Fraser Institute
Enough talk, we need to actually do something about Canadian health care

From the Macdonald Laurier Institute
By J. Edward Les for Inside Policy
Canada spends more on health care as a percentage of GDP than almost all other OECD countries, yet we rank behind most of them when it comes to outcomes that matter.
I drove a stretch of road near Calgary’s South Health Campus the other day, a section with a series of three intersections in a span of less than a few hundred metres. That is, I tried to drive it – but spent far more time idling than moving.
At each intersection, after an interminable wait, the light turned green just as the next one flipped to red, grinding traffic to a halt just after it got rolling. It was excruciating; I’m quite sure I spied a snail on crutches racing by – no doubt making a beeline (snail-line?) for the ER a stone’s throw away.
The street’s sluggishness is perhaps reflective of the hospital next to it, given that our once-cherished universal health care system has crumbled into a universal waiting system – a system seemingly crafted (like that road) to obstruct flow rather than enable it. In fact, the pace of medical care delivery in this country has become so glacial that even a parking lot by comparison feels like the Indianapolis Speedway.
The health care crisis grows more dire by the day. Reforms are long overdue. Canada spends more on health care as a percentage of GDP than almost all other OECD countries, yet we rank behind most of them when it comes to outcomes that matter.
And we’re paying with our lives: according to the Canadian Institute for Health Information, thousands of Canadians die each and every year because of the inefficiencies of our system.
Yet for all that we are paralyzed by the enormity and complexity of the mushrooming disaster. We talk about solutions – and then we talk and talk some more. But for all the talking, precious little action is taken.
I’m reminded of an Anne Lamotte vignette, related in her bestselling book Bird By Bird:
Thirty years ago my older brother, who was ten years old at the time, was trying to get a report written on birds that he’d had three months to write, which was due the next day. We were out at our family cabin in Bolinas, and he was at the kitchen table close to tears, surrounded by binder paper and pencils and unopened books about birds, immobilized by the hugeness of the task ahead. Then my father sat down beside him, put his arm around my brother’s shoulder, and said, “Bird by bird, buddy. Just take it bird by bird.”
So it is with Canadian health care: we’ve wasted years wringing our hands about the woeful state of affairs, while doing precious little about it.
Enough procrastinating. It’s time to tackle the crisis, bird by bird.
One thing we can do is to let doctors be doctors. A few weeks ago, in a piece titled “Should Doctors Mind Their Own Business?”, I questioned the customary habit of doctors hanging out their shingles in small independent community practices. Physicians spend long years of training to master their craft, years during which they receive no training in business methods whatsoever, and then we expect them to master those skills off to the side of their exam rooms. Some do it well, but many do not – and it detracts from their attention to patients.
We don’t install newly minted teachers in classrooms and at the same time task them with the keeping the lights on, managing the supply chain, overseeing staffing and payroll, and all the other mechanics of running schools. Why do we expect that of doctors?
Keeping doctors embedded within large, expensive, inefficient, bureaucracy-choked hospitals isn’t the solution, either.
There’s a better way, I argued in my essay: regional medical centres – centres built and administered in partnership with the private sector.
Such centres would allow practitioners currently practicing in the community to ply their trade unencumbered by the nuts and bolts of running a business; and they would allow us to decant a host of services from hospitals, which should be reserved for what only hospitals can do: emergency services, inpatient care, surgeries, and the like.
In short, we should let doctors be doctors, and hospitals be hospitals.
To garner feedback, I dumped my musings into a couple of online physician forums to which I belong, tagged with the query: “Food for thought, or fodder for the compost bin?”
The verdict? Hands down, the compost bin.
I was a bit taken aback, initially. Offended, even – because who among us isn’t in love with their own ideas?
But it quickly became evident from my peers’ comments that I’d been misunderstood. Not because my doctor friends are dim, but because I hadn’t been clear.
When I proposed in my essay that we “leave the administration and day-to-day tasks of running those centres to business folks who know what they’re doing,” my colleagues took that to mean that doctors would be serving at the beck and call of a tranche of ill-informed government-enabled administrators – and they reacted to the notion with anaphylactic derision. And understandably so: too many of us have long and painful experience with thick layers of health care bureaucracy seemingly organized according to the Peter Principle, with people promoted to – and permanently stuck at – the level of their incompetence.
But I didn’t mean to suggest – not for a minute – that doctors shouldn’t be engaged in running these centres. I also wrote: “None of which is to suggest that doctors shouldn’t be involved, by aptitude and inclination, in influencing the set-up and management of regional centres – of course, they should.”
Of course they should. There are plenty of physicians equipped with both the skills and interest needed to administer these centres; and they should absolutely be front and centre in leading them.
But more than that: everyone should have skin in the game. All workers have the right to share in the success of an enterprise; and when they do, everybody wins. When everyone is pulling in the same direction because everyone shares in the wins, waste and inefficiencies are rooted out like magic.
Contrast that to how hospitals are run, with scarcely anyone aware of the actual cost of the blood tests or CT scans they order or the packets of suture and gauze they rip open, and with the motivations of administrative staff, nurses, doctors, and other personnel running off in more directions than a flock of headless chickens. The capacity for waste and inefficiencies is almost limitless.
I don’t mean to suggest that the goal of regional medical centres should be to turn a profit; but fiscal prudence and economic accountability are to be celebrated, because money not wasted is money that can be allocated to enhancing patient care.
Nor do I mean to intimate that sensible resource management should be the only parameter tracked; patient outcomes and patient satisfaction are paramount.
What should government’s role be in all this? Initially, to incentivize the creation of these centres via public-private partnerships; and then, crucially, to encourage competition among them and to reward innovation and performance, with optimization of the three key metrics – patient outcomes, patient satisfaction, and economic accountability – always in focus.
No one should be mandated to work in non-hospital regional medical centres. It’s a free country (or it should be): doctors should be free to hang out their own community shingles if they wish. But if we build the model correctly, my contention is that most medical professionals will prefer to work collaboratively under one roof with a diverse group of colleagues, unencumbered by the mundanities of running a business, but also free of choking hospital bureaucracy.
I connected a couple weeks ago with the always insightful economist Jack Mintz (who is also a distinguished fellow at the Macdonald-Laurier Institute). Mintz sits on the board of a Toronto-area hospital and sees first-hand “the problems with the lack of supply, population growth, long wait times between admission and getting a bed, emergency room overuse,” and so on.
“Something has to give,” he said. “Probably more resources but better managed. We really need major reform.”
On that we can all agree. We can’t carry on this way.
So, let’s stop idling; and let’s green-light some fixes.
As Samwise Gamgee said in The Lord of the Rings, “It’s the job that’s never started as takes longest to finish.”
Dr. J. Edward Les is a pediatrician in Calgary who writes on politics, social issues, and other matters.
Fraser Institute
Long waits for health care hit Canadians in their pocketbooks

