Health
Thinking of taking a flu shot? Read this first…

From the World Council For Health
It’s not just that they’re ineffective, they also cause harm. Learn about safe alternatives such as Vitamin D, quercetin and zinc.
If you’re of a certain age or demographic and in the northern hemisphere, chances are you’re being invited or encouraged to get a flu vaccine. The claim is that flu vaccines protect you and others from coming down with flu – and that if you do get it, the symptoms will be mild. So, is this true?
Many scientists see the flu shot as an unnecessary measure. For one thing, there’s a big question over whether the flu vaccine even works, particularly for older people, for whom it is recommended. Studies show that the vaccines often do not match the circulating viruses and no significant effects on serious complications or hospitalizations have been demonstrated.
You’d think that vaccinating people against flu would lead to a reduction in deaths from flu. But figures show that this isn’t the case. In fact, even though the number of flu shots given has increased more than eightfold, the number of flu-associated deaths has remained more or less unchanged.
There’s a logical explanation, and it goes like this:
Antibodies are not enough
Flu vaccines, like any other vaccine, primarily rely on the so-called Th2 antibody response. This generates antibodies to help the body fight off the influenza virus once it enters the bloodstream. What vaccines don’t do is impact the first line of defence in the nasal mucosa. This part of the innate immune system does not use antibodies, and it is here where respiratory viruses replicate.
This is why vaccines for respiratory viruses will never prevent infection or the transmission of the disease.
The immune response to vaccinations also decreases with age, which further reduces the already weak effect of vaccination in older people. Studies bear this out. In particular, a 2012 article in the British Medical Journal quoted an independent study that looked at data from 1967 to 2012 and concluded there isn’t strong evidence showing that the flu vaccine consistently protects people. While it does offer some protection for young, healthy adults who usually don’t face serious flu complications, the researchers noted that there is not enough evidence to support its effectiveness for older adults (65 and older), who account for more than 90% of flu-related deaths.
Recent research into the efficacy of flu shots also reveals their limitations
- In 2020, Anderson et al. showed that influenza vaccination of 60 to 70 year olds in England and Wales had no discernible positive impact on hospitalization or deaths:
- Another study in Japan reported on 83,146 individuals aged 65 years and followed them up over six years. In 2023, the incidence of hospitalization for influenza did not differ significantly by vaccination and the claimed protective effectiveness against incidence waned quickly after four or five months.
- Another 2020 study from Anderson and team analysed data covering 170 million episodes of care and 7.6 million deaths. Turning 65 was associated with a statistically and clinically significant increase in rate of seasonal influenza vaccination. However, no evidence indicated that vaccination reduced hospitalizations or mortality among elderly persons. The study points out that estimates were precise enough to rule out results from many previous studies.
This is not just a concern for the elderly but for all those with weakened immune systems, including those undergoing immunosuppressive treatments, or individuals with chronic health conditions. In such cases, the Th2 response may not produce enough protective antibodies to effectively combat the virus, leading to a higher risk of severe illness.
Here’s another reason to exercise caution of the flu vaccine:
Flu vaccines actually SPREAD the virus
Controlled studies published in the Proceedings of the National Academy of Sciences (PNAS) find that people who receive flu shots emit 630% more flu virus particles into the air compared to non-vaccinated people. In other words, flu vaccines spread the flu!
Physicians for Informed Consent has produced this concise summary of facts that you, your loved ones and your doctor should consider before a potential injection.
All this leads to an important next question:
If the flu shot isn’t a good idea, what is?
The flu shots’ limitations make the prevention and treatment of flu with nutritional supplements like Vitamin D, Quercetin, and Zinc more appealing and safe. These supplements not only enhance the immune response but also offer additional antiviral and anti-inflammatory benefits:
Vitamin D protects the lungs and airways – and much more besides
Studies have shown that Vitamin D supplementation can significantly reduce the risk of influenza infections by enhancing the body’s immune response. It works by modulating the expression of inflammatory cytokines and increasing macrophage function, which are essential for fighting off infections.
