Brownstone Institute
FDA Exposed: Hundreds of Drugs Approved without Proof They Work

From the Brownstone Institute
By
The US Food and Drug Administration (FDA) has approved hundreds of drugs without proof that they work—and in some cases, despite evidence that they cause harm.
That’s the finding of a blistering two-year investigation by medical journalists Jeanne Lenzer and Shannon Brownlee, published by The Lever.
Reviewing more than 400 drug approvals between 2013 and 2022, the authors found the agency repeatedly ignored its own scientific standards.
One expert put it bluntly—the FDA’s threshold for evidence “can’t go any lower because it’s already in the dirt.”
A System Built on Weak Evidence
The findings were damning—73% of drugs approved by the FDA during the study period failed to meet all four basic criteria for demonstrating “substantial evidence” of effectiveness.
Those four criteria—presence of a control group, replication in two well-conducted trials, blinding of participants and investigators, and the use of clinical endpoints like symptom relief or extended survival—are supposed to be the bedrock of drug evaluation.
Yet only 28% of drugs met all four criteria—40 drugs met none.
These aren’t obscure technicalities—they are the most basic safeguards to protect patients from ineffective or dangerous treatments.
But under political and industry pressure, the FDA has increasingly abandoned them in favour of speed and so-called “regulatory flexibility.”
Since the early 1990s, the agency has relied heavily on expedited pathways that fast-track drugs to market.
In theory, this balances urgency with scientific rigour. In practice, it has flipped the process. Companies can now get drugs approved before proving that they work, with the promise of follow-up trials later.
But, as Lenzer and Brownlee revealed, “Nearly half of the required follow-up studies are never completed—and those that are often fail to show the drugs work, even while they remain on the market.”
“This represents a seismic shift in FDA regulation that has been quietly accomplished with virtually no awareness by doctors or the public,” they added.
More than half the approvals examined relied on preliminary data—not solid evidence that patients lived longer, felt better, or functioned more effectively.
And even when follow-up studies are conducted, many rely on the same flawed surrogate measures rather than hard clinical outcomes.
The result: a regulatory system where the FDA no longer acts as a gatekeeper—but as a passive observer.
Cancer Drugs: High Stakes, Low Standards
Nowhere is this failure more visible than in oncology.
Only 3 out of 123 cancer drugs approved between 2013 and 2022 met all four of the FDA’s basic scientific standards.
Most—81%—were approved based on surrogate endpoints like tumour shrinkage, without any evidence that they improved survival or quality of life.
Take Copiktra, for example—a drug approved in 2018 for blood cancers. The FDA gave it the green light based on improved “progression-free survival,” a measure of how long a tumour stays stable.
But a review of post-marketing data showed that patients taking Copiktra died 11 months earlier than those on a comparator drug.
It took six years after those studies showed the drug reduced patients’ survival for the FDA to warn the public that Copiktra should not be used as a first- or second-line treatment for certain types of leukaemia and lymphoma, citing “an increased risk of treatment-related mortality.”
Elmiron: Ineffective, Dangerous—And Still on the Market
Another striking case is Elmiron, approved in 1996 for interstitial cystitis—a painful bladder condition.
The FDA authorized it based on “close to zero data,” on the condition that the company conduct a follow-up study to determine whether it actually worked.
That study wasn’t completed for 18 years—and when it was, it showed Elmiron was no better than placebo.
In the meantime, hundreds of patients suffered vision loss or blindness. Others were hospitalized with colitis. Some died.
Yet Elmiron is still on the market today. Doctors continue to prescribe it.
“Hundreds of thousands of patients have been exposed to the drug, and the American Urological Association lists it as the only FDA-approved medication for interstitial cystitis,” Lenzer and Brownlee reported.
“Dangling Approvals” and Regulatory Paralysis
The FDA even has a term—”dangling approvals”—for drugs that remain on the market despite failed or missing follow-up trials.
One notorious case is Avastin, approved in 2008 for metastatic breast cancer.
It was fast-tracked, again, based on ‘progression-free survival.’ But after five clinical trials showed no improvement in overall survival—and raised serious safety concerns—the FDA moved to revoke its approval for metastatic breast cancer.
The backlash was intense.
Drug companies and patient advocacy groups launched a campaign to keep Avastin on the market. FDA staff received violent threats. Police were posted outside the agency’s building.
The fallout was so severe that for more than two decades afterwards, the FDA did not initiate another involuntary drug withdrawal in the face of industry opposition.
Billions Wasted, Thousands Harmed
Between 2018 and 2021, US taxpayers—through Medicare and Medicaid—paid $18 billion for drugs approved under the condition that follow-up studies would be conducted. Many never were.
The cost in lives is even higher.
A 2015 study found that 86% of cancer drugs approved between 2008 and 2012 based on surrogate outcomes showed no evidence that they helped patients live longer.
An estimated 128,000 Americans die each year from the effects of properly prescribed medications—excluding opioid overdoses. That’s more than all deaths from illegal drugs combined.
A 2024 analysis by Danish physician Peter Gøtzsche found that adverse effects from prescription medicines now rank among the top three causes of death globally.
Doctors Misled by the Drug Labels
Despite the scale of the problem, most patients—and most doctors—have no idea.
A 2016 survey published in JAMA asked practising physicians a simple question—what does FDA approval actually mean?
Only 6% got it right.
The rest assumed that it meant the drug had shown clear, clinically meaningful benefits—such as helping patients live longer or feel better—and that the data was statistically sound.
But the FDA requires none of that.
Drugs can be approved based on a single small study, a surrogate endpoint, or marginal statistical findings. Labels are often based on limited data, yet many doctors take them at face value.
Harvard researcher Aaron Kesselheim, who led the survey, said the results were “disappointing, but not entirely surprising,” noting that few doctors are taught about how the FDA’s regulatory process actually works.
Instead, physicians often rely on labels, marketing, or assumptions—believing that if the FDA has authorized a drug, it must be both safe and effective.
But as The Lever investigation shows, that is not a safe assumption.
And without that knowledge, even well-meaning physicians may prescribe drugs that do little good—and cause real harm.
Who Is the FDA Working for?
In interviews with more than 100 experts, patients, and former regulators, Lenzer and Brownlee found widespread concern that the FDA has lost its way.
Many pointed to the agency’s dependence on industry money. A BMJ investigation in 2022 found that user fees now fund two-thirds of the FDA’s drug review budget—raising serious questions about independence.