From the Fraser Institute
Canadians continue to endure long wait times for health care. And while waiting for care can obviously be detrimental to your health and wellbeing, it can also hurt your pocketbook.
In 2024, the latest year of available data, the median wait—from referral by a family doctor to treatment by a specialist—was 30 weeks (including 15 weeks waiting for treatment after seeing a specialist). And last year, an estimated 1.5 million Canadians were waiting for care.
It’s no wonder Canadians are frustrated with the current state of health care.
Again, long waits for care adversely impact patients in many different ways including physical pain, psychological distress and worsened treatment outcomes as lengthy waits can make the treatment of some problems more difficult. There’s also a less-talked about consequence—the impact of health-care waits on the ability of patients to participate in day-to-day life, work and earn a living.
According to a recent study published by the Fraser Institute, wait times for non-emergency surgery cost Canadian patients $5.2 billion in lost wages in 2024. That’s about $3,300 for each of the 1.5 million patients waiting for care. Crucially, this estimate only considers time at work. After also accounting for free time outside of work, the cost increases to $15.9 billion or more than $10,200 per person.
Of course, some advocates of the health-care status quo argue that long waits for care remain a necessary trade-off to ensure all Canadians receive universal health-care coverage. But the experience of many high-income countries with universal health care shows the opposite.
Despite Canada ranking among the highest spenders (4th of 31 countries) on health care (as a percentage of its economy) among other developed countries with universal health care, we consistently rank among the bottom for the number of doctors, hospital beds, MRIs and CT scanners. Canada also has one of the worst records on access to timely health care.
So what do these other countries do differently than Canada? In short, they embrace the private sector as a partner in providing universal care.
Australia, for instance, spends less on health care (again, as a percentage of its economy) than Canada, yet the percentage of patients in Australia (33.1 per cent) who report waiting more than two months for non-emergency surgery was much higher in Canada (58.3 per cent). Unlike in Canada, Australian patients can choose to receive non-emergency surgery in either a private or public hospital. In 2021/22, 58.6 per cent of non-emergency surgeries in Australia were performed in private hospitals.
But we don’t need to look abroad for evidence that the private sector can help reduce wait times by delivering publicly-funded care. From 2010 to 2014, the Saskatchewan government, among other policies, contracted out publicly-funded surgeries to private clinics and lowered the province’s median wait time from one of the longest in the country (26.5 weeks in 2010) to one of the shortest (14.2 weeks in 2014). The initiative also reduced the average cost of procedures by 26 per cent.
Canadians are waiting longer than ever for health care, and the economic costs of these waits have never been higher. Until policymakers have the courage to enact genuine reform, based in part on more successful universal health-care systems, this status quo will continue to cost Canadian patients.
Business
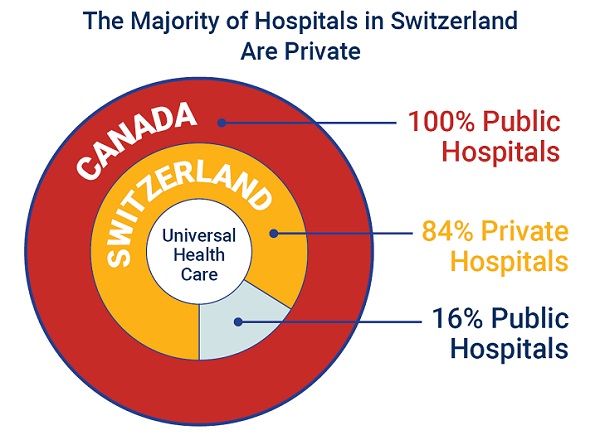
84% of Swiss hospitals and 60% of hospitalizations are in private facilities, and they face much lower wait times
From the Fraser Institute
If Canada reformed to emulate Switzerland’s approach to universal health care, including its much greater use of private sector involvement, the country would deliver far better results to patients and reduce wait times, finds a new study published today by the Fraser Institute, an independent, non-partisan Canadian policy think-tank.
“The bane of Canadian health care is lack of access to timely care, so it’s critical to look to countries like Switzerland with more successful universal health care,” said Yanick Labrie, senior fellow at the Fraser Institute and author of Integrating Private Health Care Into Canada’s Public System: What We Can Learn from Switzerland. The study highlights how Switzerland successfully integrates the private sector into their universal health-care system, which consistently outperforms Canada on most health-care metrics, including wait times.
For example, in 2022, the percentage of patients who waited less than two months for a specialist appointment was 85.3 per cent in Switzerland compared to just 48.3 per cent in Canada.
In Switzerland, 84.2 per cent of all hospitals are private (either for-profit or not-for profit) institutions, and the country’s private hospitals provide 60.2 per cent of all hospitalizations, 60.9 per cent of all births, and 67.1 per cent of all operating rooms.
Crucially, Swiss patients can obtain treatment at the hospital of their choice, whether located inside or outside their geographic location, and hospitals cannot discriminate against patients, based on the care required.
“Switzerland shows that a universal health-care system can reconcile efficiency and equity–all while being more accessible and responsive to patients’ needs and preferences,” Labrie said.
“Based on the success of the Swiss model, provinces can make these reforms now and help improve Canadian health care.”

