Crime
Bryan Kohberger avoids death penalty in brutal killing of four Idaho students

Quick Hit:
Bryan Kohberger will plead guilty to murdering four Idaho college students, avoiding a death sentence but leaving victims’ families without answers. The plea deal means he’ll spend life in prison without ever explaining why he committed the brutal 2022 killings.
Key Details:
- Kohberger will plead guilty at a hearing scheduled for Wednesday at 11 a.m. local time.
- The plea deal removes the possibility of death by firing squad but ensures life in prison without parole.
- Victims’ families say the state “failed” them by agreeing to a deal that denies them an explanation for the murders.
Diving Deeper:
Bryan Kohberger, a former PhD criminology student at Washington State University, is expected to plead guilty to the November 2022 murders of four University of Idaho students, sparing himself the death penalty but also avoiding any explanation for his motive. Idaho defense attorney Edwina Elcox told the New York Post that under the plea, Kohberger will have to admit to the killings but won’t have to provide a reason for his actions. “There is no requirement that he says why for a plea,” Elcox explained.
Prosecutors reached the plea deal just weeks before the scheduled trial, which many believed would have revealed the full details and motives behind the shocking quadruple homicide. Kohberger is accused of murdering Kaylee Goncalves, 21; Madison Mogen, 21; Ethan Chapin, 20; and Xana Kernodle, 20, with a military-style Ka-Bar knife as they slept in their off-campus home in Moscow, Idaho. His DNA was allegedly found on a knife sheath left at the scene.
The Goncalves family blasted the state for the deal, saying, “They have failed us.” They had hoped a trial would uncover why Kohberger targeted their daughter and her friends. Prosecutors, however, argued that the plea ensures a guaranteed conviction and prevents the years of appeals that typically follow a death sentence, providing a sense of finality and keeping Kohberger out of the community forever.
Sentencing will not take place for several weeks following Wednesday’s hearing, which is expected to last about an hour as the judge confirms the plea agreement is executed properly. While the families may find some closure in knowing Kohberger will never be free again, they are left without the one thing a trial could have provided: answers.
(AP Photo/Matt Rourke, Pool)
Banks
Welcome Back, Wells Fargo!
 Racket News
Racket News
By Eric Salzman
The heavyweight champion of financial crime gets seemingly its millionth chance to show it’s reformed
The past two decades have been tough ones for Wells Fargo and the many victims of its sprawling crime wave. While the banking industry is full of scammers, Wells took turning time honored street-hustles into multi-billion dollar white-collar hustles to a new level.
The Federal Reserve announced last month that Wells Fargo is no longer subject to the asset growth restriction the Fed finally enforced in 2018 after multiple scandals. This was a major enforcement action that prohibited Wells from growing existing loan portfolios, purchasing other bank branches or entering into any new activities that would result in their asset base growing.
Upon hearing the news that Wells was being released from the Fed’s penalty box, my mind turned to this pivotal moment in the classic movie “Slapshot.”
Here are some of Wells Fargo’s lowlights both before and after the Fed’s enforcement action:
- December 2022: Wells Fargo paid more than $2 billion to consumers and $1.7 billion in civil penalties after the Consumer Financial Protection Bureau (CFPB) found mismanagement — including illegal fees and interest charges — in several of its biggest product lines, such as auto loans, mortgages, and deposit accounts.
