Addictions
Canada is moving ever closer to euthanasia-on-demand without exceptions

From LifeSiteNews
As Canada expands its euthanasia regime, vulnerable individuals like the homeless, obese, and grieving are increasingly offered assisted suicide, countering claims that ‘safeguards’ ensure the protocol remains limited in its scope.
Canada’s suicide activists and euthanasia advocates promised the public that the path to “medical aid in dying” would be a narrow path with high guardrails. They were lying. It is a four-lane highway, and there’s nobody patrolling it.
Not a week goes by without some grim new development, and our government refuses to listen to those hoarsely sounding the alarm.
On October 16, the Associated Press covered the questions euthanasia providers are discussing on their private forums. One story featured a homeless man being killed by lethal injection:
One doctor wrote that although his patient had a serious lung disease, his suffering was “mostly because he is homeless, in debt and cannot tolerate the idea of (long-term care) of any kind.” A respondent questioned whether the fear of living in the nursing home was truly intolerable. Another said the prospect of “looking at the wall or ceiling waiting to be fed … to have diapers changed” was sufficiently painful. The man was eventually euthanized. One provider said any suggestion they should provide patients with better housing options before offering euthanasia “seems simply unrealistic and hence, cruel,” amid a national housing crisis.
Another featured a doctor debating whether obesity made someone eligible for assisted suicide:
One woman with severe obesity described herself as a “useless body taking up space” – she’d lost interest in activities, became socially withdrawn and said she had “no purpose,” according to the doctor who reviewed her case. Another physician reasoned that euthanasia was warranted because obesity is “a medical condition which is indeed grievous and irremediable.”
And perhaps the most chilling story of all is the case of a woman who was consistently pushed into accepting death:
When a health worker inquired whether anyone had euthanized patients for blindness, one provider reported four such cases. In one, they said, an elderly man who saw “only shadows” was his wife’s caregiver when he requested euthanasia; he wanted her to die with him. The couple had several appointments with an assessor before the wife “finally agreed” to be killed, the provider said. She died unexpectedly just days before the scheduled euthanasia.
Read that carefully: the couple had several appointments with the person assessing their eligibility for euthanasia before the wife “finally agreed” – that is, broke down and assented – to be euthanized. Other providers cited examples of people being euthanized for grief. It should be obvious to anyone looking at what is happening in Canada: there are no brakes on this train.
It just keeps getting worse. Linda Maddaford, the newly elected president of the Regina Catholic Women’s League, is sharing her family’s experience this month at the Catholic Health Association of Saskatchewan convention.
After her mother passed away, Maddaford’s family moved their father to a care facility in Saskatoon. “The very day after, we got a blanket email inviting us to come to a presentation in the dining room,” she said. The topic? Accessing euthanasia. Maddaford added that there is a “push from the top-down. That if you don’t – if you aren’t open to the idea; you should be. I worry for the people who feel the pressure of: ‘Well my doctor advised it.’ Or ‘someone with a clipboard came around and kept asking.’”
Another story, covered this month by the Telegraph, relayed the experience of a Canadian woman undergoing life-saving cancer surgery… who was offered assisted suicide by doctors as she was about to enter the operating room for her mastectomy.
None of these stories appear to give euthanasia activists pause. Instead, they are constantly pushing for more.
On October 16, the Financial Post published an editorial by Andrew Roman titled, “You should be able to reserve MAID service: Quebec is going to let people pre-order medical assistance in dying. Ottawa shouldn’t try to stop it. People should have that right.” Anyone still arguing about “rights” as Canadian physicians euthanize patients for grief, obesity, homelessness, disability, and a plethora of other conditions should not be taken seriously. But here’s Roman, arguing that if we don’t permit this, all kinds of elderly people with dementia will not be killed:
As Canada’s population continues to age, demand for MAiD – medical assistance in dying – will only increase. But, with rates of dementia also increasing, the cognitive ability of patients to consent becomes a barrier. The prevalence of dementia more than doubles every five years among seniors, rising from less than one per cent in those aged 65-69 to about 25 per cent among people 85 and older.
Then, revealing a breathtaking ignorance of how Canada’s euthanasia regime has unfolded, Roman writes this:
There is no good reason why, with the numerous safeguards in Ottawa’s and Quebec’s laws, patients should be precluded from making advance requests before their condition renders them incapable of giving consent; and no good reason why their physicians should become criminals for honouring their patients’ duly stipulated advance requests.
No good reason why? Safeguards? What a joke. He concludes:
MAiD is also regulated under provincial law and by the same medical colleges that regulate abortion. Ottawa should amend the Criminal Code to exempt MAiD altogether and, as is the case with abortion, let the medical profession do its work in accordance with provincial regulation and patients’ wishes.
And there you have it: the final goal of the euthanasia activists. Euthanasia on demand; doctors licensed to kill. We don’t have to ask ourselves what will happen if people like Roman get their way. It’s happening already.
Addictions
Why B.C.’s new witnessed dosing guidelines are built to fail

