Fraser Institute
Premier Eby seeks to suspend democracy in B.C.

From the Fraser Institute
By Niels Veldhuis and Tegan Hill
Last week, B.C. Premier David Eby proposed new legislation to give himself and his cabinet sweeping powers to unilaterally change almost any provincial law and regulation without legislative approval or review. While the legislation—dubbed the Economic Stabilization (Tariff Response) Act—has yet to be enacted into law, the fact that the government proposed such unprecedented powers is deeply concerning and a genuine threat to our democracy.
Only five months ago, British Columbians went to the polls and delivered a sobering victory to Eby’s incumbent NDP government, which lost 8 of its 55 seats and ended up with 47 of 93 seats, the narrowest “majority” possible. The popular vote was nearly dead-even between the NDP (44.86 per cent) and the upstart Conservative Party (43.28 per cent).
Even Premier Eby acknowledged the voters sent his government a message and promised to work together with other parties. “After a close and hard-fought campaign, it’s now time to come together to deliver for people,” he said. “British Columbians have asked us to work together and make life better for them.”
“Work together” in a democracy means embracing a deliberative and, at times, messy process. Thoughtful policymaking takes time. It’s a core feature of democracy. No leader has all the knowledge to act unilaterally to do what’s right. We need the legislature to weigh competing viewpoints through rigorous and transparent debate—that’s how our system works.
Yet according to the Eby government, the Economic Stabilization (Tariff Response) Act will lead to the opposite and provide “temporary authority to cabinet… to modify the application or effect of B.C. laws and regulations.” In other words, if approved, it will allow Premier Eby and his cabinet to override provincial laws, regulations, bylaws, rules, resolutions, practices, policies, standards, procedures and other measures without approval or review by the elected legislature. That’s not how our system is supposed to work.
To put it more starkly, the Eby government is telling British Columbians that 23 cabinet ministers and four ministers of state can sufficiently decide almost any matter pertaining to the government without democratic approval or input from opposition parties. It is by all measures an extraordinary circumvention of the province’s democratic institutions.
Premier Eby, of course, knows the extraordinary nature of this type of undemocratic authority. “In extraordinary times,” he told reporters last week, “we need extraordinary powers.” And he wants these extraordinary powers for the next two years.
While President Trump’s tariffs are terrible economic policy and very damaging to Canada and other countries, many governments throughout history have tried these policies. Like in the past, our politicians and policymakers must deal with tariffs and other economic challenges purposefully and deliberately within democratic constraints, which include transparent debates, reviews, re-assessments, and genuine deliberations that include opposition parties.
Instead, Premier Eby wants absolute power and control.
As British Columbians will no doubt conclude, there’s something fundamentally wrong with suspending democracy because we’re in challenging times. We often deal with significant challenges. Should our governments have suspended democracy in the wake of 9/11, the limited outbreak of SARS, the financial crisis of 2008-09 or COVID?
Finally, this dim view of democratic constraints is not new to the Eby government. Just last year, Premier Eby tried to pass one of the most significant and fundamental legislative changes in B.C. history, giving more than 200 First Nations veto power over land-use decisions in the province. Eby hoped to rush his legalisation through the legislature without full transparency or meaningful public input, and without disclosing any analysis of its economic impact. When British Columbians caught wind of his plan, there was an uproar, and before October’s election, Eby shelved the legislation (for now, at least).
Here we are again, mere months later, with Premier Eby wanting to make unprecedented changes to our democracy in response to an economic policy from another democratically elected government that, while damaging, is hardly an existential threat.
To call the Economic Stabilization (Tariff Response) Act a significant overreach would be a gross understatement. It’s an affront to our democracy.
Fraser Institute
Long waits for health care hit Canadians in their pocketbooks

