 others, who infect 2.25 others, and so on. Over 15 cycles, 2.25^15 = 191,751 cases. An 80% reduction. Understanding this exponential growth explains how the virus caught the world by surprise even as the pandemic was monitored in real time. Exponential growth just doesn’t make sense, until you do the numbers, and even, they’re still hard to believe. But another counterintuitive aspect of exponential growth is that small decreases in the exponent greatly slow growth. A 10% increase in the exponent can have a massive effect, but even a limited intervention, with a 10% decrease over time, pays large dividends (Fig. 1).
These are very, very simple models. But sophisticated modeling also shows large scale use of masks could slow, even stop pandemics. A 2010 study found that above a certain threshold, widespread use of effective masks can reduce the reproductive number (R) of an influenza virus below 1, and the pandemic stops (25). If face masks were highly effective (well-designed, used properly and consistently), then public use of masks could stop a flu pandemic if used by just 50% of people. If masks were less effective, more than half the population would have to wear them to stop the pandemic. If masks were highly ineffective, they could flatten the curve of the epidemic, but wouldn’t stop it (25). We don’t know which model is most accurate. But does it even matter? In the context of the current pandemic, any of these scenarios would be a huge win.

Real world experience suggests masks work in pandemics
The most compelling evidence of the potential effectiveness of masks in the fight against COVID-19 comes from their use in the real world. Places that have controlled their coronavirus epidemics most effectively – China, South Korea, Hong Kong, Taiwan, Vietnam, Singapore, Kuwait, Czechia, Slovakia, Japan- use masks (Fig. 2). Aside from China, which was the epicenter of the pandemic and so played catchup in developing and implementing its strategy, virtually all of the worst outbreaks are in Western countries that officially advise against mask use, and where there is little culture or practice of mask wearing.
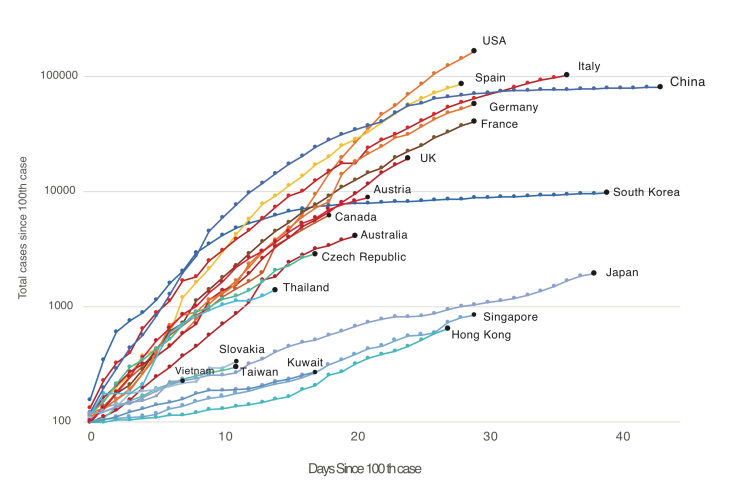
Figure 2. Western countries (US, Canada, Australia, UK, Western Europe) versus countries and territories using masks as part of official government or in practice policy (China, South Korea, Japan, Hong Kong, Taiwan, Vietnam, Thailand, Kuwait, Slovakia, Czech Republic, in blues and greens). Countries with official or unofficial policies of mask usage have controlled the outbreak far better than those without. Note that Austria currently uses masks but has only revised its official policy recently.
Places like China, South Korea, Taiwan, Vietnam, Kuwait, Czechia and Singapore differ greatly in political organization, ranging from communism to democracies, and also in their level of economic development and population density. And strikingly, these countries also differ in their suppression strategies. China implemented a lockdown of Wuhan, shut down industry nationwide, implemented temperature checks and social distancing, tested extensively— and employed masks. Korea responded with an aggressive testing and contact tracing—and masks. Japan has done far less extensive testing than Korea, but shut down schools and large gatherings— and used masks. The pandemic management strategies used by these countries far more diverse than has been appreciated. Arguably one of the few things all these successes share is widespread wearing of masks. And on the other hand, one common factor shared by the pandemic suppression strategies of the US, Canada, the UK and Europe is the decision to discourage the use of masks by the public. This evidence doesn’t prove, but it does very strongly hint that masks are a critical part of these country’s suppression strategies. And by watching countries like Austria that have recently revised their policies, we can test this idea.