Photo by Acceptable at English Wikipedia, ‘Two 1 mg pills of Hydromorphone, prescribed to me after surgery.’ [Licensed under CC BY-SA 3.0, via Wikimedia Commons]
By Alexandra Keeler
B.C. released new witnessed dosing guidelines for safer supply opioids. Experts say they are vague, loose and toothless
This February, B.C pledged to reintroduce witnessed dosing to its controversial safer supply program.
Safer supply programs provide prescription opioids to people who use drugs. Witnessed dosing requires patients to consume those prescribed opioids under the supervision of a health-care professional, rather than taking their drugs offsite.
The province said it was reintroducing witnessed dosing to “prevent the diversion of prescribed opioids and hold bad actors accountable.”
But experts are saying the government’s interim guidelines, released April 29, are fundamentally flawed.
“These guidelines — just as any guidelines for safer supply — do not align with addiction medicine best practices, period,” said Dr. Leonara Regenstreif, a primary care physician specializing in substance use disorders. Regenstreif is a founding member of Addiction Medicine Canada, an advocacy group that represents 23 addiction specialists.
Addiction physician Dr. Michael Lester, who is also a founding member of the group, goes further.
“Tweaking a treatment protocol that should not have been implemented in the first place without prior adequate study is not much of an advancement,” he said.
Witnessed dosing
Initially, B.C.’s safer supply program was generally administered through witnessed dosing. But in 2020, to facilitate access amidst pandemic restrictions, the province moved to “take-home dosing,” allowing patients to take their prescription opioids offsite.
After pandemic restrictions were lifted, the province did not initially return to witnessed dosing. Rather, it did so only recently, after a bombshell government report alleged more than 60 B.C. pharmacies were boosting sales by encouraging patients to fill unnecessary opioid prescriptions. This incentivized patients to sell their medications on the black market.
B.C.’s interim guidelines, developed by the BC Centre on Substance Use at the government’s request, now require all new safer supply patients to begin with witnessed dosing.
But for existing patients, the guidelines say prescribers have discretion to determine whether to require witnessed dosing. The guidelines define an existing patient as someone who was dispensed prescription opioids within the past 30 days.
The guidelines say exemptions to witnessed dosing are permitted under “extraordinary circumstances,” where witnessed dosing could destabilize the patient or where a prescriber uses “best clinical judgment” and determines diversion risk is “very low.”
Holes
Clinicians say the guidelines are deliberately vague.
Regenstreif described them as “wordy, deliberately confusing.” They enable prescribers to carry on as before, she says.
Lester agrees. Prescribers would be in compliance with these guidelines even if “none of their patients are transferred to witnessed dosing,” he said.
In his view, the guidelines will fail to meet their goal of curbing diversion.
And without witnessed dosing, diversion is nearly impossible to detect. “A patient can take one dose a day and sell seven — and this would be impossible to detect through urine testing,” Lester said.
He also says the guidelines do not remove the incentive for patients to sell their drugs to others. He cites estimates from Addiction Medicine Canada that clients can earn up to $20,000 annually by selling part of their prescribed supply.
“[Prescribed safer supply] can function as a form of basic income — except that the community is being flooded with addictive and dangerous opioids,” Lester said.
Regenstreif warns that patients who had been diverting may now receive unnecessarily high doses. “Now you’re going to give people a high dose of opioids who don’t take opioids,” she said.
She also says the guidelines leave out important details on adjusting doses for patients who do shift from take-home to witnessed dosing.
“If a doctor followed [the guidelines] to the word, and the patient followed it to the word, the patient would go into withdrawal,” she said.
The guidelines assume patients will swallow their pills under supervision, but many crush and inject them instead, Regenstreif says. Because swallowing is less potent, a higher dose may be needed.
“None of that is accounted for in this document,” she said.
Survival strategy
Some harm reduction advocates oppose a return to witnessed dosing, saying it will deter people from accessing a regulated drug supply.
Some also view diversion as a life-saving practice.
Diversion is “a harm reduction practice rooted in mutual aid,” says a 2022 document developed by the National Safer Supply Community of Practice, a group of clinicians and harm reduction advocates.
The group supports take-home dosing as part of a broader strategy to improve access to safer supply medications. In their document, they say barriers to accessing safer supply programs necessitate diversion among people who use drugs — and that the benefits of diversion outweigh the risks.
However, the risks — and harms — of diversion are mounting.
People can quickly develop a tolerance to “safer” opioids and then transition to more dangerous substances. Some B.C. teenagers have said the prescription opioid Dilaudid was a stepping stone to them using fentanyl. In some cases, diversion of these drugs has led to fatal overdoses.
More recently, a Nanaimo man was sentenced to prison for running a highly organized drug operation that trafficked diverted safer supply opioids. He exchanged fentanyl and other illicit drugs for prescription pills obtained from participants in B.C.’s safer supply program.
Recovery
Lester, of Addiction Medicine Canada, believes clinical discretion has gone too far. He says take-home dosing should be eliminated.
“Best practices in addiction medicine assume physicians prescribing is based on sound and thorough research, and ensuring that their prescribing does not cause harm to the broader community, as well as the patient,” he said.
“[Safer supply] for opioids fails in both these regards.”
He also says safer supply should only be offered as a short-term bridge to patients being started on proven treatments like buprenorphine or methadone, which help reduce drug cravings and manage withdrawal symptoms.
B.C.’s witnessed dosing guidelines say prescribers can discuss such treatment options with patients. However, the guidelines remain neutral on whether safer supply is intended as a transitional step toward longer-term treatment.
Regenstreif says this neutrality undermines care.
“[M]ost patients I’ve seen with opioid use disorder don’t want to have [this disorder],” she said. “They would rather be able to set goals and do other things.”
Oversight gaps
Currently, about 3,900 people in B.C. participate in the safer supply program — down from 5,200 in March 2023.
The B.C. government has not provided data on how many have been transitioned to witnessed dosing. Investigative journalist Rob Shaw recently reported that these data do not exist.
“The government … confirmed recently they don’t have any mechanism to track which ‘safe supply’ participants are witnessed and which [are] not,” said Elenore Sturko, a Conservative MLA for Surrey-Cloverdale, who has been a vocal critic of safer supply.
“Without a public report and accountability there can be no confidence.”
The BC Centre on Substance Use, which developed the interim guidelines, says it does not oversee policy decisions or data tracking. It referred Canadian Affairs’ questions to B.C.’s Ministry of Health, which has yet to clarify whether it will track and publish transition data. The ministry did not respond to requests for comment by deadline.
B.C. has also not indicated when or whether it will release final guidelines.
Regenstreif says the flawed guidelines mean many people may be misinformed, discouraged or unsupported when trying to reduce their drug use and recover.
“We’re not listening to people with lived experience of recovery,” she said.
This article was produced through the Breaking Needles Fellowship Program, which provided a grant to Canadian Affairs, a digital media outlet, to fund journalism exploring addiction and crime in Canada. Articles produced through the Fellowship are co-published by Break The Needle and Canadian Affairs.
Subscribe to Break The Needle
Addictions
More young men want to restrict pornography: survey

