Health
Canadian provinces push back after Trudeau’s health minister says MAiD will eventually be expanded

Liberal Health Minister Mark Holland
From LifeSiteNews
Holland has told Canadians that the government, is still seeking to expand MAiD (Medical Assistance in Dying) to those suffering from mental health issues; it just needs more time to prepare the ‘system.’
The Trudeau government still intends to provide euthanasia to mentally ill Canadians, but provincial health ministers are asking for the measure to be “indefinitely” postponed.
On January 30, health ministers from Ontario, Alberta, New Brunswick, Nova Scotia, Saskatchewan, Prince Edward Island, British Columbia, Yukon, Northwest Territories, and Nunavut appealed to Liberal Health Minister Mark Holland to “indefinitely pause” expanding MAiD eligibility to the mentally ill.
Health ministers from ON, AB, NB, NS, SK, PEI, BC, Yukon, NWT, and Nunavut are calling on Ottawa to "indefinitely pause" expanding MAID eligibility to mental illness.
Concerns about a consistent and safe approach, time for training, and an expected jump in patients#CdnPoli pic.twitter.com/1Hh4oJfsER
— Colton Praill (@ColtonPraill) January 30, 2024
On January 29, Holland told Canadians that the Liberal government, under the leadership of Prime Minister Justin Trudeau, is still seeking to expand MAiD (Medical Assistance in Dying) to those suffering from mental health issues; it just needs more time to prepare the “system.”
“We agree with the conclusion that the committee has come to that the system is not ready, and more time is required,” Holland told reporters, referring to a report that “fundamental issues” regarding the expansion have yet to be resolved.
Trudeau's health minister says "the system is at this time not ready and more time is required" to expand MAiD to those for whom mental illness is "the sole underlying condition" pic.twitter.com/Z4hYcduaWh
— The Post Millennial (@TPostMillennial) January 29, 2024
The new provision, which was to take effect in March, would have relaxed legislation around so-called MAiD to include those suffering solely from mental illness. This is a result of the 2021 passage of Bill C-7, which also allowed the chronically ill – not just the terminally ill – to qualify for so-called doctor-assisted death.
On Monday, following pushback from Canadians, Holland announced that Canada is not ready for the expansion and has determined to delay it. However, Holland stressed that this is not an abandonment of the new policy but merely a postponement.
“There are people who have, for decades, been trapped in mental torture, being in a horrific situation where they have tried everything and exhausted all avenues and under their own recognisance are saying that they want access to MAiD,” he claimed.
“What we’re saying is that … someone in that intractable situation … should have that right, but the system needs to be ready, and the system needs to get it right,” he added, not explaining how being killed would help their situation.
Holland did not reveal when the expansion is expected to take effect but disclosed that “those individuals are gonna have to wait a little longer” to end their lives by lethal injection.
Reporter: "Is your intention to still move ahead with MAiD for mental illness, just within a longer timeframe?"
Trudeau's health minister: "That's correct." pic.twitter.com/XzGs7QoexU
— The Post Millennial (@TPostMillennial) January 29, 2024
The Liberal government’s desire to expand MAiD to those suffering with mental health issues comes despite several experts, and provincial health ministers, warning against the move.
RELATED: Canada’s top pro-life group urges Trudeau gov’t to drop euthanasia expansion entirely
The provincial health ministers’ appeal echoes that of leading Canadian psychiatrist Dr. K. Sonu Gaind, who testified that the expansion of MAiD “is not so much a slippery slope as a runaway train.”
Similarly, in November, several Canadian psychiatrists warned that the country is “not ready” for the coming expansion of euthanasia to those who are mentally ill. They said that further liberalizing the procedure is not something that “society should be doing” as it could lead to deaths under a “false pretence.”
The expansion of euthanasia to those with mental illness even has the far-left New Democratic Party (NDP) concerned. Dismissing these concerns, a Trudeau Foundation fellow actually said Trudeau’s current euthanasia regime is marked by “privilege,” assuring the Canadian people that most of those being put to death are “white,” “well off,” and “highly educated.”
The most recent reports show that MAiD is the sixth highest cause of death. However, it was not listed as such in Statistics Canada’stop 10 leading causes of death from 2019 to 2022. When asked why MAiD was left off the list, the agency explained that it records the illnesses that led Canadians to choose to end their lives via euthanasia, not the actual cause of death, as the primary cause of death.
According to Health Canada, in 2022, 13,241 Canadians died by MAiD lethal injections. This accounts for 4.1 percent of all deaths in the country for that year,a 31.2 percent increase from 2021.
While the numbers for 2023 have yet to be released, all indications point to a situation even more grim than 2022.
Meanwhile, the pro-life Euthanasia Prevention Coalition (EPC)has launched a campaign to have the expansion thrown out. The campaign includes a rally and media conference on Parliament Hill on February 6 at 11 a.m. local time.
The movement also features a parliamentary postcard campaign, encouraging Canadians to send letters stating: “I demand that the government reverse its decision to permit ‘MAiD’ for mental illness alone.”
EPC also launched a petition to urge the Justice Minister to offer real care to those suffering from mental illness and not death by lethal injection.
Business
National dental program likely more costly than advertised