Yale physician and regulatory expert Reshma Ramachandran said the system is in urgent need of reform.
“We need an agency that’s independent from the industry it regulates and that uses high-quality science to assess the safety and efficacy of new drugs,” she told The Lever. “Without that, we might as well go back to the days of snake oil and patent medicines.”
For now, patients remain unwitting participants in a vast, unspoken experiment—taking drugs that may never have been properly tested, trusting a regulator that too often fails to protect them.
And as Lenzer and Brownlee conclude, that trust is increasingly misplaced.
- Investigative report by Jeanne Lenzer and Shannon Brownlee at The Lever [link]
- Searchable public drug approval database [link]
- See my talk: Failure of Drug Regulation: Declining standards and institutional corruption
Republished from the author’s Substack
Brownstone Institute
The Unmasking of Vaccine Science

From the Brownstone Institute
By
I recently purchased Aaron Siri’s new book Vaccines, Amen. As I flipped though the pages, I noticed a section devoted to his now-famous deposition of Dr Stanley Plotkin, the “godfather” of vaccines.
I’d seen viral clips circulating on social media, but I had never taken the time to read the full transcript — until now.
Siri’s interrogation was methodical and unflinching…a masterclass in extracting uncomfortable truths.
A Legal Showdown
In January 2018, Dr Stanley Plotkin, a towering figure in immunology and co-developer of the rubella vaccine, was deposed under oath in Pennsylvania by attorney Aaron Siri.
The case stemmed from a custody dispute in Michigan, where divorced parents disagreed over whether their daughter should be vaccinated. Plotkin had agreed to testify in support of vaccination on behalf of the father.
What followed over the next nine hours, captured in a 400-page transcript, was extraordinary.
Plotkin’s testimony revealed ethical blind spots, scientific hubris, and a troubling indifference to vaccine safety data.
He mocked religious objectors, defended experiments on mentally disabled children, and dismissed glaring weaknesses in vaccine surveillance systems.
A System Built on Conflicts
From the outset, Plotkin admitted to a web of industry entanglements.
He confirmed receiving payments from Merck, Sanofi, GSK, Pfizer, and several biotech firms. These were not occasional consultancies but long-standing financial relationships with the very manufacturers of the vaccines he promoted.
Plotkin appeared taken aback when Siri questioned his financial windfall from royalties on products like RotaTeq, and expressed surprise at the “tone” of the deposition.
Siri pressed on: “You didn’t anticipate that your financial dealings with those companies would be relevant?”
Plotkin replied: “I guess, no, I did not perceive that that was relevant to my opinion as to whether a child should receive vaccines.”
The man entrusted with shaping national vaccine policy had a direct financial stake in its expansion, yet he brushed it aside as irrelevant.
Contempt for Religious Dissent
Siri questioned Plotkin on his past statements, including one in which he described vaccine critics as “religious zealots who believe that the will of God includes death and disease.”
Siri asked whether he stood by that statement. Plotkin replied emphatically, “I absolutely do.”
Plotkin was not interested in ethical pluralism or accommodating divergent moral frameworks. For him, public health was a war, and religious objectors were the enemy.
He also admitted to using human foetal cells in vaccine production — specifically WI-38, a cell line derived from an aborted foetus at three months’ gestation.
Siri asked if Plotkin had authored papers involving dozens of abortions for tissue collection. Plotkin shrugged: “I don’t remember the exact number…but quite a few.”
Plotkin regarded this as a scientific necessity, though for many people — including Catholics and Orthodox Jews — it remains a profound moral concern.
Rather than acknowledging such sensitivities, Plotkin dismissed them outright, rejecting the idea that faith-based values should influence public health policy.
That kind of absolutism, where scientific aims override moral boundaries, has since drawn criticism from ethicists and public health leaders alike.
As NIH director Jay Bhattacharya later observed during his 2025 Senate confirmation hearing, such absolutism erodes trust.
“In public health, we need to make sure the products of science are ethically acceptable to everybody,” he said. “Having alternatives that are not ethically conflicted with foetal cell lines is not just an ethical issue — it’s a public health issue.”