From LifeSiteNews
Nearly 64% of American men now believe online pornography should be more difficult to access, with even higher numbers of women saying the same thing.
A new survey has shown that an increasing number of young men want more restrictions on online pornography.
According to a survey by the American Enterprise Institute’s Survey Center on American Life, nearly 7 in 10 (69 percent) of Americans support the idea of making online pornography less accessible. In 2013, 65 percent expressed support for policies restricting internet pornography.
The most substantial increase in the support for restrictive measures on pornography could be observed in young men (age 18-24). In 2013, about half of young men favored restrictions, while 40 percent actively opposed such policies. In 2025, 64 percent of men believe accessing online pornography should be made more difficult.
The largest support for restriction on internet pornography overall could be measured among older men (65+), where 73 percent favored restrictions. An even larger percentage of women in each age group supported making online pornography less accessible. Seventy-two percent of young women (age 18-24) favored restriction, while 87 percent of women 55 years or older expressed support for less accessibility of internet pornography.
Viewing pornography is highly addictive and can lead to serious health problems. Studies have shown that children often have their first encounter with pornography at around 12 years old, with boys having a lower average age of about 10-11, and some encountering online pornography as young as 8. Studies have also shown that viewing pornography regularly rewires humans brains and that children, adolescents, and younger men are especially at risk for becoming addicted to online pornography.
According to Gary Wilson’s landmark book on the matter, “Your Brain on Porn,” pornography addiction frequently leads to problems like destruction of genuine intimate relationships, difficulty forming and maintaining real bonds in relationship, depression, social anxiety, as well as reduction of gray matter, leading to desensitization and diminished pleasure from everyday activities among many others.
-