From the Fraser Institute
By Matthew Lau
At the beginning of June, the Canadian Dental Care Plan expanded to include all eligible adults. To be eligible, you must: not have access to dental insurance, have filed your 2024 tax return in Canada, have an adjusted family net income under $90,000, and be a Canadian resident for tax purposes.
As a result, millions more Canadians will be able to access certain dental services at reduced—or no—out-of-pocket costs, as government shoves the costs onto the backs of taxpayers. The first half of the proposition, accessing services at reduced or no out-of-pocket costs, is always popular; the second half, paying higher taxes, is less so.
A Leger poll conducted in 2022 found 72 per cent of Canadians supported a national dental program for Canadians with family incomes up to $90,000—but when asked whether they would support the program if it’s paid for by an increase in the sales tax, support fell to 42 per cent. The taxpayer burden is considerable; when first announced two years ago, the estimated price tag was $13 billion over five years, and then $4.4 billion ongoing.
Already, there are signs the final cost to taxpayers will far exceed these estimates. Dr. Maneesh Jain, the immediate past-president of the Ontario Dental Association, has pointed out that according to Health Canada the average patient saved more than $850 in out-of-pocket costs in the program’s first year. However, the Trudeau government’s initial projections in the 2023 federal budget amounted to $280 per eligible Canadian per year.
Not all eligible Canadians will necessarily access dental services every year, but the massive gap between $850 and $280 suggests the initial price tag may well have understated taxpayer costs—a habit of the federal government, which over the past decade has routinely spent above its initial projections and consistently revises its spending estimates higher with each fiscal update.
To make matters worse there are also significant administrative costs. According to a story in Canadian Affairs, “Dental associations across Canada are flagging concerns with the plan’s structure and sustainability. They say the Canadian Dental Care Plan imposes significant administrative burdens on dentists, and that the majority of eligible patients are being denied care for complex dental treatments.”
Determining eligibility and coverage is a huge burden. Canadians must first apply through the government portal, then wait weeks for Sun Life (the insurer selected by the federal government) to confirm their eligibility and coverage. Unless dentists refuse to provide treatment until they have that confirmation, they or their staff must sometimes chase down patients after the fact for any co-pay or fees not covered.
Moreover, family income determines coverage eligibility, but even if patients are enrolled in the government program, dentists may not be able to access this information quickly. This leaves dentists in what Dr. Hans Herchen, president of the Alberta Dental Association, describes as the “very awkward spot” of having to verify their patients’ family income.
Dentists must also try to explain the program, which features high rejection rates, to patients. According to Dr. Anita Gartner, president of the British Columbia Dental Association, more than half of applications for complex treatment are rejected without explanation. This reduces trust in the government program.
Finally, the program creates “moral hazard” where people are encouraged to take riskier behaviour because they do not bear the full costs. For example, while we can significantly curtail tooth decay by diligent toothbrushing and flossing, people might be encouraged to neglect these activities if their dental services are paid by taxpayers instead of out-of-pocket. It’s a principle of basic economics that socializing costs will encourage people to incur higher costs than is really appropriate (see Canada’s health-care system).
At a projected ongoing cost of $4.4 billion to taxpayers, the newly expanded national dental program is already not cheap. Alas, not only may the true taxpayer cost be much higher than this initial projection, but like many other government initiatives, the dental program already seems to be more costly than initially advertised.
Business
RFK Jr. says Hep B vaccine is linked to 1,135% higher autism rate