- September 2021: Wells Fargo paid $72.6 million to the Justice Department for overcharging foreign exchange customers from 2010-2017.
- February 2020: Wells Fargo paid $3 billion to settle criminal and civil investigations by the Justice Department and SEC into its aggressive sales practices between 2002 and 2016. About $500 million was eventually distributed to investors.
- January 2020: The Office of the Comptroller of the Currency (OCC) banned two senior executives, former CEO John Stumpf and ex-Head of Community Bank Carrie Tolstedt, from the banking industry. Stumpf and Tolstedt also incurred civil penalties of $17.5 million and $17 million.
- August 2018: The Justice Department levied a $2.09 billion fine on Wells Fargo for its actions during the subprime mortgage crisis, particularly its mortgage lending practices between 2005 and 2007.
- April 2018: Federal regulators at the CFPB and OCC examined Wells’ auto loan insurance and mortgage lending practices and ordered the bank to pay $1 billion in damages.
- February 2018: The aforementioned Fed enforcement action. In addition to the asset growth restriction, Wells was ordered to replace three directors.
- October 2017: Wells Fargo admitted wrongdoing after 110,000 clients were fined for missing a mortgage payment deadline — delays for which the bank was ultimately deemed at fault.
- July 2017: As many as 570,000 Wells Fargo customers were wrongly charged for auto insurance on car loans after the bank failed to verify whether those customers already had existing insurance. As a result, up to 20,000 customers may have defaulted on car loans.
- September 2016: Wells Fargo acknowledged its employees had created 1.5 million deposit accounts and 565,000 credit card accounts between 2002 and 2016 that “may not have been authorized by consumers,” according to CFPB. As a result, the lender was forced to pay $185 million in damages to the CFPB, OCC, and City and County of Los Angeles.
Additionally, somehow in 2023 Wells even managed to drop $1 billion in a civil settlement with shareholders for overstating their progress in complying with their 2018 agreement with the Fed to clean themselves up!
I imagine if Wells were in any other business, it wouldn’t be allowed to continue. But Wells is part of the “Too Big to Fail” club. Taking away its federal banking charter would be too disruptive for the financial markets, so instead they got what ended up being a seven-year growth ban. Not exactly rough justice.
While not the biggest settlement, my favorite Wells scam was the 2021 settlement of the seven-year pilfering operation, ripping off corporate customers’ foreign exchange transactions.
Like many banks, Wells Fargo offers its corporate clients with global operations foreign exchange (FX) services. For example, if a company is based in the U.S. but has extensive dealings in Canada, it may receive payments in Canadian dollars (CAD) that need to be exchanged for U.S. dollars (USD) and vice versa. Wells, like many banks, has foreign exchange specialists who do these conversions. Ideally, the banks optimize their clients’ revenue and decrease risk, in return for a markup fee, or “spread.”
There’s a lot of trust involved with this activity as the corporate customers generally have little idea where FX is trading minute by minute, nor do they know what time of day the actual orders for FX transactions — commonly called “BSwifts” — come in. For an unscrupulous bank, it’s a license to steal, which is exactly what Wells did.
According to the complaint, Wells regularly marked up transactions at higher spreads than what was agreed upon. This was just one of the variety of naughty schemes Wells used to clobber their customers. My two favorites were “The Big Figure Trick” and the “BSwift Pinata.”
