Fraser Institute
Australia’s universal health-care system outperforms Canada on key measures including wait times, costs less and includes large role for private hospitals

The Role of Private Hospitals in Australia’s Universal Health Care System
From the Fraser Institute
by Mackenzie Moir and Bacchus Barua
In the wake of the COVID-19 pandemic, provincial governments across Canada relied on private
clinics in order to deliver a limited number of publicly funded surgeries in a bid to clear unprecedented
surgical backlogs. Subsequently, surveys indicated that 78% of Canadians support allowing more
surgeries and tests performed in private clinics while 40% only support this policy to clear the
surgical backlog. While a majority of Canadians are either supportive (or at the very least curious)
about these arrangements, the use of private clinics continues to be controversial and raise questions
around their compatibility with the provision of universal care.
The reality is that private hospitals play a key role in delivering care to patients in other countries with universal health care. Canada is only one of 30 high-income countries with universal care and many of these countries involve the private-sector in their health-care systems to a wide extent while performing better than Canada.
Australia is one of these countries and routinely outperforms Canada on key indicators of health-care performance while spending at a similar or lower level. Like Canada, Australia ranked
in the top ten for health-care spending (as a percentage of GDP and per capita) in 2020. However, after adjusting for the age of the population, it outperforms Canada on 33 (of 36) measures of performance.
Importantly, Australia outperformed Canada on a number of key measures such as the availability of physicians, nurses, hospital beds, CT scanners, and MRI machines. Australia also outperformed
Canada on every indicator of timely access to care, including ease of access to after-hours care, same-day primary care appointments, and, crucially, timely access to elective surgical care and specialist appointments.
Australia’s universal system is also characterized by a deep integration between the public and private sectors in the financing and delivery of care. Universal health-insurance coverage is provided through its public system known as Medicare. However, Australia also has a large private health-care sector that also finances and delivers medical services. Around half of the Australian population (55.2% in 2021/22) benefit from private health-insurance coverage provided by 33 registered not-for-profit and for-profit private insurance companies.
Private hospitals (for profit and not for profit) made up nearly half (48.5%) of all Australian hospitals in 2016 and contain a third of all care beds. These hospitals are a major partner in the delivery of care in Australia. For example, in 2021/22 41% of all recorded episodes of hospital care occurred in private hospitals. While delivering a small minority of emergency care (8.2%), private hospitals delivered the majority of recorded elective care (58.6%) and 70.3% of elective admissions involving surgery.
Private hospitals primarily deliver care to fully funded public patients in two ways. The first is contracted
care, either through ad hoc inter-hospital contracts or formal programs. Fully publicly funded episodes of care occurring in private hospitals made up 6.4% of all care in private hospitals, while representing 2.6% of all recorded care. The second way is privately delivered care paid for through the Department of Veterans’ Affairs. A full 73.5% of care paid for by the Department of Veterans’ Affairs occurred in private hospitals.
It would be easy, however, to underestimate the significance of this public-private partnership by examining only the delivery of care that is fully publicly funded. Privately insured care is also partially subsidized by the government, at a rate of 75% of the public fee. Therefore, in order to understand the full extent of publicly funded or subsidized care in private hospitals, it is helpful to examine private hospital expenditures by the source of funds. In 2019/20, 32.8% of private hospital expenditures came from government sources, 18.2% of which came from private health-insurance rebates. This means that a full
third of private hospital expenditure comes from a range of public sources, including the federal government.
Overall, private hospitals are important partners in the delivery of care within the Australian universal healthcare system. The Australian system outranks Canada’s on a range of performance indicators, while spending less as a percentage of GDP. Further, the integration of private hospitals into the delivery of care, including public care, occurs while maintaining universal access for residents.
Authors:
More from this study
Fraser Institute
Long waits for health care hit Canadians in their pocketbooks