From LifeSiteNews
By Matt Lamb
They got rid of all the older children essentially and just had younger children who were too young to be diagnosed and they stratified that, stratified the data
The Centers for Disease Control and Prevention (CDC) found newborn babies who received the Hepatitis B vaccine had 1,135-percent higher autism rates than those who did not or received it later in life, Robert F. Kennedy Jr. told Tucker Carlson recently. However, the CDC practiced “trickery” in its studies on autism so as not to implicate vaccines, Kennedy said.
RFK Jr., who is the current Secretary of Health and Human Services, said the CDC buried the results by manipulating the data. Kennedy has pledged to find the causes of autism, with a particular focus on the role vaccines may play in the rise in rates in the past decades.
The Hepatitis B shot is required by nearly every state in the U.S. for children to attend school, day care, or both. The CDC recommends the jab for all babies at birth, regardless of whether their mother has Hep B, which is easily diagnosable and commonly spread through sexual activity, piercings, and tattoos.
“They kept the study secret and then they manipulated it through five different iterations to try to bury the link and we know how they did it – they got rid of all the older children essentially and just had younger children who were too young to be diagnosed and they stratified that, stratified the data,” Kennedy told Carlson for an episode of the commentator’s podcast. “And they did a lot of other tricks and all of those studies were the subject of those kind of that kind of trickery.”
But now, Kennedy said, the CDC will be conducting real and honest scientific research that follows the highest standards of evidence.
“We’re going to do real science,” Kennedy said. “We’re going to make the databases public for the first time.”
He said the CDC will be compiling records from variety of sources to allow researchers to do better studies on vaccines.
“We’re going to make this data available for independent scientists so everybody can look at it,” the HHS secretary said.
— Matt Lamb (@MattLamb22) July 1, 2025
Health and Human Services also said it has put out grant requests for scientists who want to study the issue further.
Kennedy reiterated that by September there will be some initial insights and further information will come within the next six months.
Carlson asked if the answers would “differ from status quo kind of thinking.”
“I think they will,” Kennedy said. He continued on to say that people “need to stop trusting the experts.”
“We were told at the beginning of COVID ‘don’t look at any data yourself, don’t do any investigation yourself, just trust the experts,”‘ he said.
In a democracy, Kennedy said, we have the “obligation” to “do our own research.”
“That’s the way it should be done,” Kennedy said.
He also reiterated that HHS will return to “gold standard science” and publish the results so everyone can review them.
-

 Agriculture2 days ago
Agriculture2 days agoCanada’s supply management system is failing consumers
-

 Alberta1 day ago
Alberta1 day agoAlberta uncorks new rules for liquor and cannabis
-
 Energy20 hours ago
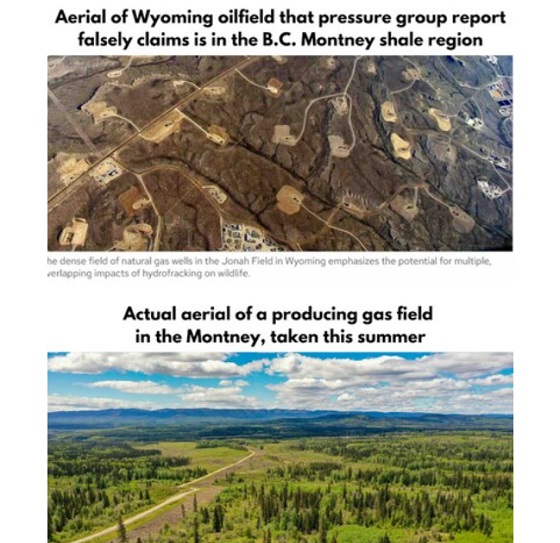
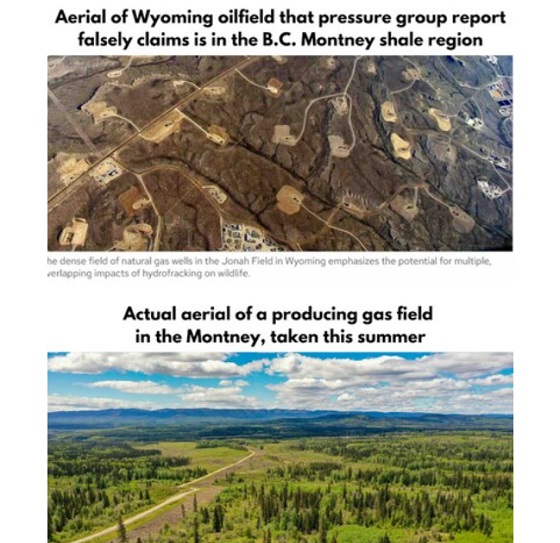
Energy20 hours agoB.C. Residents File Competition Bureau Complaint Against David Suzuki Foundation for Use of False Imagery in Anti-Energy Campaigns
-

 COVID-1920 hours ago
COVID-1920 hours agoCourt compels RCMP and TD Bank to hand over records related to freezing of peaceful protestor’s bank accounts
-

 Crime1 day ago
Crime1 day agoProject Sleeping Giant: Inside the Chinese Mercantile Machine Linking Beijing’s Underground Banks and the Sinaloa Cartel
-

 International1 day ago
International1 day agoTrump transportation secretary tells governors to remove ‘rainbow crosswalks’
-

 Alberta23 hours ago
Alberta23 hours agoAlberta Next: Alberta Pension Plan
-
 C2C Journal17 hours ago
C2C Journal17 hours agoCanada Desperately Needs a Baby Bump