Health
Opening independent non-profit hospitals would improve access to care and efficiency in Canada’s healthcare system

From the Montreal Economic Institute
Autonomous non-profit hospitals tend to perform better than government-run hospitals, shows a study published this morning by the Montreal Economic Institute.
“Interminable waits in Canadian hospitals show that our healthcare systems are struggling to deliver basic services to the population,” says Emmanuelle B. Faubert, economist at MEI and author of the study. “By allowing independent non-profit hospitals to open, our governments would help increase treatment capacity, to the benefit of patients.”
In 2023, the median wait time in Quebec ERs was 5 hours and 13 minutes, up 42 minutes from five years earlier.
It is estimated that as a result of chronic overcrowding in Canadian ERs, there are between 8,000 and 15,000 avoidable deaths each year.
The Canadian health care system ranks 10th out of 11 comparable industrialized countries, just ahead of the United States, in the Commonwealth Fund’s ranking of healthcare systems. The French, German, and Dutch systems are 8th, 5th, and 2nd respectively in the same ranking.
While the Canadian system has no independent non-profit hospitals according to the OECD’s definition, such facilities account for 14 per cent of French hospital beds, 28 per cent of German hospital beds, and 100 per cent of Dutch hospital beds.
The researcher attributes a portion of the success of these facilities to their greater managerial autonomy and to a funding method that encourages the treatment of more patients.
“One of the strengths of these hospitals is how quickly they can adapt, contrary to facilities micromanaged by government ministries, as is the case in Canada,” explains Ms. Faubert. “Since their financing depends on the type and the quantity of ailments treated, administrators see the sustainability of their facilities as being directly linked to their capacity to treat patients.”
Although Canadian hospitals generally have their own boards of directors, the management of their daily activities and their funding are subject to strict government control.
Aside from certain limited experiments, notably in Quebec, Canadian hospitals still depend largely on a global budgeting model, in which funding depends entirely on the level of activity in the previous year.
Since the annual budgetary envelope is fixed, each additional patient is seen as a cost, says the researcher.
In Europe, in contrast, hospitals are largely financed according to an activity-based funding model, whereby a hospital receives a set amount of money for each treatment carried out within its walls. With this system, each additional patient treated represents an immediate source of revenue for the facility, says the researcher.
“It’s clear that our healthcare system can and must do better, and that means changing the incentives of those who manage it,” says Ms. Faubert. “By introducing non-profit hospitals, with a better funding model, and by granting health professionals more flexibility, we will be able to provide better care to more patients, as they do in Europe.”
The MEI study is available here.
* * *
The MEI is an independent public policy think tank with offices in Montreal and Calgary. Through its publications, media appearances, and advisory services to policymakers, the MEI stimulates public policy debate and reforms based on sound economics and entrepreneurship.
Business
RFK Jr. says Hep B vaccine is linked to 1,135% higher autism rate

