Health
Medical Groupthink Makes People Sicker, Analysts Argue

From Heartland Daily News
Medicine has a huge “blind spot” that has led to an explosion of childhood obesity, diabetes, autism, peanut allergies, and autoimmune diseases in the United States, says Martin Makary, M.D., author of the bestselling book Blind Spots.
“We have the sickest population in the history of the world … right here in the United States, despite spending double what other wealthy countries spend on health care,” said Makary during a September 20 presentation at the Cato Institute, titled “Blind Spots: When Medicine Gets It Wrong, and What It Means for Our Health.” Also on the panel were Cato scholars Jeffrey A. Singer, M.D., and David A. Hyman, M.D.
Makary became well-known during the COVID-19 lockdowns as one of a small group of prominent physicians who publicly questioned the government’s response to the virus. Makary is a professor of surgery at Johns Hopkins Medicine, where he researches the underlying causes of disease and has written numerous scientific articles and two other bestselling books.
Chronic-Disease Epidemics
Makary said the rates of some diseases have reached epidemic proportions. Half of all children in the United States are obese or overweight, with 20 percent now diabetic or prediabetic. The rate of children being diagnosed with autism is up 14 percent every year for the last 23 years, one in five U.S. women have been diagnosed with an autoimmune disease, and gastrointestinal cancers have doubled in the last two decades.
“We have got to ask the big questions,” said Makary said in his remarks. “We have developed blind spots not because we’re bad people but because the system has a groupthink, a herd mentality.”
Health care has become assembly-line medicine, with health professionals pressured to focus more on productivity and billing output than on improving overall health, says Makary.
“We need to look at gut health, the microbiome, our poisoned food supply; maybe we need to look at environmental exposures that cause cancer, not just the chemo to treat it; maybe treat diabetes with cooking classes instead of throwing meds at people; maybe we need to treat high blood pressure by talking about sleep quality,” said Makary.
Sticky Theories
Hyman says cognitive dissonance can cause blind spots, highlighting an example of a surgeon initially resistant to trying less-invasive antibiotics before surgically removing an appendix, as recounted in Makary’s book.
“Easy problems are already fixed, so how do we fix this hard problem?” said Hyman at the presentation, pointing out unjustified medical opinions can persist for decades.
Such opinions include the ideas that “opioids are not addictive, or antibiotics won’t hurt you, or hormone therapy causes breast cancer even though the data never supported it, the dogma of the food pyramid,” said Makary.
“We love to hold on to old ideas not because they’re better or more logical or [more] scientifically supported than new information, but just because we heard it first,” said Makary. “And it gets comfortable. It will nest in the brain, and subconsciously we will defend it.”
Peanut Allergy Mixup
Singer asked Makary about the peanut allergy dogma the American Academy of Pediatrics pushed in 2000, recommending children not eat peanuts before the age of three. It turned out to be wrong, said Singer.
“We have peanut allergies in the U.S. at epidemic proportions, [yet] they don’t have them in Africa and parts of Europe and Asia,” said Makary. The United States “got it perfectly backward,” said Makary. “Peanut abstinence results in a sensitization at the immune-system level.”
An early introduction of peanuts reduces the incidence of people identified with peanut allergies at a rate of 86 percent, Makary told the audience.
Makary said he confronted those who argued for peanut abstinence, noting there were no studies to back up the recommendation. They replied that they felt compelled to weigh in because the public wanted something done, said Makary.
‘Demonized’ HRT
The recommendation against hormone replacement therapy (HRT) for older women because of breast cancer risk is another example of misguided groupthink, Makary told the audience.
“It is probably the biggest screw-up in modern medicine,” said Makary.
“HRT replaces estrogen when the body stops producing it,” said Makary. “Women who start it within 10 years after the onset of menopause live on average three and a half years longer, have healthier blood vessels, they will have 50 to 60 percent less cognitive decline, the risk of Alzheimer’s goes down by 35 percent. Women feel better and live longer. The rate of heart attacks goes down by half. And their bones are stronger. There is probably no medication that has a greater impact on health outcomes in populations than hormone therapy.”
A demonization campaign against HRT began 22 years ago when a single scientist at the National Institutes of Health held a press conference saying HRT was linked to breast cancer, Makary told the audience.
“The incredible back story is that no data were released at that announcement,” said Makary. “And today there is no statistically significant increase [of breast cancer].”
Political Challenges
Among the broad range of topics in the 75-minute discussion, the panelists considered how medical groupthink affects government policy.
“Agencies make decisions in the shadows of how [they think] Congress will react,” said Hyman. “Congress can make your life really miserable if you’re a federal regulator. They can cut your budget, call you in, and yell at you because you haven’t taken aggressive steps to protect the American public.”
Makary said doctors must avoid making recommendations based on “gut feelings.”
“We spend a staggering amount of money on delivering health care, and very little money on what actually works,” said Hyman.
AnneMarie Schieber ([email protected]) is the managing editor of Health Care News.
COVID-19
FDA requires new warning on mRNA COVID shots due to heart damage in young men