The Big Figure Trick
Let’s say a client needs to sell USD for CAD, and that the $1 USD is worth $1.32 CAD. In banking parlance, the 32 cents is called the “Big Figure.” Wells would buy the CAD at $1.32 for $1 USD and then transpose the actual exchange rate on the customer statement from $1.32 to $1.23. If the customer didn’t notice, Wells would pocket the difference. On a transaction where the client is buying 5 million CAD with USD, the ill-gotten gain for Wells would be about $277,000 USD!
Conversely, if the customer did notice the difference, Wells would just blame it on the grunts in its operational back office, saying they accidentally transposed the number and “correct” the transaction. From the complaint, here is some give and take between two Wells FX specialists:
“You can play the transposition error game if you get called out.” Another FX sales specialist noted to a colleague about a previous transaction that a customer “didn’t flinch at the big fig the other day. Want to take a bit more?”
The BSwift Piñata
The way this hustle would work is, let’s say the Wells corporate customer was receiving payment from one of their Canadian clients. The Canadian client’s bank would send a BSwift message to Wells. The Wells client was in the dark about the U.S. dollar-Canadian dollar exchange rate because it had no idea what time of day the message arrived. Wells took advantage of that by purchasing U.S. dollars for Canadian dollars first. For simplicity, think of the U.S. dollar-Canadian dollar exchange rate as a widget that Wells bought for $1. If the widget increased in value, say to $1.10 during the day, Wells would sell the widget they purchased for $1 to the client for $1.10 and pocket 10 cents. If the price of the widget Wells bought for $1 fell to 95 cents, Wells would just give up their $1 purchase to the client, plus whatever markup they agreed to.
Heads, Wells wins. Tails, client loses.
The complaint notes that a Wells FX specialist wrote that he:
“Bumped spreads up a pinch,” that “these clients who are in the mode of just processing wires will most likely not notice this slight change in pricing” and that it “could have a very quick positive impact on revenue without a lot of risk.”
Talk about a boiler room operation. Personally, I think calling what you are doing to a client a “piñata” should have easily put Wells in the Fed’s penalty box another 5 years at least!
Wells has been released from the Fed’s 2018 enforcement order. I would like to think they have learned their lesson and are reformed, but I would lay good odds against it. A leopard can’t change its spots.
Racket News is a reader-supported publication.
Consider becoming a free or paid subscriber.
Crime
National Health Care Fraud Takedown Results in 324 Defendants Charged in Connection with Over $14.6 Billion in Alleged Fraud
A 50-district dragnet uncovers transnational fraud, AI-driven deception, and systemic theft from Medicare, Medicaid, and U.S. taxpayers totaling over $14.6 billion
The Department of Justice announced Monday the outcome of the 2025 National Health Care Fraud Takedown, the largest coordinated enforcement action against health care fraud in U.S. history. Federal prosecutors have filed criminal charges against 324 individuals across 50 federal judicial districts and 12 State Attorneys General’s Offices, including 96 licensed medical professionals—among them doctors, nurse practitioners, and pharmacists. The defendants stand accused of orchestrating fraudulent schemes amounting to more than $14.6 billion in intended losses to Medicare, Medicaid, and other federally funded programs.

