Health
Canadians face longest waits for health care on record

From the Fraser Institute
By Bacchus Barua and Mackenzie Moir
Just when you thought Canadian health care had hit rock bottom, wait times in 2024 have hit an all-time high.
According to the latest version of our annual report published by the Fraser Institute, the median wait from referral by a family doctor to treatment (averaged across 10 provinces and 12 medical specialties including surgeries) is now 30 weeks—the longest wait in the report’s history and more than three times longer than the 9.3-week median wait in 1993.
Of course, wait times vary by province, and some provinces are worse than others. In New Brunswick and Prince Edward Island, the median wait is more than one year. And even in Ontario, which reported the shortest wait times in Canada this year, patients faced a 23.6-week wait, the longest in the province’s history.
In fact, compared to last year, wait times grew in every province (except Nova Scotia where patients still faced a median wait just shy of 40 weeks this year).
There’s also considerable variation in wait times depending on the type of care. For example, patients faced the longest waits for orthopedic surgeries (57.5 weeks) and neurosurgery (46.2 weeks) and shorter waits for chemotherapy (4.7 weeks), and radiological cancer treatments (4.5 weeks). In total, the study estimated that Canadian patients were waiting for more than 1.5 million procedures in 2024.
These waits for care are not benign inconveniences. Patients may experience physical pain, psychological distress and worsening physical condition while awaiting care. This year, the 15-week median wait for treatment after seeing a specialist was more than a month and a half longer than what physicians consider a reasonable wait (8.6 weeks). And this doesn’t even include the median 15-week wait to see a specialist in the first place.
Moreover, according to the Commonwealth Fund, a U.S.-based health-care research organization, among nine universal health-care systems worldwide, last year patients in Canada were the second-most likely to report waiting longer than one month for a specialist consultation, and the most likely to report waiting more than two months for surgery. In other words, although long wait times remain a staple of Canadian health care, they are not a necessary trade-off for having universal coverage.
And to be clear, wait times are only one manifestation of the strain on Canada’s health-care system. It’s now also normal to see emergency room closures, health-care worker burnout, and data suggesting millions of Canadians are without access to a regular health-care provider.
What’s the solution to Canada’s crippling health-care wait times?
There are many options for reform. But put simply, if policymakers in Canada want to reduce wait times for patients across the country, they should learn from better-performing universal health-care countries where patients receive more timely care. With wait times this year reaching an all-time high, relief can’t come soon enough.
Addictions
After eight years, Canada still lacks long-term data on safer supply
By Alexandra Keeler
Canada has spent more than $100 million on safer supply programs, but has failed to research their long-term effects
Canada lacks long-term data on safer supply programs, despite funding these programs for years.
Safer supply programs dispense pharmaceutical opioids as a replacement for toxic street drugs.
There is a growing body of research on safer supply’s short-term health effects. But there are no Canadian studies that evaluate program participants’ health impacts beyond 18 months.
The absence of research into long-term data on safer supply means policymakers do not understand how safer supply affects participants’ health, substance use or social outcomes over time.
“Long-term data is important because it helps us understand not just short-term health outcomes like reduced overdoses, but also broader impacts on quality of life, stability and health care use,” said Farihah Ali, scientific lead at the Institute for Mental Health Policy Research at CAMH. The Centre for Addiction and Mental Health is one of Canada’s leading centres for addiction research and clinical care.
Pilot projects
Canada’s first safer supply programs were introduced in Ontario in 2016. Those programs were initially small in scope, intended for a small group of high-risk individuals.
In 2020, the federal government began funding safer supply pilot programs across the country. Provinces are responsible for the delivery and regulation of these programs.
B.C. introduced provincewide programs in 2021. Other provinces, such as Alberta, have restricted safer supply access to a very small number of clinics, and have generally shifted away from harm reduction models in favour of recovery-oriented approaches.