What kind of mask? Surgical masks as good as N95s; are improvised masks better than nothing?
Would cloth masks work? Research into the effectiveness of cloth masks is limited (34). Existing research shows homemade masks are- unsurprisingly- inferior to surgical masks. However, they appear to be better than nothing. One laboratory study found homemade masks were half as effective as surgical masks in filtering particles (35). Another study found homemade masks made from various materials stopped virus aerosols, but less well than surgical masks (36). A surgical mask stopped 90% of viral aerosol particles, a dish towel, 72%, linen, 62%, and a cotton T-shirt, 51% (36).
Conclusions
Strong scientific evidence and rational arguments exist for the widespread, public use of facemasks. The principle behind facemasks- they reduce the amount of virus exhaled by infected people, and inhaled by uninfected- suggest they should be a primary tool in combating any respiratory virus. Scientific research, including experimental studies, retrospective studies of the SARS epidemic, hospital studies of COVID-19, and modeling studies, all suggests masks are likely to be effective in controlling the pandemic. Most importantly, the experience of countries using masks against SARS and the current coronavirus pandemic imply that they are effective when used by the public. However, modeling studies and the real-world experience of countries like China and South Korea suggests that neither masks, nor anything else, provides a magic bullet against a pandemic. So strategies should not rely on any single intervention, but rather a wide range of interventions, potentially including masks. Further research and open debate on the effectiveness of masks and other strategies are urgently needed.
Flames GM Brad Treliving does what he can to be ready for NHL reboot
COVID-19
The Persecution of Canada’s “Other” Freedom Convoy Truckers