Safety Assumed, Not Proven
When the discussion turned to safety, Siri asked, “Are you aware of any study that compares vaccinated children to completely unvaccinated children?”
Plotkin replied that he was “not aware of well-controlled studies.”
Asked why no placebo-controlled trials had been conducted on routine childhood vaccines such as hepatitis B, Plotkin said such trials would be “ethically difficult.”
That rationale, Siri noted, creates a scientific blind spot. If trials are deemed too unethical to conduct, then gold-standard safety data — the kind required for other pharmaceuticals — simply do not exist for the full childhood vaccine schedule.
Siri pointed to one example: Merck’s hepatitis B vaccine, administered to newborns. The company had only monitored participants for adverse events for five days after injection.
Plotkin didn’t dispute it. “Five days is certainly short for follow-up,” he admitted, but claimed that “most serious events” would occur within that time frame.
Siri challenged the idea that such a narrow window could capture meaningful safety data — especially when autoimmune or neurodevelopmental effects could take weeks or months to emerge.
Siri pushed on. He asked Plotkin if the DTaP and Tdap vaccines — for diphtheria, tetanus and pertussis — could cause autism.
“I feel confident they do not,” Plotkin replied.
But when shown the Institute of Medicine’s 2011 report, which found the evidence “inadequate to accept or reject” a causal link between DTaP and autism, Plotkin countered, “Yes, but the point is that there were no studies showing that it does cause autism.”
In that moment, Plotkin embraced a fallacy: treating the absence of evidence as evidence of absence.
“You’re making assumptions, Dr Plotkin,” Siri challenged. “It would be a bit premature to make the unequivocal, sweeping statement that vaccines do not cause autism, correct?”
Plotkin relented. “As a scientist, I would say that I do not have evidence one way or the other.”
The MMR
The deposition also exposed the fragile foundations of the measles, mumps, and rubella (MMR) vaccine.
When Siri asked for evidence of randomised, placebo-controlled trials conducted before MMR’s licensing, Plotkin pushed back: “To say that it hasn’t been tested is absolute nonsense,” he said, claiming it had been studied “extensively.”
Pressed to cite a specific trial, Plotkin couldn’t name one. Instead, he gestured to his own 1,800-page textbook: “You can find them in this book, if you wish.”
Siri replied that he wanted an actual peer-reviewed study, not a reference to Plotkin’s own book. “So you’re not willing to provide them?” he asked. “You want us to just take your word for it?”
Plotkin became visibly frustrated.
Eventually, he conceded there wasn’t a single randomised, placebo-controlled trial. “I don’t remember there being a control group for the studies, I’m recalling,” he said.
The exchange foreshadowed a broader shift in public discourse, highlighting long-standing concerns that some combination vaccines were effectively grandfathered into the schedule without adequate safety testing.
In September this year, President Trump called for the MMR vaccine to be broken up into three separate injections.
The proposal echoed a view that Andrew Wakefield had voiced decades earlier — namely, that combining all three viruses into a single shot might pose greater risk than spacing them out.
Wakefield was vilified and struck from the medical register. But now, that same question — once branded as dangerous misinformation — is set to be re-examined by the CDC’s new vaccine advisory committee, chaired by Martin Kulldorff.
The Aluminium Adjuvant Blind Spot
Siri next turned to aluminium adjuvants — the immune-activating agents used in many childhood vaccines.
When asked whether studies had compared animals injected with aluminium to those given saline, Plotkin conceded that research on their safety was limited.
Siri pressed further, asking if aluminium injected into the body could travel to the brain. Plotkin replied, “I have not seen such studies, no, or not read such studies.”
When presented with a series of papers showing that aluminium can migrate to the brain, Plotkin admitted he had not studied the issue himself, acknowledging that there were experiments “suggesting that that is possible.”
Asked whether aluminium might disrupt neurological development in children, Plotkin stated, “I’m not aware that there is evidence that aluminum disrupts the developmental processes in susceptible children.”
Taken together, these exchanges revealed a striking gap in the evidence base.