From the Fraser Institute
Canadians continue to endure long wait times for health care. And while waiting for care can obviously be detrimental to your health and wellbeing, it can also hurt your pocketbook.
In 2024, the latest year of available data, the median wait—from referral by a family doctor to treatment by a specialist—was 30 weeks (including 15 weeks waiting for treatment after seeing a specialist). And last year, an estimated 1.5 million Canadians were waiting for care.
It’s no wonder Canadians are frustrated with the current state of health care.
Again, long waits for care adversely impact patients in many different ways including physical pain, psychological distress and worsened treatment outcomes as lengthy waits can make the treatment of some problems more difficult. There’s also a less-talked about consequence—the impact of health-care waits on the ability of patients to participate in day-to-day life, work and earn a living.
According to a recent study published by the Fraser Institute, wait times for non-emergency surgery cost Canadian patients $5.2 billion in lost wages in 2024. That’s about $3,300 for each of the 1.5 million patients waiting for care. Crucially, this estimate only considers time at work. After also accounting for free time outside of work, the cost increases to $15.9 billion or more than $10,200 per person.
Of course, some advocates of the health-care status quo argue that long waits for care remain a necessary trade-off to ensure all Canadians receive universal health-care coverage. But the experience of many high-income countries with universal health care shows the opposite.
Despite Canada ranking among the highest spenders (4th of 31 countries) on health care (as a percentage of its economy) among other developed countries with universal health care, we consistently rank among the bottom for the number of doctors, hospital beds, MRIs and CT scanners. Canada also has one of the worst records on access to timely health care.
So what do these other countries do differently than Canada? In short, they embrace the private sector as a partner in providing universal care.
Australia, for instance, spends less on health care (again, as a percentage of its economy) than Canada, yet the percentage of patients in Australia (33.1 per cent) who report waiting more than two months for non-emergency surgery was much higher in Canada (58.3 per cent). Unlike in Canada, Australian patients can choose to receive non-emergency surgery in either a private or public hospital. In 2021/22, 58.6 per cent of non-emergency surgeries in Australia were performed in private hospitals.
But we don’t need to look abroad for evidence that the private sector can help reduce wait times by delivering publicly-funded care. From 2010 to 2014, the Saskatchewan government, among other policies, contracted out publicly-funded surgeries to private clinics and lowered the province’s median wait time from one of the longest in the country (26.5 weeks in 2010) to one of the shortest (14.2 weeks in 2014). The initiative also reduced the average cost of procedures by 26 per cent.
Canadians are waiting longer than ever for health care, and the economic costs of these waits have never been higher. Until policymakers have the courage to enact genuine reform, based in part on more successful universal health-care systems, this status quo will continue to cost Canadian patients.
Business
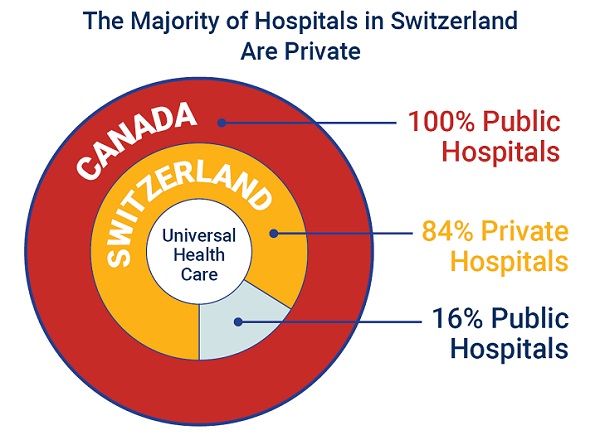
84% of Swiss hospitals and 60% of hospitalizations are in private facilities, and they face much lower wait times
From the Fraser Institute
If Canada reformed to emulate Switzerland’s approach to universal health care, including its much greater use of private sector involvement, the country would deliver far better results to patients and reduce wait times, finds a new study published today by the Fraser Institute, an independent, non-partisan Canadian policy think-tank.
“The bane of Canadian health care is lack of access to timely care, so it’s critical to look to countries like Switzerland with more successful universal health care,” said Yanick Labrie, senior fellow at the Fraser Institute and author of Integrating Private Health Care Into Canada’s Public System: What We Can Learn from Switzerland. The study highlights how Switzerland successfully integrates the private sector into their universal health-care system, which consistently outperforms Canada on most health-care metrics, including wait times.
For example, in 2022, the percentage of patients who waited less than two months for a specialist appointment was 85.3 per cent in Switzerland compared to just 48.3 per cent in Canada.
In Switzerland, 84.2 per cent of all hospitals are private (either for-profit or not-for profit) institutions, and the country’s private hospitals provide 60.2 per cent of all hospitalizations, 60.9 per cent of all births, and 67.1 per cent of all operating rooms.
Crucially, Swiss patients can obtain treatment at the hospital of their choice, whether located inside or outside their geographic location, and hospitals cannot discriminate against patients, based on the care required.
“Switzerland shows that a universal health-care system can reconcile efficiency and equity–all while being more accessible and responsive to patients’ needs and preferences,” Labrie said.
“Based on the success of the Swiss model, provinces can make these reforms now and help improve Canadian health care.”

