Health
LGBT group challenges Alberta pro-family bill, wants puberty blockers for 10-year-olds
From LifeSiteNews
A federally funded pro-LGBT group is challenging Alberta’s pro-family legislation that bans giving often sterilizing puberty blockers to kids, claiming sex “reassignment” procedures are necessary for children.
On December 9, Egale Canada, an LGBT activist group, filed an injunction against Alberta’s newly passed Health Statutes Amendment Act (HSAA), also called Bill 26, at the Calgary’s Court of King’s Bench
“If you deny a kid access to blockers and then they go through permanent changes via puberty, they then have to pursue medical treatment and interventions to undo the effects of [puberty], so that is how the coercion is operating,” Bennett Jensen, legal director at Egale Canada, told CBC News.
Alberta’s new legislation, passed last week, reflects “the government’s commitment to build a health care system that responds to the changing needs of Albertans,” it said.
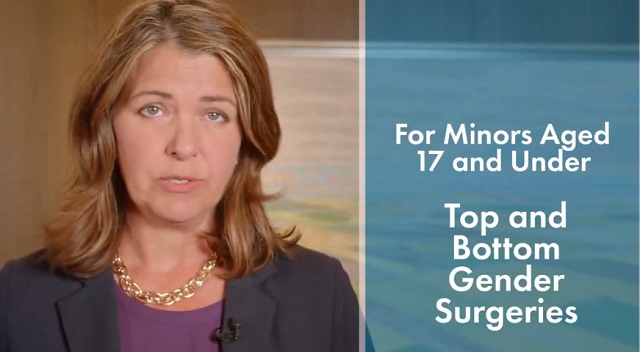
The bill will amend the Health Act to “prohibit regulated health professionals from performing sex reassignment surgeries on minors.”
It will also ban the “use of puberty blockers and hormone therapies for the treatment of gender dysphoria or gender incongruence” to kids 15 and under “except for those who have already commenced treatment and would allow for minors aged 16 and 17 to choose to commence puberty blockers and hormone therapies for gender reassignment and affirmation purposes with parental, physician and psychologist approval.”
Egale Canada, which receives funding from Prime Minister Justin Trudeau’s federal government, has paired with Skipping Stone and five Alberta families to challenge the new law. The group is using five gender-confused children to argue their case.
They claim that the new legislation violates both the national Charter of Rights and Freedoms and the provincial Alberta Bill of Rights.
The court filing effectively argues that if the Alberta bill is upheld, the gender-confused children, some as young as ten, will not be able to halt naturally occurring puberty through artificial means, which presents an impediment to their ability to “transition.”
While some are objecting to the common-sense legislation, the Alberta bill has found the support of an alliance for detransitioners who regret their “gender transition” process.
Despite the claims of LGBT activists, there is overwhelming evidence showing that people who undergo so-called “gender transitioning” are more likely to commit suicide than those who are not given irreversible surgery.
Transgender surgeries and drugs have been linked to permanent physical and psychological damage, including cardiovascular diseases, loss of bone density, cancer, strokes and blood clots, and infertility.
Meanwhile, a recent study on the side effects of transgender “sex change” surgeries discovered that 81 percent of those who had undergone “sex change” surgeries in the past five years reported experiencing pain simply from normal movement in the weeks and months that followed – and that many other side effects manifest as well.
Health
FDA warns ‘breast binder’ manufacturers to stop marketing to gender-confused girls

From LifeSiteNews
Dr. Marty Makary took aim at the transgender-medical-industrial complex that has exploded in recent years during a recent press conference.
Food and Drug Administration (FDA) commissioner Dr. Marty Makary has sternly warned companies manufacturing “breast binders” to cease marketing and supplying their product to gender-confused girls seeking to make their bodies appear masculine.
“Today the FDA is taking action,” said Makary in a press conference. “We are sending warning letters to 12 manufacturers and retailers for illegal marketing of breast binders for children, for the purposes of treating gender dysphoria.”
“Breast binders are a class one medical device with legitimate medical users, such as being used by women after breast cancer surgery,” but “these binders are not benign,” he cautioned. “Long-term usage has been associated with pain, compromised lung function, and even difficulty breast feeding later in life.”
“The warning letters will formally notify the companies of their significant regulatory violations and require prompt corrective action,” said the FDA head.
.@DrMakaryFDA: “Today the FDA is taking action. We are sending warning letters to 12 manufacturers and retailers for illegal marketing of breast binders for children, for the purposes of treating gender dysphoria.” pic.twitter.com/6JNAy36223
— HHS Rapid Response (@HHSResponse) December 18, 2025
The warning letter addressed to California manufacturer, GenderBender, notes that the company’s website states that “[c]hest binding is the practice of compressing breast mass into a more masculine shape, often done in the LGBTQ community for gender euphoria.”
“Your firm should take prompt action to address any violations identified in this letter. Failure to adequately address this matter may result in regulatory action being initiated by the FDA without further notice. These actions include, but are not limited to, seizure and injunction,” advised the FDA.
During his presentation, Makary took aim at the transgender-medical-industrial complex that has exploded in recent years.
“One of the most barbaric features of a society is the genital mutilation of its children,” observed Makary.
“Pushing transgender ideology in children is predatory, it’s wrong, and it needs to stop,” he declared.
“This ideology is a belief system that some teachers, some pediatricians, and others are selling to children without their parents knowing sometimes, or with a deliberate attempt to remove parents from the decision making,” Makary explained.
To witness society “putting kids on a path of chest binders, drugs, castration, mastectomies, and other procedures is a path that now many kids regret,” he lamented, as he pointed to Chloe Cole, who has reverted to her God-given femininity after undergoing so-called “gender-affirming” surgery as a teen.
Cole is a leading voice for young people who have “detransitioned” after having medically, surgically, and socially attempted to “transition” to a member of the opposite sex.
.@DrMakaryFDA: “Pushing transgender ideology in children is predatory, it's wrong, and it needs to stop.” pic.twitter.com/TXxWNEtNZk
— HHS Rapid Response (@HHSResponse) December 18, 2025
Health
All 12 Vaccinated vs. Unvaccinated Studies Found the Same Thing: Unvaccinated Children Are Far Healthier