From LifeSiteNews
Pfizer and Moderna’s mRNA COVID shots must now include warnings that they cause ‘extremely high risk’ of heart inflammation and irreversible damage in males up to age 24.
The Trump administration’s Food and Drug Administration (FDA) announced it will now require updated safety warnings on mRNA COVID-19 shots to include the “extremely high risk” of myocarditis/pericarditis and the likelihood of long-term, irreversible heart damage for teen boys and young men up to age 24.
The required safety updates apply to Comirnaty, the mRNA COVID shot manufactured by Pfizer Inc., and Spikevax, the mRNA COVID shot manufactured ModernaTX, Inc.
According to a press release, the FDA now requires each of those manufacturers to update the warning about the risks of myocarditis and pericarditis to include information about:
- the estimated unadjusted incidence of myocarditis and/or pericarditis following administration of the 2023-2024 Formula of mRNA COVID-19 shots and
- the results of a study that collected information on cardiac magnetic resonance imaging (cardiac MRI) in people who developed myocarditis after receiving an mRNA COVID-19 injection.
The FDA has also required the manufacturers to describe the new safety information in the adverse reactions section of the prescribing information and in the information for recipients and caregivers.
Additionally, the fact sheets for healthcare providers and for recipients and caregivers for Moderna COVID-19 shot and Pfizer-BioNTech COVID-19 shot, which are authorized for emergency use in individuals 6 months through 11 years of age, have also been updated to include the new safety information in alignment with the Comirnaty and Spikevax prescribing information and information for recipients and caregivers.
In a video published on social media, Dr. Vinay Prasad, director of the Center for Biologics Evaluation & Research Chief Medical and Scientific Officer, explained the alarming reasons for the warning updates.
While heart problems arose in approximately 8 out of 1 million persons ages 6 months to 64 years following reception of the cited shots, that number more than triples to 27 per million for males ages 12 to 24.
Prasad noted that multiple studies have arrived at similar findings.
Business
National dental program likely more costly than advertised

From the Fraser Institute
By Matthew Lau
At the beginning of June, the Canadian Dental Care Plan expanded to include all eligible adults. To be eligible, you must: not have access to dental insurance, have filed your 2024 tax return in Canada, have an adjusted family net income under $90,000, and be a Canadian resident for tax purposes.
As a result, millions more Canadians will be able to access certain dental services at reduced—or no—out-of-pocket costs, as government shoves the costs onto the backs of taxpayers. The first half of the proposition, accessing services at reduced or no out-of-pocket costs, is always popular; the second half, paying higher taxes, is less so.
A Leger poll conducted in 2022 found 72 per cent of Canadians supported a national dental program for Canadians with family incomes up to $90,000—but when asked whether they would support the program if it’s paid for by an increase in the sales tax, support fell to 42 per cent. The taxpayer burden is considerable; when first announced two years ago, the estimated price tag was $13 billion over five years, and then $4.4 billion ongoing.
Already, there are signs the final cost to taxpayers will far exceed these estimates. Dr. Maneesh Jain, the immediate past-president of the Ontario Dental Association, has pointed out that according to Health Canada the average patient saved more than $850 in out-of-pocket costs in the program’s first year. However, the Trudeau government’s initial projections in the 2023 federal budget amounted to $280 per eligible Canadian per year.
Not all eligible Canadians will necessarily access dental services every year, but the massive gap between $850 and $280 suggests the initial price tag may well have understated taxpayer costs—a habit of the federal government, which over the past decade has routinely spent above its initial projections and consistently revises its spending estimates higher with each fiscal update.
To make matters worse there are also significant administrative costs. According to a story in Canadian Affairs, “Dental associations across Canada are flagging concerns with the plan’s structure and sustainability. They say the Canadian Dental Care Plan imposes significant administrative burdens on dentists, and that the majority of eligible patients are being denied care for complex dental treatments.”
Determining eligibility and coverage is a huge burden. Canadians must first apply through the government portal, then wait weeks for Sun Life (the insurer selected by the federal government) to confirm their eligibility and coverage. Unless dentists refuse to provide treatment until they have that confirmation, they or their staff must sometimes chase down patients after the fact for any co-pay or fees not covered.
Moreover, family income determines coverage eligibility, but even if patients are enrolled in the government program, dentists may not be able to access this information quickly. This leaves dentists in what Dr. Hans Herchen, president of the Alberta Dental Association, describes as the “very awkward spot” of having to verify their patients’ family income.
Dentists must also try to explain the program, which features high rejection rates, to patients. According to Dr. Anita Gartner, president of the British Columbia Dental Association, more than half of applications for complex treatment are rejected without explanation. This reduces trust in the government program.
Finally, the program creates “moral hazard” where people are encouraged to take riskier behaviour because they do not bear the full costs. For example, while we can significantly curtail tooth decay by diligent toothbrushing and flossing, people might be encouraged to neglect these activities if their dental services are paid by taxpayers instead of out-of-pocket. It’s a principle of basic economics that socializing costs will encourage people to incur higher costs than is really appropriate (see Canada’s health-care system).
At a projected ongoing cost of $4.4 billion to taxpayers, the newly expanded national dental program is already not cheap. Alas, not only may the true taxpayer cost be much higher than this initial projection, but like many other government initiatives, the dental program already seems to be more costly than initially advertised.
-