From the Fraser Institute
Canadians continue to endure long wait times for health care. And while waiting for care can obviously be detrimental to your health and wellbeing, it can also hurt your pocketbook.
In 2024, the latest year of available data, the median wait—from referral by a family doctor to treatment by a specialist—was 30 weeks (including 15 weeks waiting for treatment after seeing a specialist). And last year, an estimated 1.5 million Canadians were waiting for care.
It’s no wonder Canadians are frustrated with the current state of health care.
Again, long waits for care adversely impact patients in many different ways including physical pain, psychological distress and worsened treatment outcomes as lengthy waits can make the treatment of some problems more difficult. There’s also a less-talked about consequence—the impact of health-care waits on the ability of patients to participate in day-to-day life, work and earn a living.
According to a recent study published by the Fraser Institute, wait times for non-emergency surgery cost Canadian patients $5.2 billion in lost wages in 2024. That’s about $3,300 for each of the 1.5 million patients waiting for care. Crucially, this estimate only considers time at work. After also accounting for free time outside of work, the cost increases to $15.9 billion or more than $10,200 per person.
Of course, some advocates of the health-care status quo argue that long waits for care remain a necessary trade-off to ensure all Canadians receive universal health-care coverage. But the experience of many high-income countries with universal health care shows the opposite.
Despite Canada ranking among the highest spenders (4th of 31 countries) on health care (as a percentage of its economy) among other developed countries with universal health care, we consistently rank among the bottom for the number of doctors, hospital beds, MRIs and CT scanners. Canada also has one of the worst records on access to timely health care.
So what do these other countries do differently than Canada? In short, they embrace the private sector as a partner in providing universal care.
Australia, for instance, spends less on health care (again, as a percentage of its economy) than Canada, yet the percentage of patients in Australia (33.1 per cent) who report waiting more than two months for non-emergency surgery was much higher in Canada (58.3 per cent). Unlike in Canada, Australian patients can choose to receive non-emergency surgery in either a private or public hospital. In 2021/22, 58.6 per cent of non-emergency surgeries in Australia were performed in private hospitals.
But we don’t need to look abroad for evidence that the private sector can help reduce wait times by delivering publicly-funded care. From 2010 to 2014, the Saskatchewan government, among other policies, contracted out publicly-funded surgeries to private clinics and lowered the province’s median wait time from one of the longest in the country (26.5 weeks in 2010) to one of the shortest (14.2 weeks in 2014). The initiative also reduced the average cost of procedures by 26 per cent.
Canadians are waiting longer than ever for health care, and the economic costs of these waits have never been higher. Until policymakers have the courage to enact genuine reform, based in part on more successful universal health-care systems, this status quo will continue to cost Canadian patients.
Business
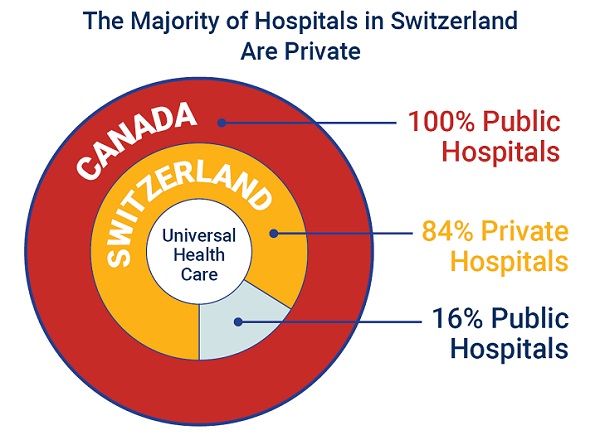
84% of Swiss hospitals and 60% of hospitalizations are in private facilities, and they face much lower wait times
From the Fraser Institute
If Canada reformed to emulate Switzerland’s approach to universal health care, including its much greater use of private sector involvement, the country would deliver far better results to patients and reduce wait times, finds a new study published today by the Fraser Institute, an independent, non-partisan Canadian policy think-tank.
“The bane of Canadian health care is lack of access to timely care, so it’s critical to look to countries like Switzerland with more successful universal health care,” said Yanick Labrie, senior fellow at the Fraser Institute and author of Integrating Private Health Care Into Canada’s Public System: What We Can Learn from Switzerland. The study highlights how Switzerland successfully integrates the private sector into their universal health-care system, which consistently outperforms Canada on most health-care metrics, including wait times.
For example, in 2022, the percentage of patients who waited less than two months for a specialist appointment was 85.3 per cent in Switzerland compared to just 48.3 per cent in Canada.
In Switzerland, 84.2 per cent of all hospitals are private (either for-profit or not-for profit) institutions, and the country’s private hospitals provide 60.2 per cent of all hospitalizations, 60.9 per cent of all births, and 67.1 per cent of all operating rooms.
Crucially, Swiss patients can obtain treatment at the hospital of their choice, whether located inside or outside their geographic location, and hospitals cannot discriminate against patients, based on the care required.
“Switzerland shows that a universal health-care system can reconcile efficiency and equity–all while being more accessible and responsive to patients’ needs and preferences,” Labrie said.
“Based on the success of the Swiss model, provinces can make these reforms now and help improve Canadian health care.”