While thousands of serious criminal cases across Canada are dropped merely due to delays, many Convoy-related prosecutions on trivial charges continue more than three-and-a-half years later. The cases of Freedom Convoy truckers (left to right) Bern Bueckert, Clayton McAllister and Csaba Vizi (whose Volvo is shown at bottom) are still not fully resolved. (Sources of photos: (top left and right) screenshots from documentary Unacceptable?; (top middle) ThankYouTruckers.Substack; (bottom) Donna Laframboise)
On September 8, three and a half years after the 2022 Freedom Convoy departed Ottawa, and five long, stressful months after his trial actually ended, Robert Dinel walked out of court a free man.
Dinel, a Quebec heavy equipment operator who’d behaved entirely peacefully during the protest over Covid restrictions, had been charged with mischief and obstruction of police. Court proceedings were repeatedly delayed — four times alone just this year — until judge Matthew Webber of the Ontario Court of Justice finally stayed the charges on the grounds that Dinel’s Charter rights to a timely trial had been violated.
For Dinel, it was a relief. For Canadians concerned about freedom and justice, his legal ordeal was yet another example of a system gone off the rails.
Most Canadians are aware of the trials of convoy leaders Tamara Lich and Chris Barber, which ended in conviction; they are to be sentenced in October. Few may realize that many more protestors were charged, most for the relatively innocuous infraction of mischief, and have had their cases drag on and on through the courts for more than three years.
The record of Canada’s legal system clearly shows that mischief charges are routinely withdrawn before scarce and expensive court time is expended on relative trivialities. But when it comes to the truckers, the Crown attorneys at the Ottawa courthouse – employees of the Government of Ontario, not the federal government – appear to have lost all perspective. They are on a mission. The sheer intensity of the prosecution of Convoy members looks less like the fair administration of justice than revenge upon people who dared protest the arbitrary and oppressive measures of the Covid years.
The initial police crackdown itself was a mess. Those arrested were passed from police officer to police officer. Officials writing up the paperwork had no direct knowledge of what had actually transpired; extra charges appear to have been tacked on willy nilly. In Dinel’s case, the prosecution doesn’t even know the identity of the tactical officer who pointed a gun at his head and hauled him out of his vehicle on February 18, 2022.
In a police processing trailer four hours after his arrest, Dinel received a medical assessment from a paramedic. Seated and hand-cuffed throughout, the five-foot-three Dinel calmly and repeatedly told police he was in no fit state to be making decisions and that he wanted to speak to a lawyer. “I want to know what I’m signing,” he insisted. But the police officers, who outnumbered him ten-to-one, kept pushing him to sign an undertaking that he wouldn’t return to the protest area. The fact he never got his phone call – that he was denied his Charter right “to retain and instruct [legal] counsel without delay” – should have stopped this case in its tracks. The Crown chose to pursue it, anyway.
A week after Dinel’s mother died in July 2023, he suffered the first of four strokes. In December 2023, one occurred in the courtroom. “My whole face just seized up,” he recalls. “I had another stroke. My whole face drooped, then the judge freaked right out.” An ambulance was summoned and his trial was adjourned. “I hate court,” says Dinel. “It’s hard, you know. It’s stressful, it’s exhausting.” Rather than staying the charges on compassionate grounds, the prosecution continued, with Dinel accompanied by a service dog.
Nova Scotia trucker Guy Meister spent hours in the same paddy wagon as Dinel the day they were arrested. After travelling from his Nova Scotia home to Ottawa for court appearances more than a dozen times – at considerable expense – in May of this year Meister was found guilty of mischief, but not of obstructing police. In late July, he was sentenced to 20 hours of community service, six months’ probation, and ordered to pay a $100 victim surcharge.
The trial for Windsor, Ontario trucker Csaba Vizi began just this month, the same day Robert Dinel’s charges were stayed. Video broadcast around the world in February 2022 shows him being assaulted by multiple police officers after he’d exited his truck and knelt down in the snow with his hands behind his head. None of those officers were themselves charged following this violence. None were forced to raise tens of thousands in lawyers’ fees, as Vizi has. Even protesters who have endured the stress of a trial and been acquitted have still not always walked free and clear, because the Crown has often insisted on filing appeals. As a result, defence lawyers routinely advise Freedom Convoy protesters that their legal nightmare isn’t actually over until an additional 30 days have come and gone. In one instance, the Crown waited until the last afternoon of the last permissible day to file its appeal.
These are just a few examples of what’s been going on in Canada’s justice system, one already beset by long delays for cases involving far more serious crimes. Credible news reports suggest that the majority of criminal cases in Ontario aren’t even making it to trial, with sexual assault
charges dropped because of delays. Yet the Convoy prosecutions continue.
Many people insist Covid is over, that we should all move on. But the legal persecution of the truckers who bravely protested government overreach in the bitter winter of early 2022 is far from over.
Donna Laframboise is an independent journalist and photographer. A former vice-president of the Canadian Civil Liberties Association, she is the author of Thank You, Truckers! Canada’s Heroes & Those Who Helped Them.
The original, full-length version of this article was recently published in C2C Journal.
COVID-19
Canada’s COVID mandates linked to rise in ‘unexplained deaths’: new report
From LifeSiteNews
The report drew on data from Statistics Canada and essentially concluded that thousands died not from the COVID-19 virus but because of public health rules.
A new report released by one of Canada’s leading constitutional freedom groups has raised alarm bells over the “harms caused” by COVID-19 lockdowns and injections imposed by various levels of government as well as a rise in unexplained deaths and bloated COVID-19 death statistics.