I joined Del Bigtree in studio on The HighWire to discuss what the data now make unavoidable: the CDC’s 81-dose hyper-vaccination schedule is driving the modern epidemics of chronic disease and autism.
This was not a philosophical debate or a clash of opinions. We walked through irrefutable, peer-reviewed evidence showing that whenever vaccinated and unvaccinated children are compared directly, the unvaccinated group is far healthier—every single time.
Reanalyzing the Largest Vaccinated vs. Unvaccinated Birth-Cohort Study Ever Conducted
At the center of our discussion was our peer-reviewed reanalysis of the Henry Ford Health System vaccinated vs. unvaccinated birth-cohort study (Lamerato et al.)—the largest and most rigorous comparison of its kind ever conducted.
|
The original authors relied heavily on Cox proportional hazards models, a time-adjusted approach that can soften absolute disease burden. Even so, nearly all chronic disease outcomes were higher in vaccinated children.
Our reanalysis used direct proportional comparisons, stripping away the smoothing and revealing the full magnitude of the signal.
- All 22 chronic disease categories favored the unvaccinated cohort when proportional disease burden was examined
- Cancer incidence was 54% higher in vaccinated children (0.0102 vs. 0.0066)
- When autism-associated conditions were grouped appropriately—including autism, ADHD, developmental delay, learning disability, speech disorder, neurologic impairment, seizures, and related diagnoses—the vaccinated cohort showed a 549% higher odds of autism-spectrum–associated clinical outcomes
The findings are internally consistent, biologically coherent, and concordant with every prior vaccinated vs. unvaccinated study, all of which show drastically poorer health outcomes among vaccinated children
The 12 Vaccinated vs. Unvaccinated Studies Regulators Ignore
In the McCullough Foundation Autism Report, we compiled all 12 vaccinated vs. unvaccinated pediatric studies currently available. These studies span different populations, countries, study designs, and data sources.
Every single one reports the same overall pattern. Across all 12 studies, unvaccinated children consistently exhibit substantially lower rates of chronic disease, including:
- Autism and other neurodevelopmental disorders
- ADHD, tics, learning and speech disorders
- Asthma, allergies, eczema, and autoimmune conditions
- Chronic ear infections, skin disorders, and gastrointestinal illness
This level of consistency across independent datasets is precisely what epidemiology looks for when assessing causality. It also explains why no federal agency has ever conducted—or endorsed—a fully vaccinated vs. fully unvaccinated safety study.
Flu Shot Failure
We also addressed the persistent failure of seasonal influenza vaccination.
A large Cleveland Clinic cohort study of 53,402 employees followed participants during the 2024–2025 respiratory viral season and found:
- 82.1% of employees were vaccinated against influenza
- Vaccinated individuals had a 27% higher adjusted risk of influenza compared with the unvaccinated state (HR 1.27; 95% CI 1.07–1.51; p = 0.007)
- This corresponded to a negative vaccine effectiveness of −26.9% (95% CI −55.0 to −6.6%), meaning vaccination was associated with increased—not reduced—risk of influenza
When vaccination exposure increases, chronic disease, neurodevelopmental disorders, and inflammatory illness increase with it. When children are unvaccinated, they are measurably healthier across virtually every outcome that matters.
The science needed to confront the chronic disease and autism epidemics already exists. What remains is the willingness to acknowledge it.
Epidemiologist and Foundation Administrator, McCullough Foundation
Support our mission: mcculloughfnd.org
Please consider following both the McCullough Foundation and my personal account on X (formerly Twitter) for further content.
FOCAL POINTS (Courageous Discourse) is a reader-supported publication.
To receive new posts and support my work, consider becoming a free or paid subscriber.
-

 Business1 day ago
Business1 day agoArgentina’s Milei delivers results free-market critics said wouldn’t work
-

 Business2 days ago
Business2 days agoState of the Canadian Economy: Number of publicly listed companies in Canada down 32.7% since 2010
-

 espionage20 hours ago
espionage20 hours agoCarney Floor Crossing Raises Counterintelligence Questions aimed at China, Former Senior Mountie Argues
-

 International2 days ago
International2 days agoDOJ fails to fully comply with Friday deadline for Epstein files release
-

 Business14 hours ago
Business14 hours agoTaxing food is like slapping a surcharge on hunger. It needs to end
-

 Bruce Dowbiggin2 days ago
Bruce Dowbiggin2 days agoHunting Poilievre Covers For Upcoming Demographic Collapse After Boomers
-

 Alberta2 days ago
Alberta2 days agoAlberta’s new diagnostic policy appears to meet standard for Canada Health Act compliance
-

 Business1 day ago
Business1 day agoDeadlocked Jury Zeroes In on Alleged US$40 Million PPE Fraud in Linda Sun PRC Influence Case








