Health
Recovered ‘brain dead’ man dancing at sister’s wedding reminds us organ donors are sometimes alive

TJ Hoover and his sister on her wedding day
From LifeSiteNews
Since brain dead people are not dead, it is not surprising that the only multicenter, prospective study of brain death found that the majority of brains from ‘brain dead’ people were not severely damaged at autopsy.
In 2021, a supposedly brain dead man, Anthony Thomas “TJ” Hoover II, opened his eyes and looked around while being wheeled to the operating room to donate his organs. Hospital staff at Baptist Health hospital in Richmond, Kentucky assured his family that these were just “reflexes.”
But organ preservationist Natasha Miller also thought Hoover looked alive. “He was moving around – kind of thrashing. Like, moving, thrashing around on the bed,” said Miller in an NPR interview. “And then when we went over there, you could see he had tears coming down. He was visibly crying.” Thankfully, the procedure was called off, and Hoover was able to recover and even dance at his sister’s wedding this past summer.
Last month, this case was brought before a U.S. House subcommittee investigating organ procurement organizations. Whistleblowers claimed that even after two doctors refused to remove Hoover’s organs, Kentucky Organ Donor Affiliates ordered their staff to find another doctor to perform the surgery.
Because brain death is a social construct and not death itself, I can tell you exactly how many “brain dead” patients are still alive: all of them. When brain death was first proposed by an ad hoc committee at Harvard Medical School in 1968, the committee admitted that these people are not dead, but rather “desperately injured.” They thought that these neurologically injured people were a burden to themselves and others, and that society would be better served if we redefined them as being “dead.” They described their reasoning this way:
Our primary purpose is to define irreversible coma as a new criterion for death. There are two reasons why there is need for a definition: (1) Improvements in resuscitative and supportive measures have led to increased efforts to save those who are desperately injured. Sometimes these efforts have only partial success so that the result is an individual whose heart continues to beat but whose brain is irreversibly damaged. The burden is great on patients who suffer permanent loss of intellect, on their families, on the hospitals, and on those in need of hospital beds already occupied by these comatose patients. (2) Obsolete criteria for the definition of death can lead to controversy in obtaining organs for transplantation.
Since brain dead people are not dead, it is not surprising that the only multicenter, prospective study of brain death found that the majority of brains from “brain dead” people were not severely damaged at autopsy – and 10 actually looked normal. Dr. Gaetano Molinari, one of the study’s principal investigators, wrote:
[D]oes a fatal prognosis permit the physician to pronounce death? It is highly doubtful whether such glib euphemisms as “he’s practically dead,” … “he can’t survive,” … “he has no chance of recovery anyway,” will ever be acceptable legally or morally as a pronouncement that death has occurred.
But history shows that despite Dr. Molinari’s doubts, “brain death,” a prognosis of possible death, went on to be widely accepted as death per se. Brain death was enshrined into US law in 1981 under the Uniform Determination of Death Act. Acceptance of this law has allowed neurologically disabled people to be redefined as “dead” and used as organ donors. Unfortunately, most of these people do not, like TJ Hoover, wake up in time. They suffer death through the harvesting of their organs, a procedure often performed without the benefit of anesthesia.
Happily, some do manage to avoid becoming organ donors and go on to receive proper medical treatment. In 1985, Jennifer Hamann was thrown into a coma after being given a prescription that was incompatible with her epilepsy medication. She could not move or sign that she was awake and aware when she overheard doctors saying that her husband was being “completely unreasonable” because he would not donate her organs. She went on to made a complete recovery and became a registered nurse.
Zack Dunlap was declared brain dead in 2007 following an ATV accident. Even though his cousin demonstrated that Zack reacted to pain, hospital staff told his family that it was just “reflexes.” But as Zack’s reactions became more vigorous, the staff took more notice and called off the organ harvesting team that was just landing via helicopter to take Zack’s organs. Today, Zack leads a fully recovered life.
Colleen Burns was diagnosed “brain dead” after a drug overdose in 2009, but wasn’t given adequate testing and awoke on the operating table just minutes before her organ harvesting surgery. Because the Burns family declined to sue, the hospital only received a slap on the wrist: the State Health Department fined St. Joseph’s Hospital Health Center in Syracuse, New York, just $6,000.
In 2015, George Pickering III was declared brain dead, but his father thought doctors were moving too fast. Armed and dangerous, he held off a SWAT team for three hours, during which time his son began to squeeze his hand on command. “There was a law broken, but it was broken for all the right reasons. I’m here now because of it,” said George III.
Trenton McKinley, a 13-year-old boy, suffered a head injury in 2018 but regained consciousness after his parents signed paperwork to donate his organs. His mother told CBS News that signing the consent to donate allowed doctors to continue Trenton’s intensive care treatment, ultimately giving him time to wake up.
Doctors often say that cases like these prove nothing, and that they are obviously the result of misdiagnosis and medical mistakes. But since all these people were about to become organ donors regardless of whether their diagnoses were correct, I doubt they find the “mistake” excuse comforting.
However, Jahi McMath was indisputably diagnosed as being “brain dead” correctly. She was declared brain dead by three different doctors, she failed three apnea tests, and she had four flat-line EEGs, as well as a cerebral perfusion scan showing “no flow.” But because her parents refused to make her an organ donor and insisted on continuing her medical care, McMath recovered to the point of being able to follow commands. Two neurologists later testified that she was no longer brain dead, but a in minimally conscious state. Her case shows that people correctly declared “brain dead” can still recover.
READ: Woman with no brainwave activity wakes up after hearing her daughter’s voice
Brain death is not death because the brain death concept does not reflect the reality of the phenomenon of death. Therefore, any guideline for its diagnosis will have no basis in scientific facts. People declared brain dead are neurologically disabled, but they are still alive. “Brain dead” organ donation is a concealed form of euthanasia.
Heidi Klessig MD is a retired anesthesiologist and pain management specialist who writes and speaks on the ethics of organ harvesting and transplantation. She is the author of “The Brain Death Fallacy” and her work may be found at respectforhumanlife.com.
Alberta
A Christmas wish list for health-care reform