Integrating Private Health Care into Canada’s Public System: What We Can Learn from Switzerland
- Access to timely care remains the Achilles’ heel of Canada’s health systems. To reduce wait times, some provinces have partnered with private clinics for publicly funded surgeries—a strategy that has proven effective, but continues to spark debate in Canada.
- This study explores how Switzerland successfully integrates private health care into a universal public system and considers what Canada can learn from this model.
- In Switzerland, universal coverage is delivered through a system of managed competition among 44 non-profit private insurers, while decentralized governance allows each of the 26 cantons to coordinate and oversee hospital services in ways that reflect local needs and priorities.
- Nearly two-thirds of Swiss hospitals are for-profit institutions; they provide roughly half of all hospitalizations, births, and hospital beds across the country.
- All hospitals are treated equally—regardless of legal status—and funded through the same activity-based model, implemented nationwide in 2012.
- The reform led to a significant increase in the number of cases treated without a corresponding rise in expenditures per case, suggesting improved efficiency, better use of resources, and expanded access to hospital care.
- The average length of hospital stay steadily decreased over time and now stands at 4.87 days in for-profit hospitals versus 5.53 days in public ones, indicating faster patient turnover and more streamlined care pathways.
- Hospital-acquired infection rates are significantly lower in private hospitals (2.7%) than in public hospitals (6.2%), a key indicator of care quality.
- Case-mix severity is as high or higher in private hospitals, countering the notion that they only take on simpler or less risky cases.
- Patient satisfaction is slightly higher in private hospitals (4.28/5) than in public ones (4.17/5), reflecting strong user experience across multiple dimensions.
- Canada could benefit from regulated competition between public and private providers and activity-based funding, without breaching the Canada Health Act.

-

 Alberta2 days ago
Alberta2 days agoAlberta’s grand bargain with Canada includes a new pipeline to Prince Rupert
-

 Bruce Dowbiggin1 day ago
Bruce Dowbiggin1 day agoWOKE NBA Stars Seems Natural For CDN Advertisers. Why Won’t They Bite?
-

 Business2 days ago
Business2 days agoCarney’s European pivot could quietly reshape Canada’s sovereignty
-

 Health1 day ago
Health1 day agoLast day and last chance to win this dream home! Support the 2025 Red Deer Hospital Lottery before midnight!
-

 Crime16 hours ago
Crime16 hours agoUK finally admits clear evidence linking Pakistanis and child grooming gangs
-

 Business20 hours ago
Business20 hours agoCarney praises Trump’s world ‘leadership’ at G7 meeting in Canada
-

 Energy1 day ago
Energy1 day agoCould the G7 Summit in Alberta be a historic moment for Canadian energy?
-

 Crime1 day ago
Crime1 day agoMinnesota shooter arrested after 48-hour manhunt