Moreover, Vitamin D has been found to protect the lungs and airways through the antimicrobial peptide cathelicidin, which has both antibacterial and antiviral properties. Vitamin D supplementation shows promise in reducing the risk and severity of respiratory infections, including influenza. The evidence suggests that consistent Vitamin D intake can lower the incidence of acute respiratory infections, shorten the duration of symptoms, and enhance immune response, particularly in the elderly. These benefits can translate into reduced hospitalizations and deaths due to flu, making Vitamin D a valuable component in flu prevention and management strategies.
Quercetin: a powerful antiviral and zinc’s vital wingman
Quercetin is a flavonoid found in many fruits and vegetables, known for its antiviral, anti-inflammatory, and antioxidant properties. It has been shown to inhibit the entry and replication of viruses in lung cells, making it a potent candidate for managing respiratory infections like the flu. Quercetin also acts as a zinc ionophore, facilitating the transport of zinc into cells, which enhances its antiviral effects. Studies suggest that the co-administration of Quercetin and Vitamin C can exert a synergistic antiviral action, further boosting immune response and reducing viral replication
Zinc: helps prevent and reduce infection severity and duration
Zinc is an essential mineral that supports various cellular functions of both the innate and adaptive immune systems. It interferes with the process that certain cold viruses use to multiply, thereby reducing the severity and duration of infections. Zinc is particularly important for the recruitment and activity of neutrophil granulocytes, natural killer cells, and T cells, all of which play critical roles in the immune response. Supplementation with zinc has been supported by evidence showing its effectiveness in preventing viral infections and reducing their severity.
In summary…
The questionable efficiency and safety of the flu vaccine raises important concerns that cannot be overlooked. Alternative approaches such as supplementing vitamin D, quercetin and zinc, are one way to enhance immunity without the risks associated with traditional vaccinations.
Moreover, the potential for the production of IgG4 antibodies as a response to the vaccine illustrates a complex interaction between immunization and immune system dynamics, where the very act of repeated vaccination may inadvertently lead to a weakened response against certain influenza strains. This effect can also result in the weakening of the immune system in general to fight infections and cancer. This highlights the need for continued research and dialogue about the benefits and risks of flu vaccination versus alternative preventive strategies.
As we navigate through flu seasons, it is crucial to remain informed and consider individualized approaches to immune health. Ultimately, a well-rounded strategy that includes lifestyle choices, nutritional support, and an understanding of the science behind flu immunization could empower individuals to make informed decisions that best suit their health needs. The World Council for Health stands for a better way.
Please subscribe to World Council for Health.
For the full experience, upgrade your subscription.
References:
1. Berndt, Christina: ‘Experten mit den falschen Freunden’, http://www.sueddeutsche.de/
2. http://influenza.rki.de/
3. http://www.gpk.de/
4. Committee concerning Influenza Pandemic (H1N1), 2009, http://www.who.int/ihr/emerg_
5. Di Pietrantonj, C.; Rivetti, A.; Bawazeer, G.A.; Al-Ansary, L.A.; Ferroni, E.: ‘Vaccines for preventing influenza in healthy adults’, in: Cochrane Database of Systematic Reviews, 2010, 7., Art. No.: CD001269, DOI: 10.1002/14651858.CD001269.
6. Wittig, Frank. Die weiße Mafia: Wie Ärzte und die Pharmaindustrie unsere Gesundheit aufs Spiel setzen, 2012Yan J, Grantham M, Pantelic J, Bueno de Mesquita PJ, Albert B, Liu F, Ehrman S, Milton DK; EMIT Consortium. Infectious virus in exhaled breath of symptomatic seasonal influenza cases from a college community. Proc Natl Acad Sci U S A. 2018 Jan 30;115(5):1081-1086. doi: 10.1073/pnas.1716561115. Epub 2018 Jan 18. PMID: 29348203; PMCID: PMC5798362.
The World Council for Health (WCH) is a grassroots, people-powered, non-profit initiative based in Bath, United Kingdom that seeks to broaden public health knowledge and sense-making through science and shared wisdom.
WCH was founded by Dr Jennifer Hibberd, a pediatric dental surgeon, and Dr Tess Lawrie, a medical doctor and former consultant to the World Health Organization, in September 2021 in response to growing distrust in local, national, and global public health authorities leaving people in fear and confused regarding how to best care for themselves, their families, and their communities.
The World Council for Health has more than 200 Coalition Partners in over 50 countries around the world and is currently in the process of decentralization, having activated more than 25 WCH Country Councils.
Addictions
No, Addicts Shouldn’t Make Drug Policy