According to the Canadian Public Health Association, an advocacy organization, the original goal for safer supply was to reduce deaths and harms associated with the unregulated toxic drug supply. It was not meant to replace addiction treatment, but to rather act as a bridge to further care.
However, a 2023 report by researchers at McMaster University and Simon Fraser University noted safer supply “does not principally operate toward goals of treatment or recovery.” The report describes safer supply instead as an emergency intervention focused on stabilization and survival.
Evidence gaps
There is a small but growing body of short-term studies on the health effects of Canada’s safer supply programs. Most only track participants’ outcomes for up to 12 months.
Some of those studies suggest safer supply may reduce the immediate harms associated with drug use.
A 2024 study found a 91 per cent reduction in the risk of death among high-risk individuals receiving safer supply in B.C. Critics have raised concerns about the study’s methodology, sample size and confounding variables.
In contrast, a March study suggested B.C.’s safer supply and decriminalization policies may be associated with increased hospitalizations. These findings also sparked controversy, with experts debating how well the data isolate causal impacts.
And a comparative study released in April also showed some positive outcomes from safer supply. It too sparked significant expert debate.
‘Arms-length’
Of all the provinces, B.C. has implemented safer supply most broadly. The province’s health ministry did not directly respond when asked about the long-term goals of its safer supply program, or whether B.C. collects longitudinal data on program participants’ health outcomes.
“Evidence shows [safer supply] helps separate people from the unregulated drug supply, manage their substance use and withdrawal symptoms with regulated medications, and helps connect them to voluntary health and social supports,” a Ministry of Health spokesperson told Canadian Affairs in an email.
The ministry did not provide the evidence it referenced.
At the federal level, Health Canada confirmed that, to date, it has funded just two evaluations of safer supply programs, despite spending more than $100 million on safer supply since April 2023.
The first was a short-term study, funded by the federal government’s Substance Use and Addictions Program program. Conducted over four months, that study assessed 10 safer supply programs in Ontario, B.C., and New Brunswick. It documented initial impacts on participants’ lives and program delivery, primarily through qualitative methods such as interviews and surveys.
The second study is an ongoing, “arms-length evaluation” of 11 safer supply pilot programs funded by the Canadian Institutes of Health Research (CIHR), Canada’s federal health research agency.
When asked about long-term research on safer supply, Health Canada referred Canadian Affairs to a 2022 funding announcement about this multi-year evaluation. While the evaluation is being conducted over several years, it is unclear if it includes long-term tracking of patients’ outcomes.
Barriers and resistance
There are a number of factors that make it challenging to evaluate safer supply programs over long periods.
Ali, of CAMH, says unstable, short-term funding can disrupt long-term research.
“When programs are shut down or scaled back, we lose contact with participants and the ability to track outcomes over time,” she said.
Program participants can also be difficult to track over long periods, she says. Many struggle with housing insecurity, health instability and criminalization.
Frontline staff also face burnout and high turnover, she says, limiting support for such research activities.
Additionally, there are tradeoffs between the anonymity needed to encourage patients to access safer supply programs and the ability to collect detailed data.
“Ethical concerns — like not wanting to burden participants or risk their safety or confidentiality — require us to design studies that are trauma-informed and flexible, which adds complexity to long-term data collection,” Ali said.
Julian Somers, a clinical psychologist and professor at Simon Fraser University, says B.C.’s failure to conduct long-term evaluations of its safer supply programs is not just an oversight, but an act of negligence.
“B.C. has some of the best pharmaceutical data systems in the world,” Somers said, referring to PharmaCare and PharmaNet — databases that capture every prescription drug transaction in the province.
Somers says his team previously used PharmaNet data to examine prescribed opioids’ effects on health and social outcomes. In 2017, he proposed a long-term safer supply evaluation using these tools.
In 2017, he proposed a long-term evaluation of B.C.’s safer supply programs.
The province declined.
According to Ali, “Future research should explore how safer supply impacts people’s long-term health, stability and connection to care.”
