Health
1,000 UK doctors condemn medical association’s push to lift puberty blocker ban for minors

From LifeSiteNews
1,000 senior doctors signed an open letter to the British Medical Association after it lobbied for the NHS to lift a ban on puberty blockers for children following the Cass Review, which found the drugs were harmful.
On August 1, the British Medical Association (BMA) – the United Kingdom’s doctors’ union – called on the government to lift the ban on puberty blockers for minors. Weirdly, the BMA also stated that in their view the implementation of NHS England’s Cass Review should be “paused” despite the fact that, as the BBC noted, the review “took four years to carry out and was widely welcomed by the medical establishment in the U.K.” The BMA called the Cass Review’s recommendations – based on “the largest and most comprehensive review” on the subject seen, looking at 237 papers from 18 countries – “unsubstantiated.”
A spokesperson for the Department of Health and Social Care responded to the BMA, firmly rejecting both the request and the claim, stating, “The Cass Review is a robust report backed by clinicians and firmly grounded in evidence. NHS England will be implementing Dr. Cass’s recommendations so that children and young people get the safe, holistic support they need. We do not support a delay to vital improvements from the NHS to gender services.” Even the leftist Guardian ran an editorial criticizing the BMA’s position, stating, “The BMA’s stance on puberty blockers defies the key principle of medicine: first, do no harm.”
READ: FDA official recommends approval of puberty blockers despite suicide risk for gender-confused youth
As it turns out, there are plenty of physicians who are very unhappy with the BMA’s move – and they are now making their voices heard. This week, 1,000 senior doctors from across the U.K. published an open letter addressed to Professor Philip Banfield, chairman of the BMA.
“We write as doctors to say, ‘not in my name,’” the letter reads. “We are extremely disappointed that the BMA council had passed a motion to conduct a ‘critique’ of the Cass Review and to lobby to oppose its recommendations. The passing of the motion was opaque and secretive. It does not reflect the views of the wider membership, whose opinion you did not seek. We understand that no information will be released on the voting figures and how council members voted. That is a failure of accountability to members and is simply not acceptable.”
The open letter further emphasizes that the Cass Review “is the most comprehensive review into healthcare for children with gender related distress ever conducted” and urged the BMA to “abandon its pointless exercise” of attacking and opposing the recommendations. “By lobbying against the best evidence we have, the BMA is going against the principles of evidence-based medicine and against ethical practice.”
Among the signatories to the letter are 23 former or current clinical leaders at royal colleges, as well as the heads and former heads of some royal colleges.
The British Medical Association is the only main medical organization to oppose the Cass Review; all others have backed it. For example, Professor Sir Stephen Powis, NHS national medical director, stated, “These plans set out in detail how we will establish a fundamentally different and safer model of care for children and young people. The work Dr. Cass has undertaken has been invaluable in helping us shape the new service offer, and we have already begun our transformation of these services by opening two new regional centres this year.” Banfield responded on behalf of the BMA council to say that the points made in the letter would be considered during their ongoing evaluation.
As Josephine Bartosch observed, “it is becoming increasingly clear that the BMA is dangerously out of step with the medical consensus. The Cass Review has sent ripples across the world, and from lawsuits in the U.S. to a change of tack across Europe – medics are increasingly acknowledging that what is a crisis in youth mental health cannot be cured by changing bodies.”
Business
RFK Jr. says Hep B vaccine is linked to 1,135% higher autism rate