This historic enforcement action more than doubles the previous national record of $6 billion. As part of this effort, federal and state authorities have seized over $245 million in cash, luxury vehicles, cryptocurrency, and other high-value assets. The Centers for Medicare & Medicaid Services (CMS) separately reported that it successfully prevented more than $4 billion in fraudulent payments in the months leading up to the Takedown. CMS also confirmed that it suspended or revoked the billing privileges of 205 providers linked to fraudulent activity. In the civil domain, federal agencies filed actions against 20 defendants tied to $14.2 million in alleged fraud and finalized civil settlements with an additional 106 defendants, totaling $34.3 million in recovered funds.
The Takedown was led by the Health Care Fraud Unit of the DOJ Criminal Division’s Fraud Section and carried out in close coordination with U.S. Attorneys’ Offices nationwide, the Department of Health and Human Services Office of Inspector General (HHS-OIG), the Federal Bureau of Investigation (FBI), the Drug Enforcement Administration (DEA), and multiple state law enforcement agencies. Medicaid Fraud Control Units in 18 states also played a central role in investigating and prosecuting the cases.
In remarks accompanying the announcement, Secretary of Health and Human Services Robert F. Kennedy Jr. emphasized that the agency would aggressively work with law enforcement to eliminate the “pervasive health care fraud that drove up costs and harmed patients under the former administration.” Attorney General Pamela Bondi echoed the urgency, calling the action “justice delivered to those who steal from taxpayers and endanger lives.” Matthew R. Galeotti, head of the Justice Department’s Criminal Division, underscored the gravity of the crimes targeted, noting that fraudulent schemes often lead not only to financial losses but also to direct patient harm, including medically unnecessary procedures and worsened addiction outcomes.
FBI Director Kash Patel emphasized that this Takedown represents the largest in the bureau’s history, highlighting the theft of more than $13 billion from federal health programs. Acting Inspector General Juliet T. Hodgkins of HHS-OIG described the scale of harm as unprecedented and reaffirmed the agency’s commitment to safeguarding the public.
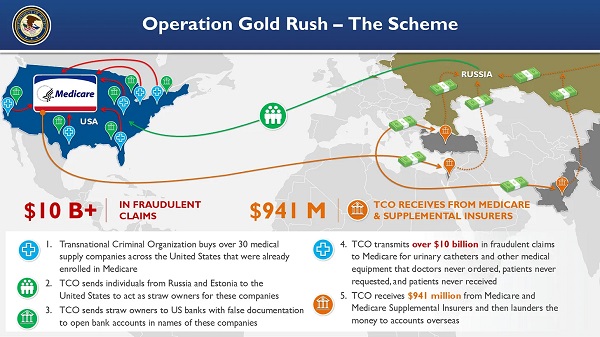
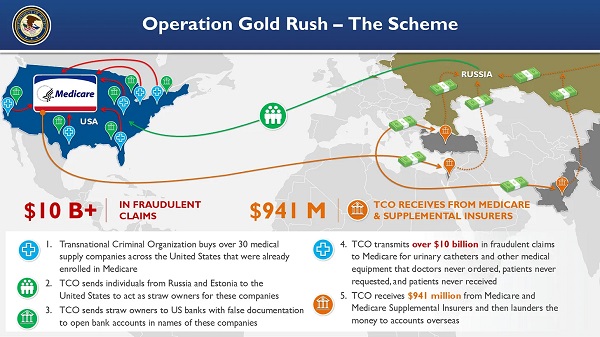
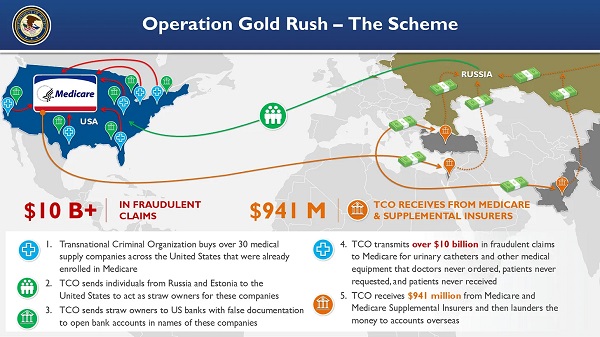
Among the most significant components of this national operation was Operation Gold Rush, which uncovered a sophisticated transnational conspiracy responsible for over $10 billion in fraudulent Medicare claims. The scheme was orchestrated by foreign nationals who, acting as a coordinated criminal enterprise, acquired more than 30 medical supply companies across the United States. These companies had already been enrolled in Medicare, and were then used to funnel false claims for urinary catheters and other durable medical equipment. Stolen identities of over one million Americans were used to submit these claims, which had not been requested by patients, nor ordered by physicians.
The conspiracy relied on straw owners sent from Russia and Estonia to the U.S., who were directed by co-conspirators communicating through encrypted channels. Using fraudulent documentation, these straw owners opened U.S. bank accounts for laundering proceeds. Though the organization submitted over $10.6 billion in claims, CMS successfully blocked most of the payments. Only approximately $41 million reached the conspirators via Medicare, but approximately $900 million was disbursed by Medicare supplemental insurers before the fraud was detected.
Four individuals were arrested in Estonia and eight others were apprehended at major U.S. airports and border crossings as they attempted to flee. Law enforcement seized approximately $27.7 million in fraud proceeds from this operation.