From the Fraser Institute
By Nadeem Esmail and Mackenzie Moir
It’s an exciting time in Canadian health-care policy. But even the slew of new reforms in Alberta only go part of the way to using all the policy tools employed by high performing universal health-care systems.
For 2026, for the sake of Canadian patients, let’s hope Alberta stays the path on changes to how hospitals are paid and allowing some private purchases of health care, and that other provinces start to catch up.
While Alberta’s new reforms were welcome news this year, it’s clear Canada’s health-care system continued to struggle. Canadians were reminded by our annual comparison of health care systems that they pay for one of the developed world’s most expensive universal health-care systems, yet have some of the fewest physicians and hospital beds, while waiting in some of the longest queues.
And speaking of queues, wait times across Canada for non-emergency care reached the second-highest level ever measured at 28.6 weeks from general practitioner referral to actual treatment. That’s more than triple the wait of the early 1990s despite decades of government promises and spending commitments. Other work found that at least 23,746 patients died while waiting for care, and nearly 1.3 million Canadians left our overcrowded emergency rooms without being treated.
At least one province has shown a genuine willingness to do something about these problems.
The Smith government in Alberta announced early in the year that it would move towards paying hospitals per-patient treated as opposed to a fixed annual budget, a policy approach that Quebec has been working on for years. Albertans will also soon be able purchase, at least in a limited way, some diagnostic and surgical services for themselves, which is again already possible in Quebec. Alberta has also gone a step further by allowing physicians to work in both public and private settings.
While controversial in Canada, these approaches simply mirror what is being done in all of the developed world’s top-performing universal health-care systems. Australia, the Netherlands, Germany and Switzerland all pay their hospitals per patient treated, and allow patients the opportunity to purchase care privately if they wish. They all also have better and faster universally accessible health care than Canada’s provinces provide, while spending a little more (Switzerland) or less (Australia, Germany, the Netherlands) than we do.
While these reforms are clearly a step in the right direction, there’s more to be done.
Even if we include Alberta’s reforms, these countries still do some very important things differently.
Critically, all of these countries expect patients to pay a small amount for their universally accessible services. The reasoning is straightforward: we all spend our own money more carefully than we spend someone else’s, and patients will make more informed decisions about when and where it’s best to access the health-care system when they have to pay a little out of pocket.
The evidence around this policy is clear—with appropriate safeguards to protect the very ill and exemptions for lower-income and other vulnerable populations, the demand for outpatient healthcare services falls, reducing delays and freeing up resources for others.
Charging patients even small amounts for care would of course violate the Canada Health Act, but it would also emulate the approach of 100 per cent of the developed world’s top-performing health-care systems. In this case, violating outdated federal policy means better universal health care for Canadians.
These top-performing countries also see the private sector and innovative entrepreneurs as partners in delivering universal health care. A relationship that is far different from the limited individual contracts some provinces have with private clinics and surgical centres to provide care in Canada. In these other countries, even full-service hospitals are operated by private providers. Importantly, partnering with innovative private providers, even hospitals, to deliver universal health care does not violate the Canada Health Act.
So, while Alberta has made strides this past year moving towards the well-established higher performance policy approach followed elsewhere, the Smith government remains at least a couple steps short of truly adopting a more Australian or European approach for health care. And other provinces have yet to even get to where Alberta will soon be.
Let’s hope in 2026 that Alberta keeps moving towards a truly world class universal health-care experience for patients, and that the other provinces catch up.
Health
FDA warns ‘breast binder’ manufacturers to stop marketing to gender-confused girls