The report, titled “Post-COVID Canada: The rise in unexpected deaths,” was released September 3 by the Justice Centre for Constitutional Freedoms (JCCF). It found three key findings that arose from various Canadian governments’ handling of COVID.
“The report raises urgent concerns about the accuracy of Covid death reports, the harmful impacts of lockdowns and vaccine mandates, and the ongoing trend of unexplained deaths in Canada,” the JCCF noted.
The report drew on data from Statistics Canada and essentially concluded that thousands of Canadians died not from the COVID-19 virus itself but rather because of public health rules and vaccine mandates put in place.
The first main finding is that so called “unexpected” or “excess” deaths were significantly higher in 2022 after most lockdowns were in place but also at a time when most had had at least one injection of the mRNA COVID jabs.
The report found that there were “14,950 unexpected deaths in 2020, 13,510 unexpected deaths in 2021, and 31,370 unexpected deaths in 2022.”
“Canadians died at an alarming rate between 2020 and 2024. While public health officials and politicians claim that COVID was the cause, the data show that Covid death statistics were inflated and that thousands of Canadians died due to lockdowns, vaccine mandates, and their downstream effects,” the JCCF noted.
The report also found that deaths rose after the rollout of the COVID injections, noting that by the end of 2021, over 80 percent of Canadians were “fully vaccinated for Covid.”
“In 2022, however, Covid deaths increased to an all-time high of 19,906 – a 22 percent increase over 2020 Covid deaths,” the JCCF mentioned.
The report also concluded that 10,000 deaths among seniors in 2020 and 2021 were “misclassified as Covid deaths.”
However, the JCCF observed that when looking at the statistics, in 2020 and 2021, Statistics Canada reported “690 fewer deaths from respiratory and pulmonary disease; 3,270 fewer deaths from respiratory infections and lung disease; 6,100 fewer deaths from vascular and other dementia diseases; and 1,000 fewer deaths from Parkinson’s, Alzheimer’s, and other degenerative diseases of the nervous system.”
“The data is clear: deaths that would otherwise have been attributed to these illnesses were attributed to Covid,” the JCCF stated.
LifeSiteNews has published an extensive amount of research on the dangers of the experimental COVID mRNA jabs that include heart damage and blood clots.
The mRNA shots have also been linked to a multitude of negative and often severe side effects in children, and all have connections to cell lines derived from aborted babies.
Deaths linked to COVID lockdowns and ‘unknown’ causes spiked in 2022
In the report, the JCCF observed that when it comes to deaths “linked” to COVID lockdowns, drug overdose, delayed medical procedures, and alcohol-related deaths “increased significantly during lockdowns.”
The data, which Statistics Canada attributed to deaths from “unknown causes” for “Canadians under 45, who passed away in 2022, over 15 percent of these did not have a cause of death.”
JCCF research and education coordinator Benjamin Klassen, who is also the lead author of the report, said, “This report shows that Canadians were seriously misled about Covid and about the safety and effectiveness of government lockdowns and vaccine mandates.”
“Governments not only failed to protect lives but also contributed to thousands of preventable deaths with their freedom-violating policies,” he observed.
Klassen noted that despite government “assurances” that its policies would “save lives,” the reality is that the “data reveals the opposite.”
“Lockdowns, delayed healthcare, and rushed vaccine mandates all appear to have significantly contributed to high numbers of additional and unexpected deaths from causes other than Covid,” he observed.
“Higher death rates in Canada have continued to rise – especially evident among young Canadians.”
Report recommends investigation into COVID jabs and lockdowns
The JCCF report recommends that three steps be urgently taken at once to ensure that transparency and accountability to the public happens.
The first recommendation calls for both Statistics Canada and all levels of government to “provide timely and accurate death data.”
The second recommendation is a call for an investigation into the “harms caused by Covid lockdowns and vaccines.”
“Canadians deserve an independent and transparent inquiry into the short-term and long-term harms caused by government responses to Covid,” the report states.
The third recommendation calls for the protection of “freedom of expression for professionals.”
“Canadian professionals need legislation that prohibits colleges of physicians and surgeons and other professional regulatory bodies from censoring and punishing professionals who express dissenting views on public health issues,” the report says.
It should be noted that, after Premier Danielle Smith took over, the provincial government of Alberta commissioned Dr. Gary Davidson to investigate the previous administration’s handling of COVID-19.
Davidson’s report, which was made public earlier this year, recommended an immediate halt to the experimental jabs for healthy children and teenagers, citing the risks the shots pose.
From about March 2020 to mid-2022, most of Canada was under various COVID-19 mandates and lockdowns, including mask mandates, at the local, provincial, and federal levels.
In October 2021, then-Prime Minister Justin Trudeau announced unprecedented COVID-19 jab mandates for all federal workers and those in the transportation sector, saying the unjabbed would no longer be able to travel by air, boat, or train, both domestically and internationally.
This policy resulted in thousands losing their jobs or being placed on leave for non-compliance.
-

 Crime2 days ago
Crime2 days agoAlleged Killer Of Charlie Kirk Caught
-

 Opinion2 days ago
Opinion2 days agoThe Charlie Kirk I Knew
-

 Crime2 days ago
Crime2 days ago‘Dark Moment For America’: Trump Addresses Nation After Kirk Assassination
-

 Bruce Dowbiggin1 day ago
Bruce Dowbiggin1 day agoKirk’s Killing: Which Side Can Count on the Military’s Loyalty Now?
-

 Crime1 day ago
Crime1 day agoFormer FBI Agent Says Charlie Kirk Assassination May Have Been ‘A Professional Hit’
-

 Alberta1 day ago
Alberta1 day agoAlberta deserves a police force that actually reflects its values
-

 Crime2 days ago
Crime2 days agoCharlie Kirk ASSASSINATED
-

 Alberta1 day ago
Alberta1 day agoProvincial pension plan could boost retirement savings for Albertans