 Alberta9 hours ago
Alberta9 hours agoCOWBOY UP! Pierre Poilievre Promises to Fight for Oil and Gas, a Stronger Military and the Interests of Western Canada
-
 Alberta1 day ago
Alberta1 day agoAlberta Next: Immigration
-

 Business2 days ago
Business2 days agoThe Digital Services Tax Q&A: “It was going to be complicated and messy”
-

 International2 days ago
International2 days agoElon Musk forms America Party after split with Trump
-
 Alberta9 hours ago
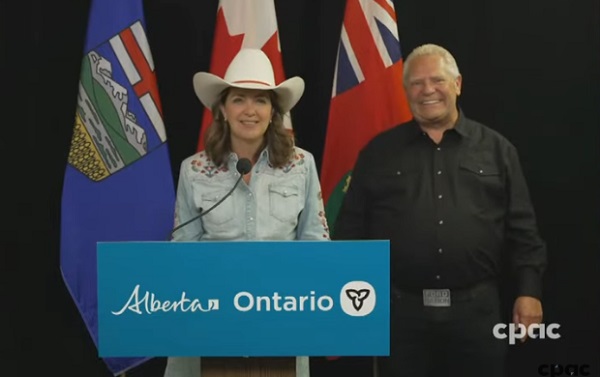
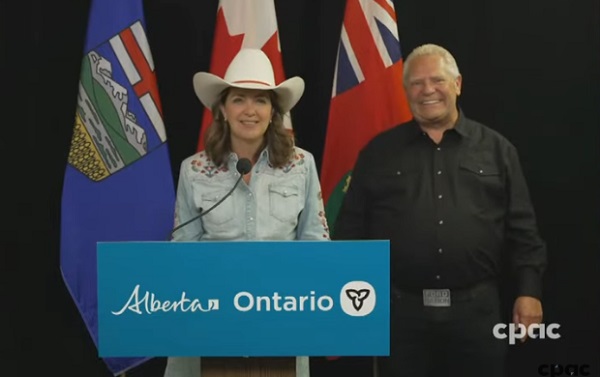
Alberta9 hours agoAlberta and Ontario sign agreements to drive oil and gas pipelines, energy corridors, and repeal investment blocking federal policies
-

 COVID-1913 hours ago
COVID-1913 hours agoFDA requires new warning on mRNA COVID shots due to heart damage in young men
-

 Alberta Sports Hall of Fame and Museum24 hours ago
Alberta Sports Hall of Fame and Museum24 hours agoAlberta Sports Hall of Fame 2025 Inductee Profiles – Para Nordic Skiing – Brian and Robin McKeever
-

 Crime10 hours ago
Crime10 hours agoEyebrows Raise as Karoline Leavitt Answers Tough Questions About Epstein