“We also need to listen to people’s experiences, how safer supply affects their daily lives, their sense of dignity, and their relationships with care providers through qualitative mechanisms.”
This article was produced through the Breaking Needles Fellowship Program, which provided a grant to Canadian Affairs, a digital media outlet, to fund journalism exploring addiction and crime in Canada. Articles produced through the Fellowship are co-published by Break The Needle and Canadian Affairs.
Addictions
Why B.C.’s new witnessed dosing guidelines are built to fail

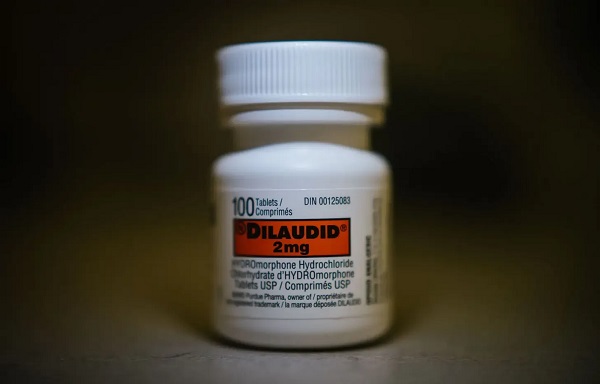
Photo by Acceptable at English Wikipedia, ‘Two 1 mg pills of Hydromorphone, prescribed to me after surgery.’ [Licensed under CC BY-SA 3.0, via Wikimedia Commons]
By Alexandra Keeler
B.C. released new witnessed dosing guidelines for safer supply opioids. Experts say they are vague, loose and toothless
This February, B.C pledged to reintroduce witnessed dosing to its controversial safer supply program.
Safer supply programs provide prescription opioids to people who use drugs. Witnessed dosing requires patients to consume those prescribed opioids under the supervision of a health-care professional, rather than taking their drugs offsite.
The province said it was reintroducing witnessed dosing to “prevent the diversion of prescribed opioids and hold bad actors accountable.”
But experts are saying the government’s interim guidelines, released April 29, are fundamentally flawed.
“These guidelines — just as any guidelines for safer supply — do not align with addiction medicine best practices, period,” said Dr. Leonara Regenstreif, a primary care physician specializing in substance use disorders. Regenstreif is a founding member of Addiction Medicine Canada, an advocacy group that represents 23 addiction specialists.
Addiction physician Dr. Michael Lester, who is also a founding member of the group, goes further.
“Tweaking a treatment protocol that should not have been implemented in the first place without prior adequate study is not much of an advancement,” he said.
Witnessed dosing
Initially, B.C.’s safer supply program was generally administered through witnessed dosing. But in 2020, to facilitate access amidst pandemic restrictions, the province moved to “take-home dosing,” allowing patients to take their prescription opioids offsite.
After pandemic restrictions were lifted, the province did not initially return to witnessed dosing. Rather, it did so only recently, after a bombshell government report alleged more than 60 B.C. pharmacies were boosting sales by encouraging patients to fill unnecessary opioid prescriptions. This incentivized patients to sell their medications on the black market.
B.C.’s interim guidelines, developed by the BC Centre on Substance Use at the government’s request, now require all new safer supply patients to begin with witnessed dosing.
But for existing patients, the guidelines say prescribers have discretion to determine whether to require witnessed dosing. The guidelines define an existing patient as someone who was dispensed prescription opioids within the past 30 days.
The guidelines say exemptions to witnessed dosing are permitted under “extraordinary circumstances,” where witnessed dosing could destabilize the patient or where a prescriber uses “best clinical judgment” and determines diversion risk is “very low.”
Holes
Clinicians say the guidelines are deliberately vague.
Regenstreif described them as “wordy, deliberately confusing.” They enable prescribers to carry on as before, she says.
Lester agrees. Prescribers would be in compliance with these guidelines even if “none of their patients are transferred to witnessed dosing,” he said.
In his view, the guidelines will fail to meet their goal of curbing diversion.