From LifeSiteNews
By Matt Lamb
They got rid of all the older children essentially and just had younger children who were too young to be diagnosed and they stratified that, stratified the data
The Centers for Disease Control and Prevention (CDC) found newborn babies who received the Hepatitis B vaccine had 1,135-percent higher autism rates than those who did not or received it later in life, Robert F. Kennedy Jr. told Tucker Carlson recently. However, the CDC practiced “trickery” in its studies on autism so as not to implicate vaccines, Kennedy said.
RFK Jr., who is the current Secretary of Health and Human Services, said the CDC buried the results by manipulating the data. Kennedy has pledged to find the causes of autism, with a particular focus on the role vaccines may play in the rise in rates in the past decades.
The Hepatitis B shot is required by nearly every state in the U.S. for children to attend school, day care, or both. The CDC recommends the jab for all babies at birth, regardless of whether their mother has Hep B, which is easily diagnosable and commonly spread through sexual activity, piercings, and tattoos.
“They kept the study secret and then they manipulated it through five different iterations to try to bury the link and we know how they did it – they got rid of all the older children essentially and just had younger children who were too young to be diagnosed and they stratified that, stratified the data,” Kennedy told Carlson for an episode of the commentator’s podcast. “And they did a lot of other tricks and all of those studies were the subject of those kind of that kind of trickery.”
But now, Kennedy said, the CDC will be conducting real and honest scientific research that follows the highest standards of evidence.
“We’re going to do real science,” Kennedy said. “We’re going to make the databases public for the first time.”
He said the CDC will be compiling records from variety of sources to allow researchers to do better studies on vaccines.
“We’re going to make this data available for independent scientists so everybody can look at it,” the HHS secretary said.
— Matt Lamb (@MattLamb22) July 1, 2025
Health and Human Services also said it has put out grant requests for scientists who want to study the issue further.
Kennedy reiterated that by September there will be some initial insights and further information will come within the next six months.
Carlson asked if the answers would “differ from status quo kind of thinking.”
“I think they will,” Kennedy said. He continued on to say that people “need to stop trusting the experts.”
“We were told at the beginning of COVID ‘don’t look at any data yourself, don’t do any investigation yourself, just trust the experts,”‘ he said.
In a democracy, Kennedy said, we have the “obligation” to “do our own research.”
“That’s the way it should be done,” Kennedy said.
He also reiterated that HHS will return to “gold standard science” and publish the results so everyone can review them.
International
RFK Jr. tells Tucker how Big Pharma uses ‘perverse incentives’ to get vaccines approved
From LifeSiteNews
By Matt Lamb
Kennedy defended his decision to fire all 17 members of the Advisory Committee on Immunization Practices, which he decried as a tool used to “rubber stamp” vaccines.
The vaccine approval process is a “bundle of perverse incentives” since pharmaceutical companies stand to make billions of dollars in revenue from it, Secretary of Health and Human Services Robert F. Kennedy Jr. told Tucker Carlson recently.
Kennedy appeared on Carlson’s show yesterday to discuss a variety of issues, including the potential link between autism and vaccines and his overhauling of the vaccine advisory committee at the Centers for Disease Control and Prevention last month.
Twenty years ago, Bobby Kennedy was exiled from polite society for suggesting a link between autism and vaccines. Now he’s a cabinet secretary, and still saying it.
(0:00) The Organized Opposition to RFK’s Mission
(6:46) Uncovering the Reason for Skyrocketing Rates of Autism… pic.twitter.com/g8T8te3kNC— Tucker Carlson (@TuckerCarlson) June 30, 2025
Kennedy began by explaining that Big Pharma has been targeting academic journals to ensure its products receive favorable reviews.
“The journals won’t publish anything critical of vaccines … there’s so much pressure on them. They’re funded by pharmaceutical companies, and they’ll lose advertising and revenue from reprints,” Kennedy said.
Kennedy then noted that Big Pharma will “pay to get something published in these journals,” before accusing industry leaders of pushing drugs on doctors and of hiring “mercenary scientists” to manipulate data until their product is deemed safe and effective.
The entire complex is broken due to the “perverse incentives,” he lamented.
Later in the interview, Kennedy defended his decision to fire all 17 members of the Advisory Committee on Immunization Practices (ACIP) in June, which he decried as a mere tool to “rubber stamp” vaccines.
It served as “a sock puppet for the industry that it was supposed to regulate,” Kennedy exclaimed, citing conflicts of interest for the overwhelming majority of its board members.
This sort of “agency capture” explains the lucrative nature of vaccines, he added.
— Matt Lamb (@MattLamb22) July 1, 2025
Kennedy then summarized the “perverse” process as follows:
First of all, the federal government often times actually designs the vaccine, [the National Institutes of Health] would design it, would hand it over to the pharmaceutical company. The pharmaceutical company then runs it … first through [the] FDA, then through [the] ACIP, and gets it recommended.
If you can get that recommendation you now got a billion dollars in — at least — revenues by the end of the year, every year, forever. So, there was a gold rush to add new vaccines to the schedule and ACIP never turned away a single vaccine … that came to them they recommended, and a lot of these vaccines are for diseases that are not even casually contagious.
Kennedy further pointed to the Hepatitis B shot for newborns as an example of how the industry has been corrupted.
In 1999, the CDC “looked at children who had received the hepatitis vaccine within the first 30 days of life and compared those children to children who had received the vaccine later — or not at all. And they found an 1,135% elevated risk of autism among the vaccinated children. It shocked them. They kept the study secret and manipulated it through five different iterations to try to bury the link,” he said.
“We want to protect public health,” Kennedy explained, but “these vaccines … can cause chronic disease, chronic injuries that last a lifetime.”
-