From LifeSiteNews
By Matt Lamb
They got rid of all the older children essentially and just had younger children who were too young to be diagnosed and they stratified that, stratified the data
The Centers for Disease Control and Prevention (CDC) found newborn babies who received the Hepatitis B vaccine had 1,135-percent higher autism rates than those who did not or received it later in life, Robert F. Kennedy Jr. told Tucker Carlson recently. However, the CDC practiced “trickery” in its studies on autism so as not to implicate vaccines, Kennedy said.
RFK Jr., who is the current Secretary of Health and Human Services, said the CDC buried the results by manipulating the data. Kennedy has pledged to find the causes of autism, with a particular focus on the role vaccines may play in the rise in rates in the past decades.
The Hepatitis B shot is required by nearly every state in the U.S. for children to attend school, day care, or both. The CDC recommends the jab for all babies at birth, regardless of whether their mother has Hep B, which is easily diagnosable and commonly spread through sexual activity, piercings, and tattoos.
“They kept the study secret and then they manipulated it through five different iterations to try to bury the link and we know how they did it – they got rid of all the older children essentially and just had younger children who were too young to be diagnosed and they stratified that, stratified the data,” Kennedy told Carlson for an episode of the commentator’s podcast. “And they did a lot of other tricks and all of those studies were the subject of those kind of that kind of trickery.”
But now, Kennedy said, the CDC will be conducting real and honest scientific research that follows the highest standards of evidence.
“We’re going to do real science,” Kennedy said. “We’re going to make the databases public for the first time.”
He said the CDC will be compiling records from variety of sources to allow researchers to do better studies on vaccines.
“We’re going to make this data available for independent scientists so everybody can look at it,” the HHS secretary said.
— Matt Lamb (@MattLamb22) July 1, 2025
Health and Human Services also said it has put out grant requests for scientists who want to study the issue further.
Kennedy reiterated that by September there will be some initial insights and further information will come within the next six months.
Carlson asked if the answers would “differ from status quo kind of thinking.”
“I think they will,” Kennedy said. He continued on to say that people “need to stop trusting the experts.”
“We were told at the beginning of COVID ‘don’t look at any data yourself, don’t do any investigation yourself, just trust the experts,”‘ he said.
In a democracy, Kennedy said, we have the “obligation” to “do our own research.”
“That’s the way it should be done,” Kennedy said.
He also reiterated that HHS will return to “gold standard science” and publish the results so everyone can review them.
International
RFK Jr. tells Tucker how Big Pharma uses ‘perverse incentives’ to get vaccines approved
From LifeSiteNews
By Matt Lamb
Kennedy defended his decision to fire all 17 members of the Advisory Committee on Immunization Practices, which he decried as a tool used to “rubber stamp” vaccines.
The vaccine approval process is a “bundle of perverse incentives” since pharmaceutical companies stand to make billions of dollars in revenue from it, Secretary of Health and Human Services Robert F. Kennedy Jr. told Tucker Carlson recently.
Kennedy appeared on Carlson’s show yesterday to discuss a variety of issues, including the potential link between autism and vaccines and his overhauling of the vaccine advisory committee at the Centers for Disease Control and Prevention last month.
Twenty years ago, Bobby Kennedy was exiled from polite society for suggesting a link between autism and vaccines. Now he’s a cabinet secretary, and still saying it.
(0:00) The Organized Opposition to RFK’s Mission
(6:46) Uncovering the Reason for Skyrocketing Rates of Autism… pic.twitter.com/g8T8te3kNC— Tucker Carlson (@TuckerCarlson) June 30, 2025
Kennedy began by explaining that Big Pharma has been targeting academic journals to ensure its products receive favorable reviews.
“The journals won’t publish anything critical of vaccines … there’s so much pressure on them. They’re funded by pharmaceutical companies, and they’ll lose advertising and revenue from reprints,” Kennedy said.
Kennedy then noted that Big Pharma will “pay to get something published in these journals,” before accusing industry leaders of pushing drugs on doctors and of hiring “mercenary scientists” to manipulate data until their product is deemed safe and effective.
The entire complex is broken due to the “perverse incentives,” he lamented.
Later in the interview, Kennedy defended his decision to fire all 17 members of the Advisory Committee on Immunization Practices (ACIP) in June, which he decried as a mere tool to “rubber stamp” vaccines.
It served as “a sock puppet for the industry that it was supposed to regulate,” Kennedy exclaimed, citing conflicts of interest for the overwhelming majority of its board members.
This sort of “agency capture” explains the lucrative nature of vaccines, he added.
— Matt Lamb (@MattLamb22) July 1, 2025
Kennedy then summarized the “perverse” process as follows:
First of all, the federal government often times actually designs the vaccine, [the National Institutes of Health] would design it, would hand it over to the pharmaceutical company. The pharmaceutical company then runs it … first through [the] FDA, then through [the] ACIP, and gets it recommended.
If you can get that recommendation you now got a billion dollars in — at least — revenues by the end of the year, every year, forever. So, there was a gold rush to add new vaccines to the schedule and ACIP never turned away a single vaccine … that came to them they recommended, and a lot of these vaccines are for diseases that are not even casually contagious.
Kennedy further pointed to the Hepatitis B shot for newborns as an example of how the industry has been corrupted.
In 1999, the CDC “looked at children who had received the hepatitis vaccine within the first 30 days of life and compared those children to children who had received the vaccine later — or not at all. And they found an 1,135% elevated risk of autism among the vaccinated children. It shocked them. They kept the study secret and manipulated it through five different iterations to try to bury the link,” he said.
“We want to protect public health,” Kennedy explained, but “these vaccines … can cause chronic disease, chronic injuries that last a lifetime.”
-

 Business6 hours ago
Business6 hours agoRFK Jr. says Hep B vaccine is linked to 1,135% higher autism rate
-

 Alberta1 day ago
Alberta1 day agoAlberta Independence Seekers Take First Step: Citizen Initiative Application Approved, Notice of Initiative Petition Issued
-
 Crime19 hours ago
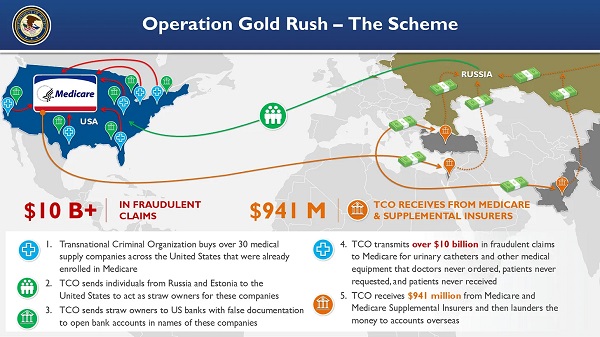
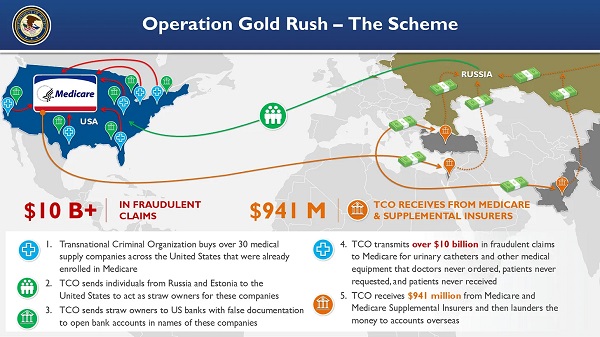
Crime19 hours agoNational Health Care Fraud Takedown Results in 324 Defendants Charged in Connection with Over $14.6 Billion in Alleged Fraud
-

 Crime1 day ago
Crime1 day agoSuspected ambush leaves two firefighters dead in Idaho
-

 Health18 hours ago
Health18 hours agoRFK Jr. Unloads Disturbing Vaccine Secrets on Tucker—And Surprises Everyone on Trump
-

 Alberta1 day ago
Alberta1 day agoWhy the West’s separatists could be just as big a threat as Quebec’s
-

 Business1 day ago
Business1 day agoCanada Caves: Carney ditches digital services tax after criticism from Trump
-

 Business1 day ago
Business1 day agoMassive government child-care plan wreaking havoc across Ontario