And without witnessed dosing, diversion is nearly impossible to detect. “A patient can take one dose a day and sell seven — and this would be impossible to detect through urine testing,” Lester said.
He also says the guidelines do not remove the incentive for patients to sell their drugs to others. He cites estimates from Addiction Medicine Canada that clients can earn up to $20,000 annually by selling part of their prescribed supply.
“[Prescribed safer supply] can function as a form of basic income — except that the community is being flooded with addictive and dangerous opioids,” Lester said.
Regenstreif warns that patients who had been diverting may now receive unnecessarily high doses. “Now you’re going to give people a high dose of opioids who don’t take opioids,” she said.
She also says the guidelines leave out important details on adjusting doses for patients who do shift from take-home to witnessed dosing.
“If a doctor followed [the guidelines] to the word, and the patient followed it to the word, the patient would go into withdrawal,” she said.
The guidelines assume patients will swallow their pills under supervision, but many crush and inject them instead, Regenstreif says. Because swallowing is less potent, a higher dose may be needed.
“None of that is accounted for in this document,” she said.
Survival strategy
Some harm reduction advocates oppose a return to witnessed dosing, saying it will deter people from accessing a regulated drug supply.
Some also view diversion as a life-saving practice.
Diversion is “a harm reduction practice rooted in mutual aid,” says a 2022 document developed by the National Safer Supply Community of Practice, a group of clinicians and harm reduction advocates.
The group supports take-home dosing as part of a broader strategy to improve access to safer supply medications. In their document, they say barriers to accessing safer supply programs necessitate diversion among people who use drugs — and that the benefits of diversion outweigh the risks.
However, the risks — and harms — of diversion are mounting.
People can quickly develop a tolerance to “safer” opioids and then transition to more dangerous substances. Some B.C. teenagers have said the prescription opioid Dilaudid was a stepping stone to them using fentanyl. In some cases, diversion of these drugs has led to fatal overdoses.
More recently, a Nanaimo man was sentenced to prison for running a highly organized drug operation that trafficked diverted safer supply opioids. He exchanged fentanyl and other illicit drugs for prescription pills obtained from participants in B.C.’s safer supply program.
Recovery
Lester, of Addiction Medicine Canada, believes clinical discretion has gone too far. He says take-home dosing should be eliminated.
“Best practices in addiction medicine assume physicians prescribing is based on sound and thorough research, and ensuring that their prescribing does not cause harm to the broader community, as well as the patient,” he said.
“[Safer supply] for opioids fails in both these regards.”
He also says safer supply should only be offered as a short-term bridge to patients being started on proven treatments like buprenorphine or methadone, which help reduce drug cravings and manage withdrawal symptoms.
B.C.’s witnessed dosing guidelines say prescribers can discuss such treatment options with patients. However, the guidelines remain neutral on whether safer supply is intended as a transitional step toward longer-term treatment.
Regenstreif says this neutrality undermines care.
“[M]ost patients I’ve seen with opioid use disorder don’t want to have [this disorder],” she said. “They would rather be able to set goals and do other things.”
Oversight gaps
Currently, about 3,900 people in B.C. participate in the safer supply program — down from 5,200 in March 2023.
The B.C. government has not provided data on how many have been transitioned to witnessed dosing. Investigative journalist Rob Shaw recently reported that these data do not exist.
“The government … confirmed recently they don’t have any mechanism to track which ‘safe supply’ participants are witnessed and which [are] not,” said Elenore Sturko, a Conservative MLA for Surrey-Cloverdale, who has been a vocal critic of safer supply.
“Without a public report and accountability there can be no confidence.”
The BC Centre on Substance Use, which developed the interim guidelines, says it does not oversee policy decisions or data tracking. It referred Canadian Affairs’ questions to B.C.’s Ministry of Health, which has yet to clarify whether it will track and publish transition data. The ministry did not respond to requests for comment by deadline.
B.C. has also not indicated when or whether it will release final guidelines.
