Fraser Institute
Opposition says Premier Eby using tariff fight to give B.C. cabinet ‘unlimited power’

From the Fraser Institute
By Bruce Pardy
It’s been 800 years since the Magna Carta. Governments everywhere now aspire to tear down the concept that it helped establish: the rule of law. Last week, British Columbia’s NDP government introduced the Economic Stabilization (Tariff Response) Act, also known as Bill 7, which would allow Premier David Eby and his cabinet the power to take the law into their own hands without going through the elected legislature.
In this case, the justification is President Donald Trump’s tariffs. But the bill would authorize any action taken for the vague purpose of supporting the economy of B.C. or Canada, or responding to the actions of any foreign government, even if the actions haven’t happened yet. But according to Eby, “These are not sweeping powers.”
The project of concentrating power in the executive branch (i.e. cabinet) and usurping the role of legislators has a long pedigree. In theory, no office or officers are above the law or are empowered to make it up as they go. In practise, that theory counts for less and less. Governments, including in Canada, don’t like the rule of law.
But what, exactly, does “the rule of law” mean? Legal theorists say it’s complicated. It need not be. To see it clearly, compare it to the alternative: the rule of persons. When King Solomon decreed that a baby claimed by two women should be split in half, he had absolute power to decide what to do. When Henry VIII ordered that Anne Boleyn should lose her head, that was absolute power, too. In each case, tyrants exercised their personal rule for good or bad.
The “rule of law” is the opposite idea. No single authority has free reign to decide how the state will use its force. The rule of law limits the powers of those who govern.
It does so in part by separating powers between three branches of the state. The Supreme Court of Canada has said that the “separation of powers” is a fundamental feature of the Canadian Constitution. Legislatures legislate. The executive executes. Judges adjudicate. In principle, no single office or officer can alone decide what should be done.
But not in practise. Exceptions are so common today as to be ubiquitous. The Human Rights Commission, not the legislature, declares what constitutes discrimination. The police decide whether to enforce court orders. Environment ministry officials determine when environmental impacts are permissible. Cabinet decides when pipelines will be built.
But in these cases, decision-makers at least must keep themselves within the boundaries of their authorizing statute, which was passed by elected legislatures. Under Bill 7, the Eby government will take delegation to the next level. Its cabinet will have the power not just to exercise broad discretion in accordance with legislation, but to override legislation itself. The bill will allow cabinet to make exceptions to the law, modify the law’s requirements, limit the law’s application, or establish powers or duties in place of the law. And not just a specific law, but any enactment on the books. The cabinet’s edicts will be valid for more than two years, until May 2027.
In 1539, the Statute of Proclamations conferred on King Henry VIII the power to rule by decree, directing that the King’s proclamations should be obeyed as though they were legislation. Such provisions, since known as “Henry VIII clauses,” are controversial because they eviscerate limits on executive power. Yet they may be constitutionally permissible in Canada. Parliament cannot abdicate its functions, the Supreme Court of Canada wrote in 1918, in a case considering the government’s conscription orders under the broad powers of the War Measures Act of 1914. But Parliament can pass legislation that delegates its powers to the executive as it sees fit. As long as the legislature retains the power to reverse the delegation, the theory goes, then separation of powers remains intact.
The rule of law is inconvenient. It gets in the way of governments and officials crafting solutions to problems they perceive as important. That’s not its downside but its purpose. Even when government efforts are well-intentioned, the power of officials to solve problems can pose a more serious threat to citizens than the problem itself. As the late Alan Borovoy, former general counsel of the Canadian Civil Liberties Association, once put it, “The source of the most insidious peril is not evil wrongdoers seeking to do harm, but parochial bureaucrats seeking to do good.” If the modern administrative state is incompatible with the rule of law, then the state should be required to adapt. For decades, the current has flowed strongly in the other direction.
Crises are an ideal time for the state to advance into territory from which it will not wish to retreat. COVID-19 was the previous excuse. Now the threat of American tariffs is the latest justification to declare an emergency and discard the limitations of the rule of law. Even impending calamity does not justify the tyranny of unfettered discretion. Boundless authority to respond to circumstances is an unbearable licence to dictate.
This commentary is based on previous commentaries.
Fraser Institute
Long waits for health care hit Canadians in their pocketbooks