By Adam Zivo
Canada’s policy of deferring to the “leadership” of drug users has proved predictably disastrous. The United States should take heed.
[This article was originally published in City Journal, a public policy magazine and website published by the Manhattan Institute for Policy Research]
Progressive “harm reduction” advocates have insisted for decades that active users should take a central role in crafting drug policy. While this belief is profoundly reckless—akin to letting drunk drivers set traffic laws—it is now entrenched in many left-leaning jurisdictions. The harms and absurdities of the position cannot be understated.
While the harm-reduction movement is best known for championing public-health interventions that supposedly minimize the negative effects of drug use, it also has a “social justice” component. In this context, harm reduction tries to redefine addicts as a persecuted minority and illicit drug use as a human right.
This campaign traces its roots to the 1980s and early 1990s, when “queer” activists, desperate to reduce the spread of HIV, began operating underground needle exchanges to curb infections among drug users. These exchanges and similar efforts allowed some more extreme LGBTQ groups to form close bonds with addicts and drug-reform advocates. Together, they normalized the concept of harm reduction, such that, within a few years, needle exchanges would become officially sanctioned public-health interventions.
The alliance between these more radical gay rights advocates and harm-reduction proponents proved enduring. Drug addiction remained linked to HIV, and both groups shared a deep hostility to the police, capitalism, and society’s “moralizing” forces.
In the 1990s, harm-reduction proponents imitated the LGBTQ community’s advocacy tactics. They realized that addicts would have greater political capital if they were considered a persecuted minority group, which could legitimize their demands for extensive accommodations and legal protections under human rights laws. Harm reductionists thus argued that addiction was a kind of disability, and that, like the disabled, active users were victims of social exclusion who should be given a leading role in crafting drug policy.
These arguments were not entirely specious. Addiction can reasonably be considered a mental and physical disability because illicit drugs hijack users’ brains and bodies. But being disabled doesn’t necessarily mean that one is part of a persecuted group, much less that one should be given control over public policy.
More fundamentally, advocates were wrong to argue that the stigma associated with drug addiction was senseless persecution. In fact, it was a reasonable response to anti-social behavior. Drug addiction severely impairs a person’s judgement, often making him a threat to himself and others. Someone who is constantly high and must rob others to fuel his habit is a self-evident danger to society.
Despite these obvious pitfalls, portraying drug addicts as a persecuted minority group became increasingly popular in the 2000s, thanks to several North American AIDS organizations that pivoted to addiction work after the HIV epidemic subsided.
In 2005, the Canadian HIV/AIDS Legal Network published a report titled “Nothing about us without us.” (The nonprofit joined other groups in publishing an international version in 2008.) The 2005 report included a “manifesto” written by Canadian drug users, who complained that they were “among the most vilified and demonized groups in society” and demanded that policymakers respect their “expertise and professionalism in addressing drug use.”
The international report argued that addiction qualified as a disability under international human rights treaties, and called on governments to “enact anti-discrimination or protective laws to reduce human rights violations based on dependence to drugs.” It further advised that drug users be heavily involved in addiction-related policy and decision-making bodies; that addict-led organizations be established and amply funded; and that “community-based organizations . . . increase involvement of people who use drugs at all levels of the organization.”
While the international report suggested that addicts could serve as effective policymakers, it also presented them as incapable of basic professionalism. In a list of “do’s and don’ts,” the authors counseled potential employers to pay addicts in cash and not to pass judgment if the money were spent on drugs. They also encouraged policymakers to hold meetings “in a low-key setting or in a setting where users already hang out,” and to avoid scheduling meetings at “9 a.m., or on welfare cheque issue day.” In cases where addicts must travel for policy-related work, the report recommended policymakers provide “access to sterile injecting equipment” and “advice from a local person who uses drugs.”
The international report further asserted that if an organization’s employees—even those who are former drug users—were bothered by the presence of addicts, then management should refer those employees to counselling at the organization’s expense. “Under no circumstances should [drug addicts] be reprimanded, singled out or made to feel responsible in any way for the triggering responses of others,” stressed the authors.
Reflecting the document’s general hostility to recovery, the international report emphasized that former drug addicts “can never replace involvement of active users” in public policy work, because people in recovery “may be somewhat disconnected from the community they seek to represent, may have other priorities than active users, may sometimes even have different and conflicting agenda, and may find it difficult to be around people who currently use drugs.”
Subscribe for free to get BTN’s latest news and analysis – or donate to our investigative journalism fund.
The messaging in these reports proved highly influential throughout the 2000s and 2010s. In Canada, federal and provincial human rights legislation expanded to protect active addicts on the basis of disability. Reformers in the United States mirrored Canadian activists’ appeals to addicts’ “lived experience,” albeit with less success. For now, American anti-discrimination protections only extend to people who have a history of addiction but who are not actively using drugs.
The harm reduction movement reached its zenith in the early 2020s, after the Covid-19 pandemic swept the world and instigated a global spike in addiction. During this period, North American drug-reform activists again promoted the importance of treating addicts like public-health experts.
Canada was at the forefront of this push. For example, the Canadian Association of People Who Use Drugs released its “Hear Us, See Us, Respect Us” report in 2021, which recommended that organizations “deliberately choose to normalize the culture of drug use” and pay addicts $25-50 per hour. The authors stressed that employers should pay addicts “under the table” in cash to avoid jeopardizing access to government benefits.
These ideas had a profound impact on Canadian drug policy. Throughout the country, public health officials pushed for radical pro-drug experiments, including giving away free heroin-strength opioids without supervision, simply because addicts told researchers that doing so would be helpful. In 2024, British Columbia’s top doctor even called for the legalization of all illicit drugs (“non-medical safer supply”) primarily on the basis of addict testimonials, with almost no other supporting evidence.
For Canadian policymakers, deferring to the “lived experiences” and “leadership” of drug users meant giving addicts almost everything they asked for. The results were predictably disastrous: crime, public disorder, overdoses, and program fraud skyrocketed. Things have been less dire in the United States, where the harm reduction movement is much weaker. But Americans should be vigilant and ensure that this ideology does not flower in their own backyard.
Subscribe to Break The Needle.
Our content is always free – but if you want to help us commission more high-quality journalism,
consider getting a voluntary paid subscription.
COVID-19
Canadian gov’t to take control of vaccine injury program after reports of serious mismanagement