Compounds such as aluminium hydroxide and aluminium phosphate have been injected into babies for decades, yet no rigorous studies have ever evaluated their neurotoxicity against an inert placebo.
This issue returned to the spotlight in September 2025, when President Trump pledged to remove aluminium from vaccines, and world-leading researcher Dr Christopher Exley renewed calls for its complete reassessment.
A Broken Safety Net
Siri then turned to the reliability of the Vaccine Adverse Event Reporting System (VAERS) — the primary mechanism for collecting reports of vaccine-related injuries in the United States.
Did Plotkin believe most adverse events were captured in this database?
“I think…probably most are reported,” he replied.
But Siri showed him a government-commissioned study by Harvard Pilgrim, which found that fewer than 1% of vaccine adverse events are reported to VAERS.
“Yes,” Plotkin said, backtracking. “I don’t really put much faith into the VAERS system…”
Yet this is the same database officials routinely cite to claim that “vaccines are safe.”
Ironically, Plotkin himself recently co-authored a provocative editorial in the New England Journal of Medicine, conceding that vaccine safety monitoring remains grossly “inadequate.”
Experimenting on the Vulnerable
Perhaps the most chilling part of the deposition concerned Plotkin’s history of human experimentation.
“Have you ever used orphans to study an experimental vaccine?” Siri asked.
“Yes,” Plotkin replied.
“Have you ever used the mentally handicapped to study an experimental vaccine?” Siri asked.
“I don’t recollect…I wouldn’t deny that I may have done so,” Plotkin replied.
Siri cited a study conducted by Plotkin in which he had administered experimental rubella vaccines to institutionalised children who were “mentally retarded.”
Plotkin stated flippantly, “Okay well, in that case…that’s what I did.”
There was no apology, no sign of ethical reflection — just matter-of-fact acceptance.
Siri wasn’t done.
He asked if Plotkin had argued that it was better to test on those “who are human in form but not in social potential” rather than on healthy children.
Plotkin admitted to writing it.
Siri established that Plotkin had also conducted vaccine research on the babies of imprisoned mothers, and on colonised African populations.
Plotkin appeared to suggest that the scientific value of such studies outweighed the ethical lapses—an attitude that many would interpret as the classic ‘ends justify the means’ rationale.
But that logic fails the most basic test of informed consent. Siri asked whether consent had been obtained in these cases.
“I don’t remember…but I assume it was,” Plotkin said.
Assume?
This was post-Nuremberg research. And the leading vaccine developer in America couldn’t say for sure whether he had properly informed the people he experimented on.
In any other field of medicine, such lapses would be disqualifying.
A Casual Dismissal of Parental Rights
Plotkin’s indifference to experimenting on disabled children didn’t stop there.
Siri asked whether someone who declined a vaccine due to concerns about missing safety data should be labelled “anti-vax.”
Plotkin replied, “If they refused to be vaccinated themselves or refused to have their children vaccinated, I would call them an anti-vaccination person, yes.”
Plotkin was less concerned about adults making that choice for themselves, but he had no tolerance for parents making those choices for their own children.
“The situation for children is quite different,” said Plotkin, “because one is making a decision for somebody else and also making a decision that has important implications for public health.”
In Plotkin’s view, the state held greater authority than parents over a child’s medical decisions — even when the science was uncertain.
The Enabling of Figures Like Plotkin
The Plotkin deposition stands as a case study in how conflicts of interest, ideology, and deference to authority have corroded the scientific foundations of public health.
Plotkin is no fringe figure. He is celebrated, honoured, and revered. Yet he promotes vaccines that have never undergone true placebo-controlled testing, shrugs off the failures of post-market surveillance, and admits to experimenting on vulnerable populations.
This is not conjecture or conspiracy — it is sworn testimony from the man who helped build the modern vaccine program.
Now, as Health Secretary Robert F. Kennedy, Jr. reopens long-dismissed questions about aluminium adjuvants and the absence of long-term safety studies, Plotkin’s once-untouchable legacy is beginning to fray.
Republished from the author’s Substack
Brownstone Institute
Bizarre Decisions about Nicotine Pouches Lead to the Wrong Products on Shelves