From LifeSiteNews
Dr. Marty Makary took aim at the transgender-medical-industrial complex that has exploded in recent years during a recent press conference.
Food and Drug Administration (FDA) commissioner Dr. Marty Makary has sternly warned companies manufacturing “breast binders” to cease marketing and supplying their product to gender-confused girls seeking to make their bodies appear masculine.
“Today the FDA is taking action,” said Makary in a press conference. “We are sending warning letters to 12 manufacturers and retailers for illegal marketing of breast binders for children, for the purposes of treating gender dysphoria.”
“Breast binders are a class one medical device with legitimate medical users, such as being used by women after breast cancer surgery,” but “these binders are not benign,” he cautioned. “Long-term usage has been associated with pain, compromised lung function, and even difficulty breast feeding later in life.”
“The warning letters will formally notify the companies of their significant regulatory violations and require prompt corrective action,” said the FDA head.
.@DrMakaryFDA: “Today the FDA is taking action. We are sending warning letters to 12 manufacturers and retailers for illegal marketing of breast binders for children, for the purposes of treating gender dysphoria.” pic.twitter.com/6JNAy36223
— HHS Rapid Response (@HHSResponse) December 18, 2025
The warning letter addressed to California manufacturer, GenderBender, notes that the company’s website states that “[c]hest binding is the practice of compressing breast mass into a more masculine shape, often done in the LGBTQ community for gender euphoria.”
“Your firm should take prompt action to address any violations identified in this letter. Failure to adequately address this matter may result in regulatory action being initiated by the FDA without further notice. These actions include, but are not limited to, seizure and injunction,” advised the FDA.
During his presentation, Makary took aim at the transgender-medical-industrial complex that has exploded in recent years.
“One of the most barbaric features of a society is the genital mutilation of its children,” observed Makary.
“Pushing transgender ideology in children is predatory, it’s wrong, and it needs to stop,” he declared.
“This ideology is a belief system that some teachers, some pediatricians, and others are selling to children without their parents knowing sometimes, or with a deliberate attempt to remove parents from the decision making,” Makary explained.
To witness society “putting kids on a path of chest binders, drugs, castration, mastectomies, and other procedures is a path that now many kids regret,” he lamented, as he pointed to Chloe Cole, who has reverted to her God-given femininity after undergoing so-called “gender-affirming” surgery as a teen.
Cole is a leading voice for young people who have “detransitioned” after having medically, surgically, and socially attempted to “transition” to a member of the opposite sex.
.@DrMakaryFDA: “Pushing transgender ideology in children is predatory, it's wrong, and it needs to stop.” pic.twitter.com/TXxWNEtNZk
— HHS Rapid Response (@HHSResponse) December 18, 2025
-

 Alberta1 day ago
Alberta1 day agoAlberta Next Panel calls to reform how Canada works
-

 Automotive2 days ago
Automotive2 days agoCanada’s EV gamble is starting to backfire
-

 International6 hours ago
International6 hours agoGeorgia county admits illegally certifying 315k ballots in 2020 presidential election
-
 Digital ID24 hours ago
Digital ID24 hours agoCanadian government launches trial version of digital ID for certain licenses, permits
-

 Business23 hours ago
Business23 hours agoThe “Disruptor-in-Chief” places Canada in the crosshairs
-

 Agriculture1 day ago
Agriculture1 day agoEnd Supply Management—For the Sake of Canadian Consumers
-

 Alberta6 hours ago
Alberta6 hours agoCalgary’s new city council votes to ban foreign flags at government buildings
-
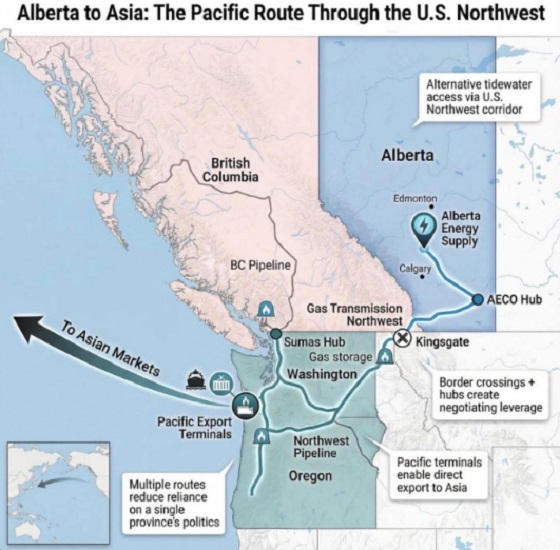
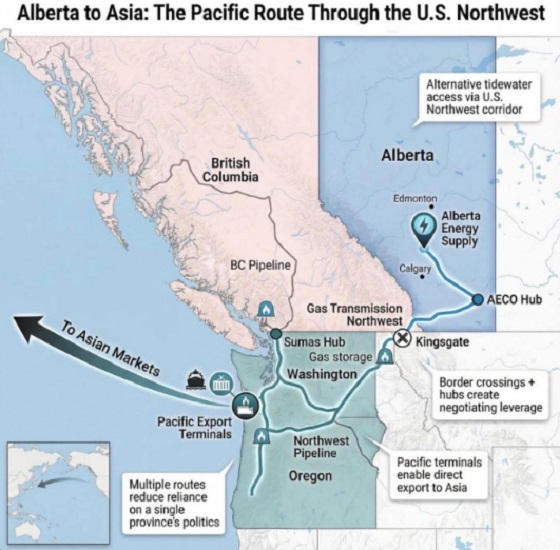 Alberta10 hours ago
Alberta10 hours agoWhat are the odds of a pipeline through the American Pacific Northwest