 Business1 day ago
Business1 day agoRFK Jr. says Hep B vaccine is linked to 1,135% higher autism rate
-
 Crime2 days ago
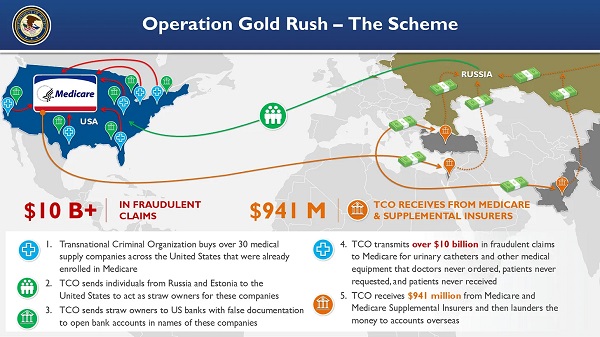
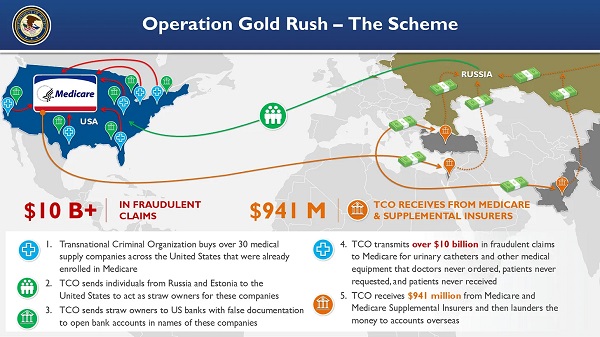
Crime2 days agoNational Health Care Fraud Takedown Results in 324 Defendants Charged in Connection with Over $14.6 Billion in Alleged Fraud
-

 Business15 hours ago
Business15 hours agoWhy it’s time to repeal the oil tanker ban on B.C.’s north coast
-

 Censorship Industrial Complex1 day ago
Censorship Industrial Complex1 day agoGlobal media alliance colluded with foreign nations to crush free speech in America: House report
-
 Alberta10 hours ago
Alberta10 hours agoAlberta Provincial Police – New chief of Independent Agency Police Service
-

 Health2 days ago
Health2 days agoRFK Jr. Unloads Disturbing Vaccine Secrets on Tucker—And Surprises Everyone on Trump
-

 Alberta15 hours ago
Alberta15 hours agoPierre Poilievre – Per Capita, Hardisty, Alberta Is the Most Important Little Town In Canada
-

 Opinion7 hours ago
Opinion7 hours agoBlind to the Left: Canada’s Counter-Extremism Failure Leaves Neo-Marxist and Islamist Threats Unchecked