Health
3+ million Canadians waiting for basic care as health system crisis continues

From LifeSiteNews
Canada’s health system crisis continues as a new report shows over 3.2 million citizens are stuck waiting for basic care including surgeries, diagnostic scans and appointments with specialists.
Millions of Canadians seeking healthcare have been waitlisted, according to most recent reports.
In an October 24 press release, Canadian think tank SecondStreet reported that over 3.2 million Canadians are still waiting to receive basic healthcare, including surgeries, diagnostic scans and appointments with specialists.
“Despite record health spending by provincial governments to reduce wait times, improvements to waiting lists have been quite sluggish,” said Harrison Fleming, Legislative and Policy Director at SecondStreet.org.
“With more than three million Canadians waiting today – nearly the same number since Canada came out of the pandemic – it’s clear that throwing money at the problem isn’t the answer,” he continued. “Copying policies that work well in universal systems in Europe could help.”
SecondStreet further revealed that their data is incomplete since neither Yukon or Prince Edward Island provided data, meaning the actual number of Canadians awaiting health care is likely closer to 5.1 million patients, or about one in eight Canadians.
According to the data, wait times in Saskatchewan have improved since the “pandemic” as both the number of patients waiting for surgery and diagnostic scans have dropped 22% and 11% respectively.
In Ontario, residents saw surgical waitlist volumes decrease 19%, while diagnostic waitlist volumes rose 32%.
Quebec’s numbers saw a greater improvement, as the province witnessed a 42% decrease in diagnostic waitlist volumes while only a 4% increase in surgical waitlist numbers.
The Maritime provinces provided little to no data, with New Brunswick only reporting a 2% increase in surgery wait times and Newfoundland reporting a 31% drop in diagnostic waitlists. Similarly, Nova Scotia saw a 33.5% drop in those waiting for surgery.
At the same time, British Columbia’s surgical waitlist volume has increased 10%, while 204,737 patients are on waitlists for MRIs, CT Scans, colonoscopies, and other GI endoscopies.
Additionally, Alberta’s surgical and diagnostic waitlists increased 4% and 3% respectively, leaving nearly 200,000 patients waiting for surgical and diagnostic care. However, the province explained that their new data drew from a larger pool of health providers than previously provided.
Finally, in Manitoba, the number of people waiting for surgery and to receive a diagnostic scan increased over 16% to a total of 76,021.
The continued problem with long waits for care comes after years of reports that the medical systems of Canadian provinces are woefully understaffed compared to the population. In May, data revealed that Ontario will need 33,200 more nurses and 50,853 more personal support workers by 2032 to fill the ongoing shortages, figures Premier Doug Ford’s government had asked the Information and Privacy Commissioner to keep secret.
Many have pointed to the fact that the crisis was exacerbated when provinces began levying COVID vaccine mandates as a condition of employment for healthcare workers. While the official number of nurses and other workers relieved of their duties for refusing to take the experimental injections remains uncertain, Raphael Gomez, director of the Centre for Industrial Relations and Human Relations at the University of Toronto, told CTV News that as many as 10 percent of nurses in Ontario, the nation’s most populous province, either quit or retired early as a result of the mandates.
Officials tried to justify the mandates by claiming that the unvaccinated were “unprotected” from COVID while the vaccinated were believed to have immunity from the virus. However, there is overwhelming evidence that the COVID vaccine does not prevent transmission and can also cause a plethora of negative side effects.
Similarly, in February, Health Canada revealed that Canada was short 89,995 doctors, nurses and other front line health care workers, which is double the rate from 2020 before COVID vaccine mandates were imposed.
Currently, wait times to receive care in Canada have increased to an average of 27.7 weeks, leading some Canadians to despair and opt for euthanasia instead of waiting for assistance. At the same time, sick and elderly Canadians who have refused to end their lives via MAiD have reported being called “selfish” by their providers.
COVID-19
FDA requires new warning on mRNA COVID shots due to heart damage in young men

From LifeSiteNews
Pfizer and Moderna’s mRNA COVID shots must now include warnings that they cause ‘extremely high risk’ of heart inflammation and irreversible damage in males up to age 24.
The Trump administration’s Food and Drug Administration (FDA) announced it will now require updated safety warnings on mRNA COVID-19 shots to include the “extremely high risk” of myocarditis/pericarditis and the likelihood of long-term, irreversible heart damage for teen boys and young men up to age 24.
The required safety updates apply to Comirnaty, the mRNA COVID shot manufactured by Pfizer Inc., and Spikevax, the mRNA COVID shot manufactured ModernaTX, Inc.
According to a press release, the FDA now requires each of those manufacturers to update the warning about the risks of myocarditis and pericarditis to include information about:
- the estimated unadjusted incidence of myocarditis and/or pericarditis following administration of the 2023-2024 Formula of mRNA COVID-19 shots and
- the results of a study that collected information on cardiac magnetic resonance imaging (cardiac MRI) in people who developed myocarditis after receiving an mRNA COVID-19 injection.
The FDA has also required the manufacturers to describe the new safety information in the adverse reactions section of the prescribing information and in the information for recipients and caregivers.
Additionally, the fact sheets for healthcare providers and for recipients and caregivers for Moderna COVID-19 shot and Pfizer-BioNTech COVID-19 shot, which are authorized for emergency use in individuals 6 months through 11 years of age, have also been updated to include the new safety information in alignment with the Comirnaty and Spikevax prescribing information and information for recipients and caregivers.
In a video published on social media, Dr. Vinay Prasad, director of the Center for Biologics Evaluation & Research Chief Medical and Scientific Officer, explained the alarming reasons for the warning updates.
While heart problems arose in approximately 8 out of 1 million persons ages 6 months to 64 years following reception of the cited shots, that number more than triples to 27 per million for males ages 12 to 24.
Prasad noted that multiple studies have arrived at similar findings.
Business
National dental program likely more costly than advertised