Integrating Private Health Care into Canada’s Public System: What We Can Learn from Switzerland
- Access to timely care remains the Achilles’ heel of Canada’s health systems. To reduce wait times, some provinces have partnered with private clinics for publicly funded surgeries—a strategy that has proven effective, but continues to spark debate in Canada.
- This study explores how Switzerland successfully integrates private health care into a universal public system and considers what Canada can learn from this model.
- In Switzerland, universal coverage is delivered through a system of managed competition among 44 non-profit private insurers, while decentralized governance allows each of the 26 cantons to coordinate and oversee hospital services in ways that reflect local needs and priorities.
- Nearly two-thirds of Swiss hospitals are for-profit institutions; they provide roughly half of all hospitalizations, births, and hospital beds across the country.
- All hospitals are treated equally—regardless of legal status—and funded through the same activity-based model, implemented nationwide in 2012.
- The reform led to a significant increase in the number of cases treated without a corresponding rise in expenditures per case, suggesting improved efficiency, better use of resources, and expanded access to hospital care.
- The average length of hospital stay steadily decreased over time and now stands at 4.87 days in for-profit hospitals versus 5.53 days in public ones, indicating faster patient turnover and more streamlined care pathways.
- Hospital-acquired infection rates are significantly lower in private hospitals (2.7%) than in public hospitals (6.2%), a key indicator of care quality.
- Case-mix severity is as high or higher in private hospitals, countering the notion that they only take on simpler or less risky cases.
- Patient satisfaction is slightly higher in private hospitals (4.28/5) than in public ones (4.17/5), reflecting strong user experience across multiple dimensions.
- Canada could benefit from regulated competition between public and private providers and activity-based funding, without breaching the Canada Health Act.

-

 conflict2 days ago
conflict2 days agoIran nuclear talks were ‘coordinated deception’ between US and Israel: report
-
 Alberta2 days ago
Alberta2 days agoPunishing Alberta Oil Production: The Divisive Effect of Policies For Carney’s “Decarbonized Oil”
-

 International2 days ago
International2 days agoIsrael’s Decapitation Strike on Iran Reverberates Across Global Flashpoints
-

 Energy2 days ago
Energy2 days agoCanada is no energy superpower
-

 Alberta2 days ago
Alberta2 days agoAlberta Premier Danielle Smith Discusses Moving Energy Forward at the Global Energy Show in Calgary
-

 Health2 days ago
Health2 days agoJust 3 Days Left to Win the Dream Home of a Lifetime!
-

 Fraser Institute2 days ago
Fraser Institute2 days agoLong waits for health care hit Canadians in their pocketbooks
-

 conflict1 day ago
conflict1 day agoOne dead, over 60 injured after Iranian missiles pierce Iron Dome