Federal prosecutors filed related charges in five districts: the Central District of California, the Middle District of Florida, the Northern District of Illinois, the District of New Jersey, and the Eastern District of New York.
In a separate scheme centered in Illinois, the Department brought charges against five individuals, including two executives from Pakistani marketing firms, who used artificial intelligence to generate fake audio recordings of Medicare beneficiaries purporting to consent to receive medical equipment. This fraudulent data was sold to laboratories and equipment suppliers, which used it to file $703 million in false claims. Approximately $418 million was ultimately paid out on these claims, and the government has so far seized $44.7 million in related assets. The fraud involved not only AI-based deception but also the illegal sale and laundering of stolen personal health information.
Another case exposed a billing company executive based in Pakistan and the United Arab Emirates who conspired with addiction treatment centers to submit approximately $650 million in fraudulent claims to Arizona Medicaid. Some services billed were never rendered, and others were so deficient as to provide no therapeutic value. The operation targeted vulnerable individuals, including members of Native American tribes and the homeless. Kickbacks were paid for patient referrals, and the executive used at least $25 million in illicit funds to purchase a $2.9 million home in Dubai.

The Department also charged 49 defendants in connection with over $1.17 billion in fraudulent claims tied to telemedicine and genetic testing. In one Florida case, an owner of both telemedicine and durable medical equipment companies orchestrated a $46 million scheme involving deceptive telemarketing campaigns that generated unauthorized genetic testing and equipment claims. The Department continues to prioritize cases involving telehealth-based fraud, which often exploits unwitting patients through misrepresented or manufactured consent.
Prescription opioid diversion was another central focus of the Takedown. A total of 74 defendants, including 44 licensed medical professionals, were charged across 58 criminal cases for illegally distributing more than 15 million opioid pills. One Texas pharmacy alone was responsible for over 3 million of these pills, which included highly addictive substances such as oxycodone, hydrocodone, and carisoprodol. The DEA concurrently announced 93 administrative actions to revoke licenses and registrations of pharmacies and providers implicated in the unlawful handling of controlled substances.
Other cases include a $28.7 million scheme in Tennessee involving medications falsely billed to the Federal Employees’ Compensation Fund, where prescriptions were neither authorized by physicians nor dispensed as claimed. In separate indictments filed in Washington and California, medical providers were charged with stealing fentanyl and hydrocodone intended for pediatric patients under anesthesia.
The geographic scope of the Takedown was vast. In total, 189 federal cases were filed across all 50 federal judicial districts, and 91 state-level cases were brought in 12 states by participating Attorneys General. This unprecedented coordination underscores the national impact and bipartisan support for rooting out fraud in American health care systems.
To enhance ongoing efforts, the Department also announced the establishment of a new Health Care Fraud Data Fusion Center.

This joint initiative brings together specialists from the DOJ’s Health Care Fraud Unit, HHS-OIG, FBI, and CMS to leverage cloud computing, artificial intelligence, and large-scale data analytics to detect emergent fraud patterns. The Fusion Center aligns with Executive Order 14243, “Stopping Waste, Fraud, and Abuse by Eliminating Information Silos,” which mandates interagency cooperation and data-sharing to reduce redundancy and increase efficiency in enforcement.
Principal Assistant Deputy Chief Jacob Foster, Assistant Deputy Chief Rebecca Yuan, Trial Attorney Miriam L. Glaser Dauermann, and Data Analyst Elizabeth Nolte coordinated this year’s Takedown from within the DOJ’s Health Care Fraud Unit. Prosecutors from the National Rapid Response team and regional Strike Forces in 27 districts led casework alongside U.S. Attorneys’ Offices and 18 state Medicaid Fraud Control Units. Additional support came from the Department of Labor, VA-OIG, IRS Criminal Investigation, Homeland Security Investigations, the Defense Criminal Investigative Service, the Office of Personnel Management, the United States Postal Service OIG, and numerous other federal and local agencies.
Image sources: US DOJ
-

 Business1 day ago
Business1 day agoRFK Jr. says Hep B vaccine is linked to 1,135% higher autism rate
-

 Business17 hours ago
Business17 hours agoWhy it’s time to repeal the oil tanker ban on B.C.’s north coast
-
 Crime2 days ago
Crime2 days agoNational Health Care Fraud Takedown Results in 324 Defendants Charged in Connection with Over $14.6 Billion in Alleged Fraud
-

 Censorship Industrial Complex2 days ago
Censorship Industrial Complex2 days agoGlobal media alliance colluded with foreign nations to crush free speech in America: House report
-
 Alberta12 hours ago
Alberta12 hours agoAlberta Provincial Police – New chief of Independent Agency Police Service
-

 Health2 days ago
Health2 days agoRFK Jr. Unloads Disturbing Vaccine Secrets on Tucker—And Surprises Everyone on Trump
-

 Opinion9 hours ago
Opinion9 hours agoBlind to the Left: Canada’s Counter-Extremism Failure Leaves Neo-Marxist and Islamist Threats Unchecked
-

 Alberta17 hours ago
Alberta17 hours agoPierre Poilievre – Per Capita, Hardisty, Alberta Is the Most Important Little Town In Canada

 By
By