From the Brownstone Institute
A walk through a dozen convenience stores in Montgomery County, Pennsylvania, says a lot about how US nicotine policy actually works. Only about one in eight nicotine-pouch products for sale is legal. The rest are unauthorized—but they’re not all the same. Some are brightly branded, with uncertain ingredients, not approved by any Western regulator, and clearly aimed at impulse buyers. Others—like Sweden’s NOAT—are the opposite: muted, well-made, adult-oriented, and already approved for sale in Europe.
Yet in the United States, NOAT has been told to stop selling. In September 2025, the Food and Drug Administration (FDA) issued the company a warning letter for offering nicotine pouches without marketing authorization. That might make sense if the products were dangerous, but they appear to be among the safest on the market: mild flavors, low nicotine levels, and recyclable paper packaging. In Europe, regulators consider them acceptable. In America, they’re banned. The decision looks, at best, strange—and possibly arbitrary.
What the Market Shows
My October 2025 audit was straightforward. I visited twelve stores and recorded every distinct pouch product visible for sale at the counter. If the item matched one of the twenty ZYN products that the FDA authorized in January, it was counted as legal. Everything else was counted as illegal.
Two of the stores told me they had recently received FDA letters and had already removed most illegal stock. The other ten stores were still dominated by unauthorized products—more than 93 percent of what was on display. Across all twelve locations, about 12 percent of products were legal ZYN, and about 88 percent were not.
The illegal share wasn’t uniform. Many of the unauthorized products were clearly high-nicotine imports with flashy names like Loop, Velo, and Zimo. These products may be fine, but some are probably high in contaminants, and a few often with very high nicotine levels. Others were subdued, plainly meant for adult users. NOAT was a good example of that second group: simple packaging, oat-based filler, restrained flavoring, and branding that makes no effort to look “cool.” It’s the kind of product any regulator serious about harm reduction would welcome.
Enforcement Works
To the FDA’s credit, enforcement does make a difference. The two stores that received official letters quickly pulled their illegal stock. That mirrors the agency’s broader efforts this year: new import alerts to detain unauthorized tobacco products at the border (see also Import Alert 98-06), and hundreds of warning letters to retailers, importers, and distributors.
But effective enforcement can’t solve a supply problem. The list of legal nicotine-pouch products is still extremely short—only a narrow range of ZYN items. Adults who want more variety, or stores that want to meet that demand, inevitably turn to gray-market suppliers. The more limited the legal catalog, the more the illegal market thrives.
Why the NOAT Decision Appears Bizarre
The FDA’s own actions make the situation hard to explain. In January 2025, it authorized twenty ZYN products after finding that they contained far fewer harmful chemicals than cigarettes and could help adult smokers switch. That was progress. But nine months later, the FDA has approved nothing else—while sending a warning letter to NOAT, arguably the least youth-oriented pouch line in the world.
The outcome is bad for legal sellers and public health. ZYN is legal; a handful of clearly risky, high-nicotine imports continue to circulate; and a mild, adult-market brand that meets European safety and labeling rules is banned. Officially, NOAT’s problem is procedural—it lacks a marketing order. But in practical terms, the FDA is punishing the very design choices it claims to value: simplicity, low appeal to minors, and clean ingredients.
This approach also ignores the differences in actual risk. Studies consistently show that nicotine pouches have far fewer toxins than cigarettes and far less variability than many vapes. The biggest pouch concerns are uneven nicotine levels and occasional traces of tobacco-specific nitrosamines, depending on manufacturing quality. The serious contamination issues—heavy metals and inconsistent dosage—belong mostly to disposable vapes, particularly the flood of unregulated imports from China. Treating all “unauthorized” products as equally bad blurs those distinctions and undermines proportional enforcement.
A Better Balance: Enforce Upstream, Widen the Legal Path
My small Montgomery County survey suggests a simple formula for improvement.
First, keep enforcement targeted and focused on suppliers, not just clerks. Warning letters clearly change behavior at the store level, but the biggest impact will come from auditing distributors and importers, and stopping bad shipments before they reach retail shelves.
Second, make compliance easy. A single-page list of authorized nicotine-pouch products—currently the twenty approved ZYN items—should be posted in every store and attached to distributor invoices. Point-of-sale systems can block barcodes for anything not on the list, and retailers could affirm, once a year, that they stock only approved items.
Third, widen the legal lane. The FDA launched a pilot program in September 2025 to speed review of new pouch applications. That program should spell out exactly what evidence is needed—chemical data, toxicology, nicotine release rates, and behavioral studies—and make timely decisions. If products like NOAT meet those standards, they should be authorized quickly. Legal competition among adult-oriented brands will crowd out the sketchy imports far faster than enforcement alone.
The Bottom Line
Enforcement matters, and the data show it works—where it happens. But the legal market is too narrow to protect consumers or encourage innovation. The current regime leaves a few ZYN products as lonely legal islands in a sea of gray-market pouches that range from sensible to reckless.
The FDA’s treatment of NOAT stands out as a case study in inconsistency: a quiet, adult-focused brand approved in Europe yet effectively banned in the US, while flashier and riskier options continue to slip through. That’s not a public-health victory; it’s a missed opportunity.
If the goal is to help adult smokers move to lower-risk products while keeping youth use low, the path forward is clear: enforce smartly, make compliance easy, and give good products a fair shot. Right now, we’re doing the first part well—but failing at the second and third. It’s time to fix that.
-