Integrating Private Health Care into Canada’s Public System: What We Can Learn from Switzerland
- Access to timely care remains the Achilles’ heel of Canada’s health systems. To reduce wait times, some provinces have partnered with private clinics for publicly funded surgeries—a strategy that has proven effective, but continues to spark debate in Canada.
- This study explores how Switzerland successfully integrates private health care into a universal public system and considers what Canada can learn from this model.
- In Switzerland, universal coverage is delivered through a system of managed competition among 44 non-profit private insurers, while decentralized governance allows each of the 26 cantons to coordinate and oversee hospital services in ways that reflect local needs and priorities.
- Nearly two-thirds of Swiss hospitals are for-profit institutions; they provide roughly half of all hospitalizations, births, and hospital beds across the country.
- All hospitals are treated equally—regardless of legal status—and funded through the same activity-based model, implemented nationwide in 2012.
- The reform led to a significant increase in the number of cases treated without a corresponding rise in expenditures per case, suggesting improved efficiency, better use of resources, and expanded access to hospital care.
- The average length of hospital stay steadily decreased over time and now stands at 4.87 days in for-profit hospitals versus 5.53 days in public ones, indicating faster patient turnover and more streamlined care pathways.
- Hospital-acquired infection rates are significantly lower in private hospitals (2.7%) than in public hospitals (6.2%), a key indicator of care quality.
- Case-mix severity is as high or higher in private hospitals, countering the notion that they only take on simpler or less risky cases.
- Patient satisfaction is slightly higher in private hospitals (4.28/5) than in public ones (4.17/5), reflecting strong user experience across multiple dimensions.
- Canada could benefit from regulated competition between public and private providers and activity-based funding, without breaching the Canada Health Act.

-

 Business1 day ago
Business1 day agoCarney’s European pivot could quietly reshape Canada’s sovereignty
-

 Alberta24 hours ago
Alberta24 hours agoAlberta’s grand bargain with Canada includes a new pipeline to Prince Rupert
-

 Crime1 day ago
Crime1 day agoManhunt on for suspect in shooting deaths of Minnesota House speaker, husband
-

 Bruce Dowbiggin9 hours ago
Bruce Dowbiggin9 hours agoWOKE NBA Stars Seems Natural For CDN Advertisers. Why Won’t They Bite?
-

 Crime9 hours ago
Crime9 hours agoMinnesota shooter arrested after 48-hour manhunt
-

 Energy9 hours ago
Energy9 hours agoCould the G7 Summit in Alberta be a historic moment for Canadian energy?
-

 conflict2 hours ago
conflict2 hours agoIsrael bombs Iranian state TV while live on air
-

 Aristotle Foundation6 hours ago
Aristotle Foundation6 hours agoThe Canadian Medical Association’s inexplicable stance on pediatric gender medicine