From the Fraser Institute
Canadians continue to endure long wait times for health care. And while waiting for care can obviously be detrimental to your health and wellbeing, it can also hurt your pocketbook.
In 2024, the latest year of available data, the median wait—from referral by a family doctor to treatment by a specialist—was 30 weeks (including 15 weeks waiting for treatment after seeing a specialist). And last year, an estimated 1.5 million Canadians were waiting for care.
It’s no wonder Canadians are frustrated with the current state of health care.
Again, long waits for care adversely impact patients in many different ways including physical pain, psychological distress and worsened treatment outcomes as lengthy waits can make the treatment of some problems more difficult. There’s also a less-talked about consequence—the impact of health-care waits on the ability of patients to participate in day-to-day life, work and earn a living.
According to a recent study published by the Fraser Institute, wait times for non-emergency surgery cost Canadian patients $5.2 billion in lost wages in 2024. That’s about $3,300 for each of the 1.5 million patients waiting for care. Crucially, this estimate only considers time at work. After also accounting for free time outside of work, the cost increases to $15.9 billion or more than $10,200 per person.
Of course, some advocates of the health-care status quo argue that long waits for care remain a necessary trade-off to ensure all Canadians receive universal health-care coverage. But the experience of many high-income countries with universal health care shows the opposite.
Despite Canada ranking among the highest spenders (4th of 31 countries) on health care (as a percentage of its economy) among other developed countries with universal health care, we consistently rank among the bottom for the number of doctors, hospital beds, MRIs and CT scanners. Canada also has one of the worst records on access to timely health care.
So what do these other countries do differently than Canada? In short, they embrace the private sector as a partner in providing universal care.
Australia, for instance, spends less on health care (again, as a percentage of its economy) than Canada, yet the percentage of patients in Australia (33.1 per cent) who report waiting more than two months for non-emergency surgery was much higher in Canada (58.3 per cent). Unlike in Canada, Australian patients can choose to receive non-emergency surgery in either a private or public hospital. In 2021/22, 58.6 per cent of non-emergency surgeries in Australia were performed in private hospitals.
But we don’t need to look abroad for evidence that the private sector can help reduce wait times by delivering publicly-funded care. From 2010 to 2014, the Saskatchewan government, among other policies, contracted out publicly-funded surgeries to private clinics and lowered the province’s median wait time from one of the longest in the country (26.5 weeks in 2010) to one of the shortest (14.2 weeks in 2014). The initiative also reduced the average cost of procedures by 26 per cent.
Canadians are waiting longer than ever for health care, and the economic costs of these waits have never been higher. Until policymakers have the courage to enact genuine reform, based in part on more successful universal health-care systems, this status quo will continue to cost Canadian patients.
Business
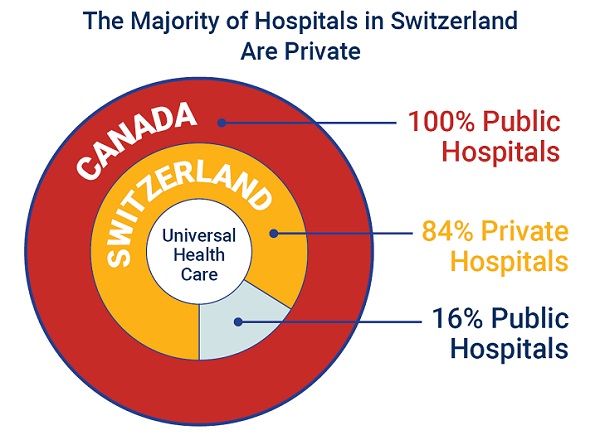
84% of Swiss hospitals and 60% of hospitalizations are in private facilities, and they face much lower wait times
From the Fraser Institute
If Canada reformed to emulate Switzerland’s approach to universal health care, including its much greater use of private sector involvement, the country would deliver far better results to patients and reduce wait times, finds a new study published today by the Fraser Institute, an independent, non-partisan Canadian policy think-tank.
“The bane of Canadian health care is lack of access to timely care, so it’s critical to look to countries like Switzerland with more successful universal health care,” said Yanick Labrie, senior fellow at the Fraser Institute and author of Integrating Private Health Care Into Canada’s Public System: What We Can Learn from Switzerland. The study highlights how Switzerland successfully integrates the private sector into their universal health-care system, which consistently outperforms Canada on most health-care metrics, including wait times.
For example, in 2022, the percentage of patients who waited less than two months for a specialist appointment was 85.3 per cent in Switzerland compared to just 48.3 per cent in Canada.
In Switzerland, 84.2 per cent of all hospitals are private (either for-profit or not-for profit) institutions, and the country’s private hospitals provide 60.2 per cent of all hospitalizations, 60.9 per cent of all births, and 67.1 per cent of all operating rooms.
Crucially, Swiss patients can obtain treatment at the hospital of their choice, whether located inside or outside their geographic location, and hospitals cannot discriminate against patients, based on the care required.
“Switzerland shows that a universal health-care system can reconcile efficiency and equity–all while being more accessible and responsive to patients’ needs and preferences,” Labrie said.
“Based on the success of the Swiss model, provinces can make these reforms now and help improve Canadian health care.”