 National2 days ago
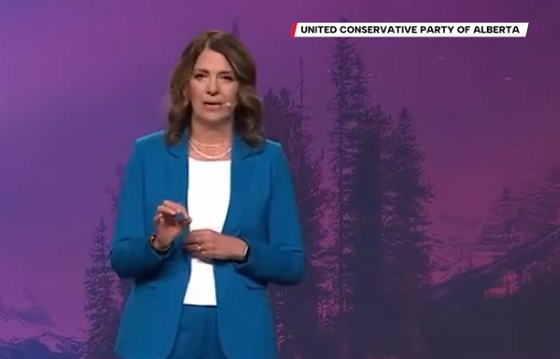
National2 days agoCanada Needs an Alternative to Carney’s One Man Show
-

 Alberta1 day ago
Alberta1 day agoThis new Canada–Alberta pipeline agreement will cost you more than you think
-

 Daily Caller2 days ago
Daily Caller2 days agoTech Mogul Gives $6 Billion To 25 Million Kids To Boost Trump Investment Accounts
-

 Business2 days ago
Business2 days agoRecent price declines don’t solve Toronto’s housing affordability crisis
-

 Automotive1 day ago
Automotive1 day agoPower Struggle: Governments start quietly backing away from EV mandates
-

 Energy1 day ago
Energy1 day agoUnceded is uncertain
-

 Business2 days ago
Business2 days agoCanada’s future prosperity runs through the northwest coast
-

 Business11 hours ago
Business11 hours agoCanada’s climate agenda hit business hard but barely cut emissions