Regenstreif says the flawed guidelines mean many people may be misinformed, discouraged or unsupported when trying to reduce their drug use and recover.
“We’re not listening to people with lived experience of recovery,” she said.
This article was produced through the Breaking Needles Fellowship Program, which provided a grant to Canadian Affairs, a digital media outlet, to fund journalism exploring addiction and crime in Canada. Articles produced through the Fellowship are co-published by Break The Needle and Canadian Affairs.
Subscribe to Break The Needle
-

 Daily Caller2 days ago
Daily Caller2 days ago‘Strange Confluence Of Variables’: Mike Benz Wants Transparency Task Force To Investigate What Happened in Butler, PA
-
 Crime1 day ago
Crime1 day agoDEA Busts Canadian Narco Whose Chinese Supplier Promised to Ship 100 Kilos of Fentanyl Precursors per Month From Vancouver to Los Angeles
-

 conflict2 days ago
conflict2 days agoTrump’s done waiting: 50-day ultimatum for Putin to end Ukraine war
-
 International16 hours ago
International16 hours agoMatt Walsh slams Trump administration’s move to bury Epstein sex trafficking scandal
-

 Alberta1 day ago
Alberta1 day agoMedian workers in Alberta could receive 72% more under Alberta Pension Plan compared to Canada Pension Plan
-

 International1 day ago
International1 day agoBiden autopen scandal: Did unelected aides commit fraud during his final days in office?
-
 Business4 hours ago
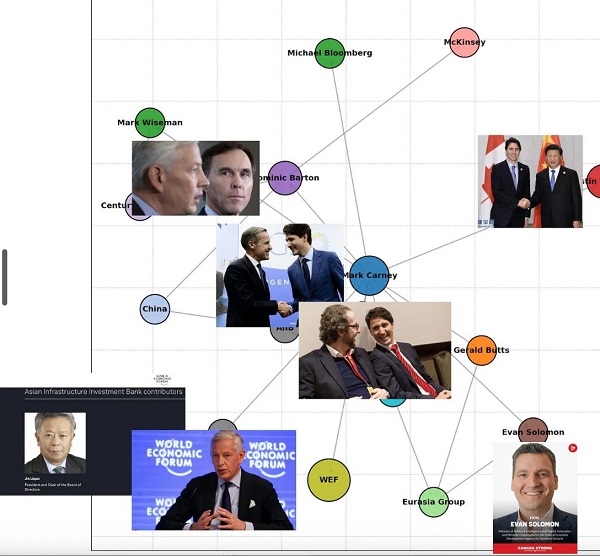
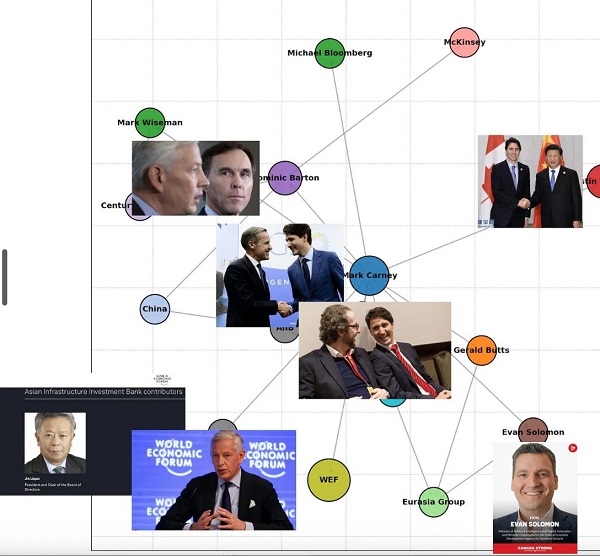
Business4 hours agoDemocracy Watchdog Says PM Carney’s “Ethics Screen” Actually “Hides His Participation” In Conflicted Investments
-

 Energy2 days ago
Energy2 days agoActivists using the courts in attempt to hijack energy policy