From the Fraser Institute
By Matthew Lau
At the beginning of June, the Canadian Dental Care Plan expanded to include all eligible adults. To be eligible, you must: not have access to dental insurance, have filed your 2024 tax return in Canada, have an adjusted family net income under $90,000, and be a Canadian resident for tax purposes.
As a result, millions more Canadians will be able to access certain dental services at reduced—or no—out-of-pocket costs, as government shoves the costs onto the backs of taxpayers. The first half of the proposition, accessing services at reduced or no out-of-pocket costs, is always popular; the second half, paying higher taxes, is less so.
A Leger poll conducted in 2022 found 72 per cent of Canadians supported a national dental program for Canadians with family incomes up to $90,000—but when asked whether they would support the program if it’s paid for by an increase in the sales tax, support fell to 42 per cent. The taxpayer burden is considerable; when first announced two years ago, the estimated price tag was $13 billion over five years, and then $4.4 billion ongoing.
Already, there are signs the final cost to taxpayers will far exceed these estimates. Dr. Maneesh Jain, the immediate past-president of the Ontario Dental Association, has pointed out that according to Health Canada the average patient saved more than $850 in out-of-pocket costs in the program’s first year. However, the Trudeau government’s initial projections in the 2023 federal budget amounted to $280 per eligible Canadian per year.
Not all eligible Canadians will necessarily access dental services every year, but the massive gap between $850 and $280 suggests the initial price tag may well have understated taxpayer costs—a habit of the federal government, which over the past decade has routinely spent above its initial projections and consistently revises its spending estimates higher with each fiscal update.
To make matters worse there are also significant administrative costs. According to a story in Canadian Affairs, “Dental associations across Canada are flagging concerns with the plan’s structure and sustainability. They say the Canadian Dental Care Plan imposes significant administrative burdens on dentists, and that the majority of eligible patients are being denied care for complex dental treatments.”
Determining eligibility and coverage is a huge burden. Canadians must first apply through the government portal, then wait weeks for Sun Life (the insurer selected by the federal government) to confirm their eligibility and coverage. Unless dentists refuse to provide treatment until they have that confirmation, they or their staff must sometimes chase down patients after the fact for any co-pay or fees not covered.
Moreover, family income determines coverage eligibility, but even if patients are enrolled in the government program, dentists may not be able to access this information quickly. This leaves dentists in what Dr. Hans Herchen, president of the Alberta Dental Association, describes as the “very awkward spot” of having to verify their patients’ family income.
Dentists must also try to explain the program, which features high rejection rates, to patients. According to Dr. Anita Gartner, president of the British Columbia Dental Association, more than half of applications for complex treatment are rejected without explanation. This reduces trust in the government program.
Finally, the program creates “moral hazard” where people are encouraged to take riskier behaviour because they do not bear the full costs. For example, while we can significantly curtail tooth decay by diligent toothbrushing and flossing, people might be encouraged to neglect these activities if their dental services are paid by taxpayers instead of out-of-pocket. It’s a principle of basic economics that socializing costs will encourage people to incur higher costs than is really appropriate (see Canada’s health-care system).
At a projected ongoing cost of $4.4 billion to taxpayers, the newly expanded national dental program is already not cheap. Alas, not only may the true taxpayer cost be much higher than this initial projection, but like many other government initiatives, the dental program already seems to be more costly than initially advertised.
-

 Alberta11 hours ago
Alberta11 hours agoCOWBOY UP! Pierre Poilievre Promises to Fight for Oil and Gas, a Stronger Military and the Interests of Western Canada
-
 Alberta1 day ago
Alberta1 day agoAlberta Next: Immigration
-
 Alberta11 hours ago
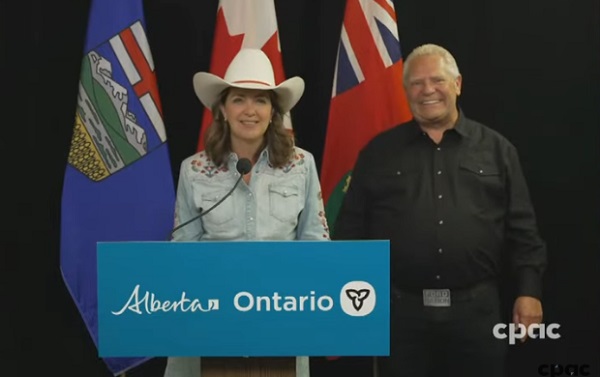
Alberta11 hours agoAlberta and Ontario sign agreements to drive oil and gas pipelines, energy corridors, and repeal investment blocking federal policies
-

 Business2 days ago
Business2 days agoThe Digital Services Tax Q&A: “It was going to be complicated and messy”
-

 International2 days ago
International2 days agoElon Musk forms America Party after split with Trump
-

 COVID-1915 hours ago
COVID-1915 hours agoFDA requires new warning on mRNA COVID shots due to heart damage in young men
-

 Alberta Sports Hall of Fame and Museum1 day ago
Alberta Sports Hall of Fame and Museum1 day agoAlberta Sports Hall of Fame 2025 Inductee Profiles – Para Nordic Skiing – Brian and Robin McKeever
-

 Indigenous13 hours ago
Indigenous13 hours agoInternal emails show Canadian gov’t doubted ‘mass graves’ narrative but went along with it