Integrating Private Health Care into Canada’s Public System: What We Can Learn from Switzerland
- Access to timely care remains the Achilles’ heel of Canada’s health systems. To reduce wait times, some provinces have partnered with private clinics for publicly funded surgeries—a strategy that has proven effective, but continues to spark debate in Canada.
- This study explores how Switzerland successfully integrates private health care into a universal public system and considers what Canada can learn from this model.
- In Switzerland, universal coverage is delivered through a system of managed competition among 44 non-profit private insurers, while decentralized governance allows each of the 26 cantons to coordinate and oversee hospital services in ways that reflect local needs and priorities.
- Nearly two-thirds of Swiss hospitals are for-profit institutions; they provide roughly half of all hospitalizations, births, and hospital beds across the country.
- All hospitals are treated equally—regardless of legal status—and funded through the same activity-based model, implemented nationwide in 2012.
- The reform led to a significant increase in the number of cases treated without a corresponding rise in expenditures per case, suggesting improved efficiency, better use of resources, and expanded access to hospital care.
- The average length of hospital stay steadily decreased over time and now stands at 4.87 days in for-profit hospitals versus 5.53 days in public ones, indicating faster patient turnover and more streamlined care pathways.
- Hospital-acquired infection rates are significantly lower in private hospitals (2.7%) than in public hospitals (6.2%), a key indicator of care quality.
- Case-mix severity is as high or higher in private hospitals, countering the notion that they only take on simpler or less risky cases.
- Patient satisfaction is slightly higher in private hospitals (4.28/5) than in public ones (4.17/5), reflecting strong user experience across multiple dimensions.
- Canada could benefit from regulated competition between public and private providers and activity-based funding, without breaching the Canada Health Act.

-

 conflict2 days ago
conflict2 days agoOne dead, over 60 injured after Iranian missiles pierce Iron Dome
-

 Crime11 hours ago
Crime11 hours agoManhunt on for suspect in shooting deaths of Minnesota House speaker, husband
-

 Business38 mins ago
Business38 mins agoCarney’s European pivot could quietly reshape Canada’s sovereignty
-

 Alberta16 mins ago
Alberta16 mins agoAlberta’s grand bargain with Canada includes a new pipeline to Prince Rupert