 Business1 day ago
Business1 day agoMark Carney’s Fiscal Fantasy Will Bankrupt Canada
-

 Entertainment2 days ago
Entertainment2 days agoStudy finds 99% of late-night TV guests in 2025 have been liberal
-

 Alberta24 hours ago
Alberta24 hours agoTemporary Alberta grid limit unlikely to dampen data centre investment, analyst says
-

 Opinion1 day ago
Opinion1 day agoCharity Campaigns vs. Charity Donations
-

 Frontier Centre for Public Policy2 days ago
Frontier Centre for Public Policy2 days agoCanada’s New Border Bill Spies On You, Not The Bad Guys
-

 Daily Caller19 hours ago
Daily Caller19 hours ago‘Strange Confluence Of Variables’: Mike Benz Wants Transparency Task Force To Investigate What Happened in Butler, PA
-

 Uncategorized2 days ago
Uncategorized2 days agoCNN’s Shock Climate Polling Data Reinforces Trump’s Energy Agenda
-
 Opinion1 day ago
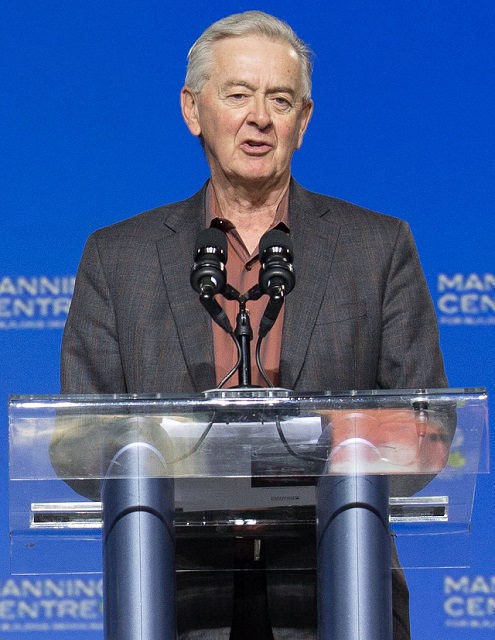
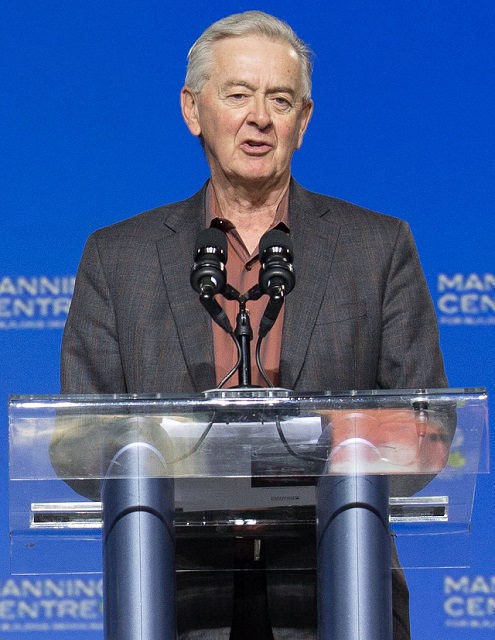
Opinion1 day agoPreston Manning: Three Wise Men from the East, Again