From LifeSiteNews
The Canadian federal gov’t will take over the Vaccine Injury Support Program from Oxaro by March 2026 following reports of misallocated funds, unresolved claims, and unprofessional conduct.
The federal government is taking over Canada’s vaccine injury program after reports have discovered mismanagement.
The Public Health Agency of Canada (PHAC) is expected to take control of the Vaccine Injury Support Program (VISP) beginning on March 31, 2026, after a Global News report exposed the program for misallocating taxpayer funds and disregarding many vaccine-injured Canadians.
“We will publicly share further details on how the program will be delivered under PHAC when they become available,” Guillaume Bertrand, director of communications for Health Minister Marjorie Michel, told Global News.
Bertrand revealed that the government contract with Oxaro, the company tasked with running the VISP, will end in March, after which the federal government will take control.
“This is also part of our commitment to significantly reducing reliance on external consultants, while improving the capacity of the public service to hire expertise in-house,” Bertrand said.
Canada’s VISP was launched in December 2020 after the Canadian government gave vaccine makers a shield from liability regarding COVID-19 jab-related injuries; however, mismanagement within the program has led to many injured Canadians still waiting to receive compensation, while government contractors grow richer.
In July, Conservatives penned a letter calling for an investigation into the failing program, saying, “Despite the $50 million contract, over 1,700 of the 3,100 claims remain unresolved. Families dealing with life-altering injuries have been left waiting years for answers and support they were promised.”
Furthermore, the claims do not represent the total number of Canadians injured by the allegedly “safe and effective” COVID shots, as inside memos have revealed that Public Health Agency of Canada (PHAC) officials neglected to report all adverse effects from COVID shots and even went as far as telling staff not to report all events.
The PHAC’s downplaying of vaccine injuries is of little surprise to Canadians, as a 2023 secret memo revealed that the federal government purposefully hid adverse event reports so as not to alarm Canadians.
Of the $50.6 million that Oxaro Inc., has received, $33.7 million has been spent on administrative costs, compared to only $16.9 million going to vaccine-injured Canadians.
The letter further documented former VISP employees’ concerns that the program lacked professionalism and outlining what Conservatives described as “a fraternity house rather than a professional organization responsible for administering health-related claims.”
“Reports of constant workplace drinking, ping pong, and Netflix are a slap in the face to taxpayers and the thousands of Canadians waiting for support for life altering injuries,” the letter continued.
The federal government has ordered an audit into VISP. In late July, PHAC revealed that it is expediting its audit in light of reports of mismanagement within Oxaro.
-

 International1 day ago
International1 day agoTrump sues New York Times for $15 billion over ‘malicious, defamatory’ election coverage
-

 Crime2 days ago
Crime2 days agoStruggle for control of the Sinaloa Carel has ramifications for Canada
-
 Crime2 days ago
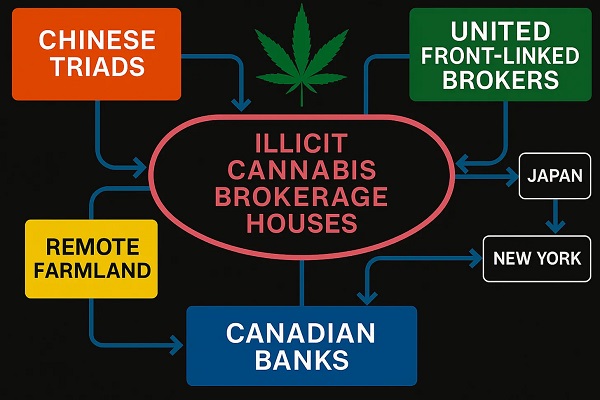
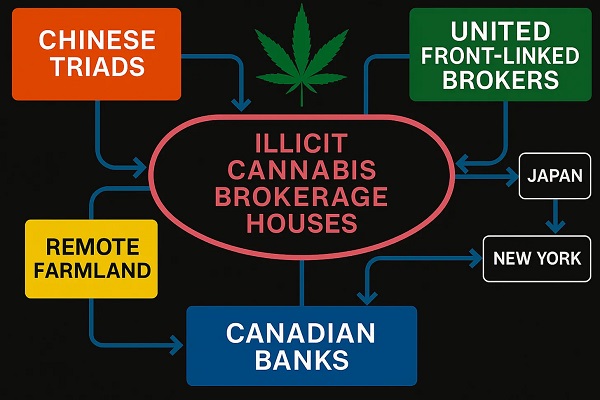
Crime2 days agoU.S. Lawmakers Confront Chinese Government Conspiracy Behind Marijuana Boom
-

 Censorship Industrial Complex2 days ago
Censorship Industrial Complex2 days agoThe FCC Should Let Jimmy Kimmel Be
-
 Crime20 hours ago
Crime20 hours agoFrom Vancouver to Oklahoma: Canadian Murder Case and CCP ‘Police Station’ Links Align U.S. Testimony and The Bureau’s PRC Pot Investigations
-

 Alberta1 day ago
Alberta1 day agoEducation negotiations update: Minister Horner
-

 Business2 days ago
Business2 days agoThe Real Reason Tuition Keeps Going Up at Canada’s Universities
-

 Addictions1 day ago
Addictions1 day agoNo, Addicts Shouldn’t Make Drug Policy






